- Geisel School of Medicine at Dartmouth, Hanover,
- Department of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, USA.
Correspondence Address:
David F. Bauer
Geisel School of Medicine at Dartmouth, Hanover,
Department of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, USA.
DOI:10.25259/SNI-305-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Christopher E. Louie, Jennifer Hong, David F. Bauer. Surgical management of Bertolotti’s syndrome in two adolescents and literature review. 05-Jul-2019;10:135
How to cite this URL: Christopher E. Louie, Jennifer Hong, David F. Bauer. Surgical management of Bertolotti’s syndrome in two adolescents and literature review. 05-Jul-2019;10:135. Available from: http://surgicalneurologyint.com/surgicalint-articles/9460/
Abstract
Background: Bertolotti’s syndrome is defined by back pain and/or radicular symptoms attributed to a congenital lumbosacral transitional vertebra (LSTV). There are few studies that discuss the surgical management of Bertolotti’s syndrome. Here, we report long-term outcomes after resecting a pseudoarthrosis between the sacrum and L5 in two teenage patients, along with a review of literature.
Case Descriptions: Surgical resection of a lumbosacral bridging articulation (LSTV type IIa) was performed in two patients, 15 and 16 years of age who presented with intractable back pain. The adequacy of surgery was confirmed with postoperative studies. In both patients, pain and functional status improved within 6 weeks and have remained improved at last follow-up.
