- Department of Neurosurgery, Faculty of Medicine, São Paulo University, São Paulo, Brazil.
DOI:10.25259/SNI_206_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Adilson de Oliveira, Clarissa Nascimento, Diego Ramos, Hamilton Matushita. Surgical management of caudal duplication syndrome: A rare entity with a centered approach on quality of life. 20-Sep-2019;10:181
How to cite this URL: Adilson de Oliveira, Clarissa Nascimento, Diego Ramos, Hamilton Matushita. Surgical management of caudal duplication syndrome: A rare entity with a centered approach on quality of life. 20-Sep-2019;10:181. Available from: http://surgicalneurologyint.com/surgicalint-articles/9662/
Abstract
Background: Caudal duplication syndrome (CDS) is associated with complete/partial duplication of the spine, spinal cord, duplication/malformations of other caudal structures, and often neurological dysfunction.
Case Description: A 9-month-old with the prenatal diagnosis of multiple fetal malformations was born through cesarean section at 39 weeks. Computed tomography and magnetic resonance imaging revealed a series of abnormalities: intramedullary cyst at the L4 level with tethering of the conus with a lipoma, a duplication of the sacrum, duplication of the intestines, a ventricular septal defect, bladder duplication, four kidneys, two fully formed functional penises, two anuses (imperforate on the left), and a paramedian ossified appendage suggestive of a malformed leg. The child, at an 8 months of age, underwent a laminectomy at the L4 level for resection of the conus lipoma, release of the tethered cord, and resection of the intramedullary cyst.
Conclusion: Spine/spinal cord duplication syndromes are typically associated with spine/spinal cord abnormalities and are often associated with moderate/severe neurological deficits. Additional malformations associated with the CDS include duplication of vascular structures/organs (e.g., bladder and distal gastrointestinal tract). Here, we focused on both the patient’s quality of life and the multidisciplinary approach to managing the duplication syndrome associated with multiple system malformations (e.g., neurological/spinal, bladder, and gastrointestinal, others).
Keywords: Congenital malformation, Pediatric neurosurgery: Caudal duplication, Quality of life, Spine duplication
INTRODUCTION
The rare caudal duplication syndrome (CDS) includes a broad spectrum of anomalies involving the gastrointestinal, genitourinary, neurological, and vertebral skeletal systems. This entity was first described by Dominguez et al., in 1993; the prevalence is <1/100,000 births.[
CASE REPORT
Documentation of anomalies at birth
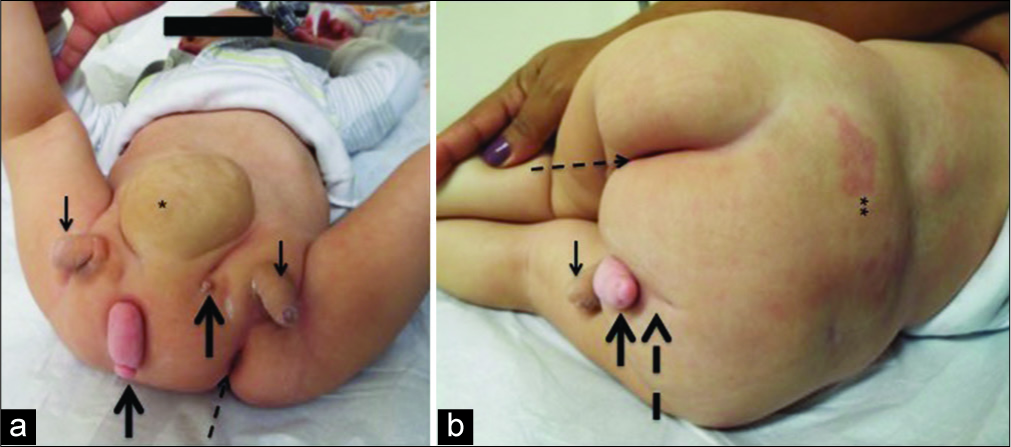
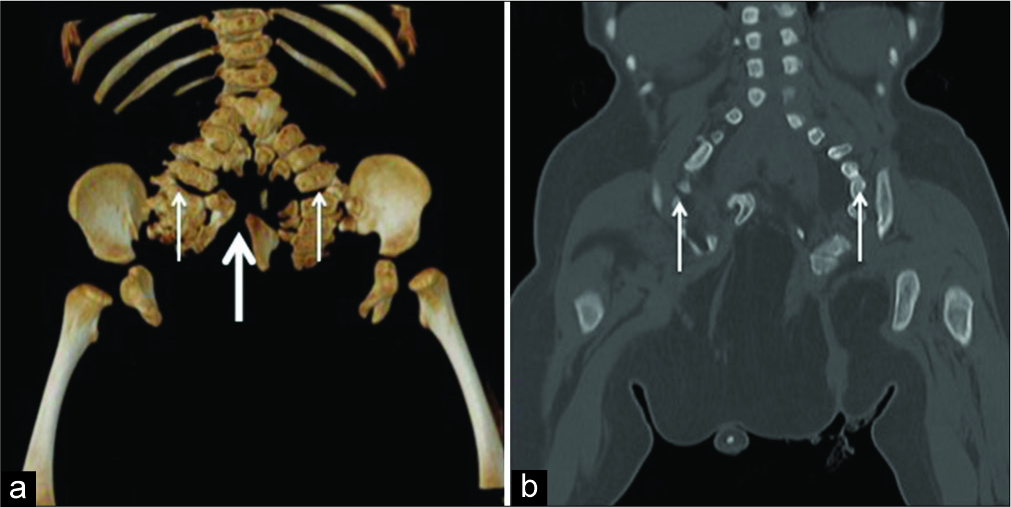