Conclusion: Surgical removal of a pathologic L5 transverse process fused to the sacral ala in two young patients with Bertolotti’s syndrome improved postoperative pain and increased overall function. Given the progressive nature of Bertolotti’s syndrome, surgical intervention in young patients should be considered to mitigate years of chronic pain and attendant morbidity.
Keywords: Bertolotti’s syndrome, Lumbosacral transitional vertebrae, Sacralized pseudoarthrosis
INTRODUCTION
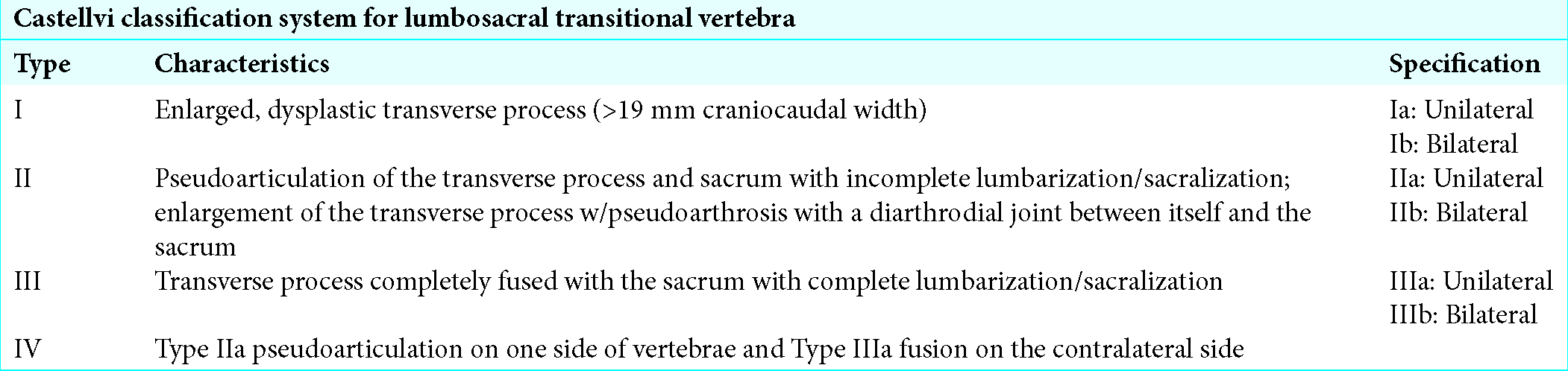
Bertolotti’s syndrome is defined as a congenital lumbosacral transitional vertebra (LSTV) that is responsible for disabling low back pain. It most commonly occurs at the L5 level, followed by the L6 level, and is characterized by various morphologic presentations [
CLINICAL PRESENTATION
Patient 1
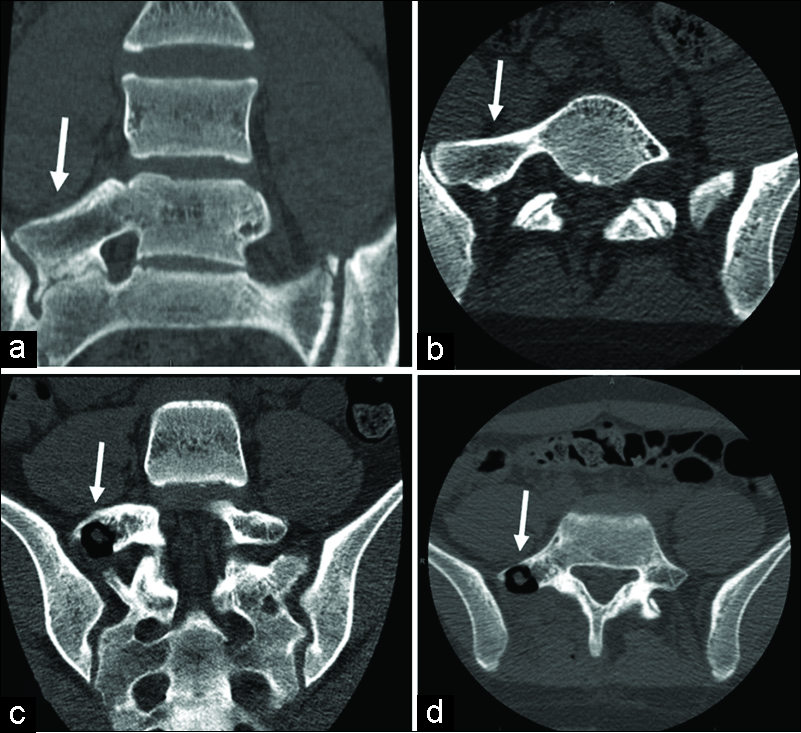
A 14-year-old female with midline low back pain and the right hip/leg pain was treated for 9 months with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs) without relief. Her neurological examination was normal. Lumbar X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) studies showed Bertolotti’s syndrome, characterized by a right-sided partially sacralized L5 vertebra with pseudoarthrosis between L5 to S1 and ileum, with areas of irregularity/sclerosis [
Patient 2
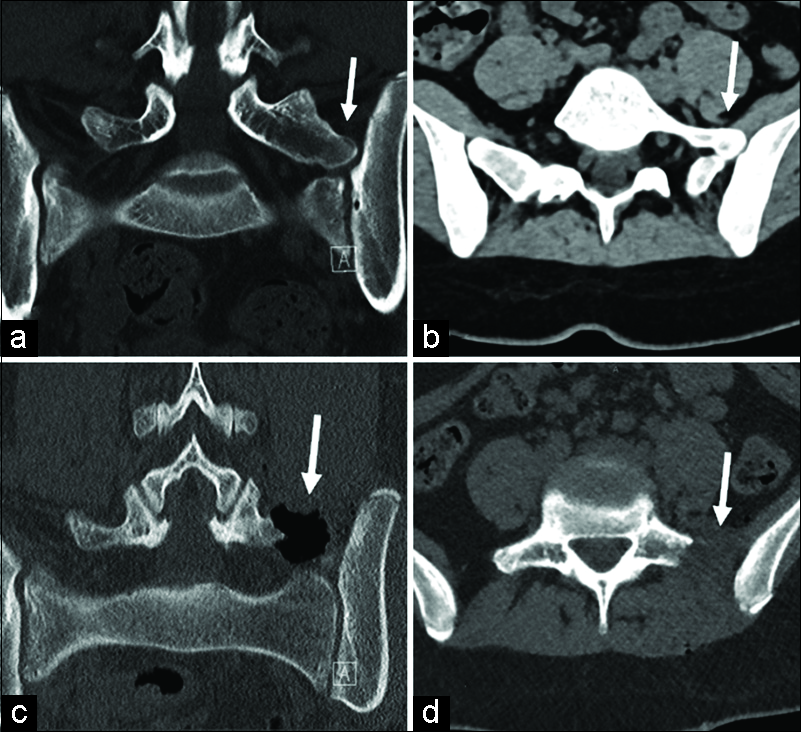
A 16-year-old female presented with 2 years of low back pain and 3 months of pain radiating into her left hip refractory to NSAIDs and physical therapy. Comorbidities included recurrent migraines, major depressive disorder, obstructive sleep apnea, and restless leg syndrome. Her neurological examination was normal. The lumbar CT and MRI studies showed Bertolotti’s syndrome on the left at the L5-S1 level characterized by an enlarged left L5 transverse process fused with the ilium and sacrum, with mild degeneration/sclerosis of the left L5 pars interarticularis [
DISCUSSION AND REVIEW OF RELEVANT LITERATURE
Diagnosis and pathophysiology of Bertolotti’s syndrome
Bertolotti’s syndrome is found in 10% of patients presenting with back and leg pain under 30 years of age.[
Radiographic analysis
Radiographs, including flexion, extension views, and oblique views, confirm the diagnosis of Bertolotti’s syndrome. Both CT and MRI also demonstrate Bertolotti’s syndrome and also readily identify associated stenosis, osteophytes, and sclerosis adjacent to the articulation between the lumbar segment and ilium and/or sacrum.
Management of Bertolotti’s syndrome
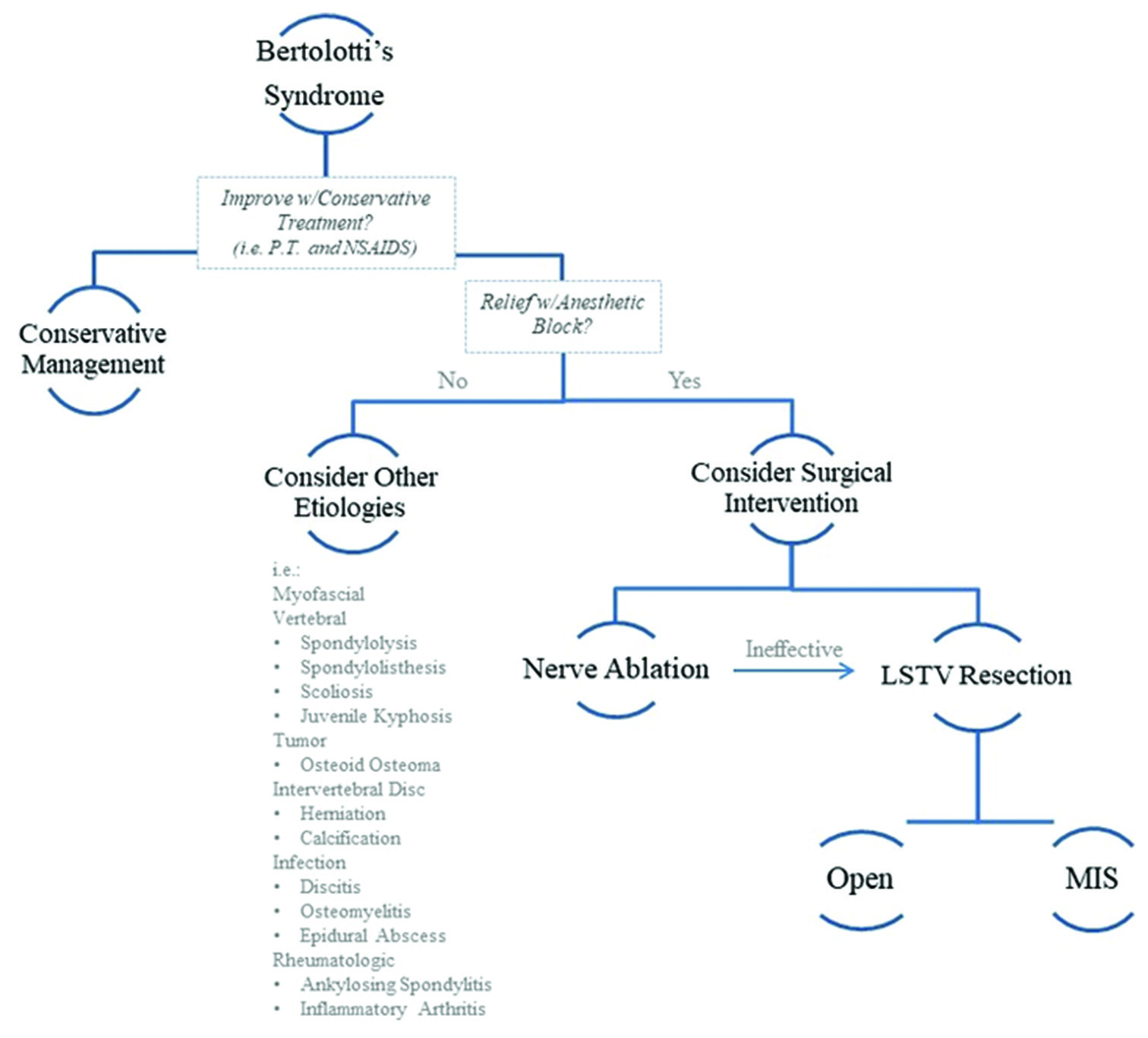
Surgical resection of LSTV should be considered in patients presenting with intractable low back pain despite conservative treatment (e.g., physical therapy, nonsteroidal anti-inflammatory drugs, and localized anesthetic blocks in adults
Outcomes of surgery with Bertolotti’s syndrome
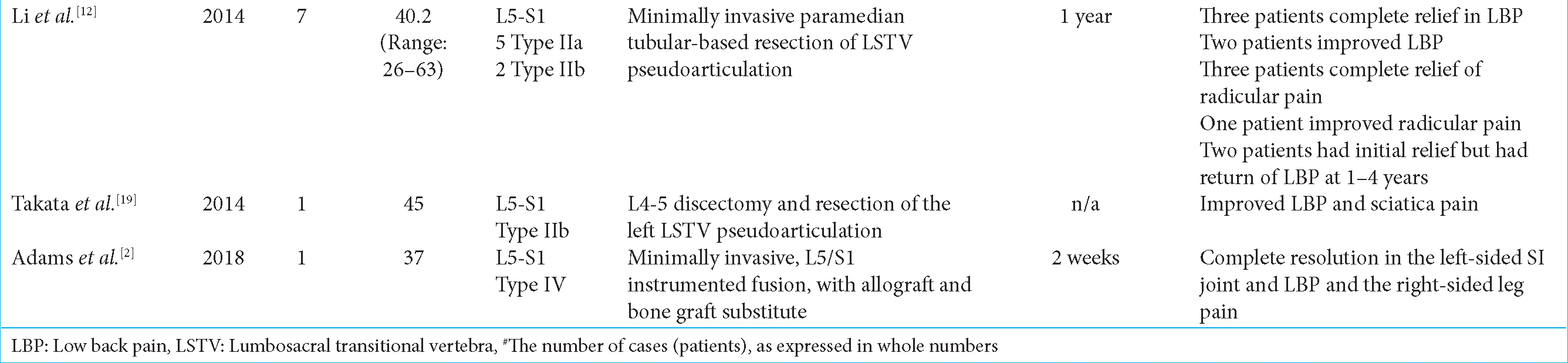
There are few reports for patients under 18 years of age treated for Bertolotti’s syndrome [
CONCLUSION
Bertolotti’s syndrome is seen in 10% of patients presenting with back and leg pain under 30 years of age.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given her consent for her images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
1. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997. 22: 823-6
2. Adams R, Herrera-Nicol S, Jenkins AL. Surgical treatment of a rare presentation of Bertolotti’s syndrome from castellvi Type IV lumbosacral transitional vertebra: Case report and review of the literature. J Neurol Surg Rep. 2018. 79: e70-e74
3. Babu H, Lagman C, Kim TT, Grode M, Johnson JP, Drazin D. Intraoperative navigation-guided resection of anomalous transverse processes in patients with Bertolotti’s syndrome. Surg Neurol Int. 2017. 8: 236-
4. Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine (Phila Pa 1976). 2001. 26: 226-9
5. Holm EK, Bünger C, Foldager CB. Symptomatic lumbosacral transitional vertebra: A review of the current literature and clinical outcomes following steroid injection or surgical intervention. SICOT J. 2017. 3: 71-
6. Ichihara K, Taguchi T, Hashida T, Ochi Y, Murakami T, Kawai S. The treatment of far-out foraminal stenosis below a lumbosacral transitional vertebra: A report of two cases. J Spinal Disord Tech. 2004. 17: 154-7
7. Jain A, Agarwal A, Jain S, Shamshery C. Bertolotti syndrome: A diagnostic and management dilemma for pain physicians. Korean J Pain. 2013. 26: 368-73
8. Jönsson B, Strömqvist B, Egund N. Anomalous lumbosacral articulations and low-back pain. Evaluation and treatment. Spine (Phila Pa 1976). 1989. 14: 831-4
9. Ju CI, Kim SW, Kim JG, Lee SM, Shin H, Lee HY. Decompressive L5 transverse processectomy for Bertolotti’s syndrome: A preliminary study. Pain Physician. 2017. 20: E923-E932
10. Kapetanakis S, Chaniotakis C, Paraskevopoulos C, Pavlidis P. An unusual case report of Bertolotti’s syndrome: Extraforaminal stenosis and L5 unilateral root compression (Castellvi type III an LSTV). J Orthop Case Rep. 2017. 7: 9-12
11. Kikuchi K, Abe E, Miyakoshi N, Kobayashi T, Abe T, Hongo M. Anterior decompression for far-out syndrome below a transitional vertebra: A report of two cases. Spine J. 2013. 13: e21-5
12. Li Y, Lubelski D, Abdullah KG, Mroz TE, Steinmetz MP. Minimally invasive tubular resection of the anomalous transverse process in patients with Bertolotti’s syndrome: Presented at the 2013 joint spine section meeting: Clinical article. J Neurosurg Spine. 2014. 20: 283-90
13. Malham GM, Limb RJ, Claydon MH, Brazenor GA. Anterior pseudoarthrectomy for symptomatic Bertolotti’s syndrome. J Clin Neurosci. 2013. 20: 1762-6
14. Manmohan S, Dzulkarnain A, Azlin ZA, Fazir M. Bertolotti’s syndrome: A commonly missed cause of back pain in young patients. Malays Fam Physician. 2015. 10: 55-8
15. Miyoshi Y, Yasuhara T, Date I. Posterior decompression of far-out foraminal stenosis caused by a lumbosacral transitional vertebra case report. Neurol Med Chir (Tokyo). 2011. 51: 153-6
16. Quinlan JF, Duke D, Eustace S. Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006. 88: 1183-6
17. Santavirta S, Tallroth K, Ylinen P, Suoranta H. Surgical treatment of Bertolotti’s syndrome. Follow-up of 16 patients. Arch Orthop Trauma Surg. 1993. 112: 82-7
18. Shibayama M, Ito F, Miura Y, Nakamura S, Ikeda S, Fujiwara K. Unsuspected reason for sciatica in Bertolotti’s syndrome. J Bone Joint Surg Br. 2011. 93: 705-7
19. Takata Y, Sakai T, Higashino K, Goda Y, Mineta K, Sugiura K. Minimally invasive microendoscopic resection of the transverse process for treatment of low back pain with Bertolotti’s syndrome. Case Rep Orthop. 2014. 2014: 613971-
20. Ugokwe KT, Chen TL, Klineberg E, Steinmetz MP. Minimally invasive surgical treatment of Bertolotti’s syndrome: Case report. Neurosurgery. 2008. 62: ONSE454-5
21. Weber J, Ernestus RI. Transitional lumbosacral segment with unilateral transverse process anomaly (Castellvi type 2A) resulting in extraforaminal impingement of the spinal nerve: A pathoanatomical study of four specimens and report of two clinical cases. Neurosurg Rev. 2010. 34: 143-50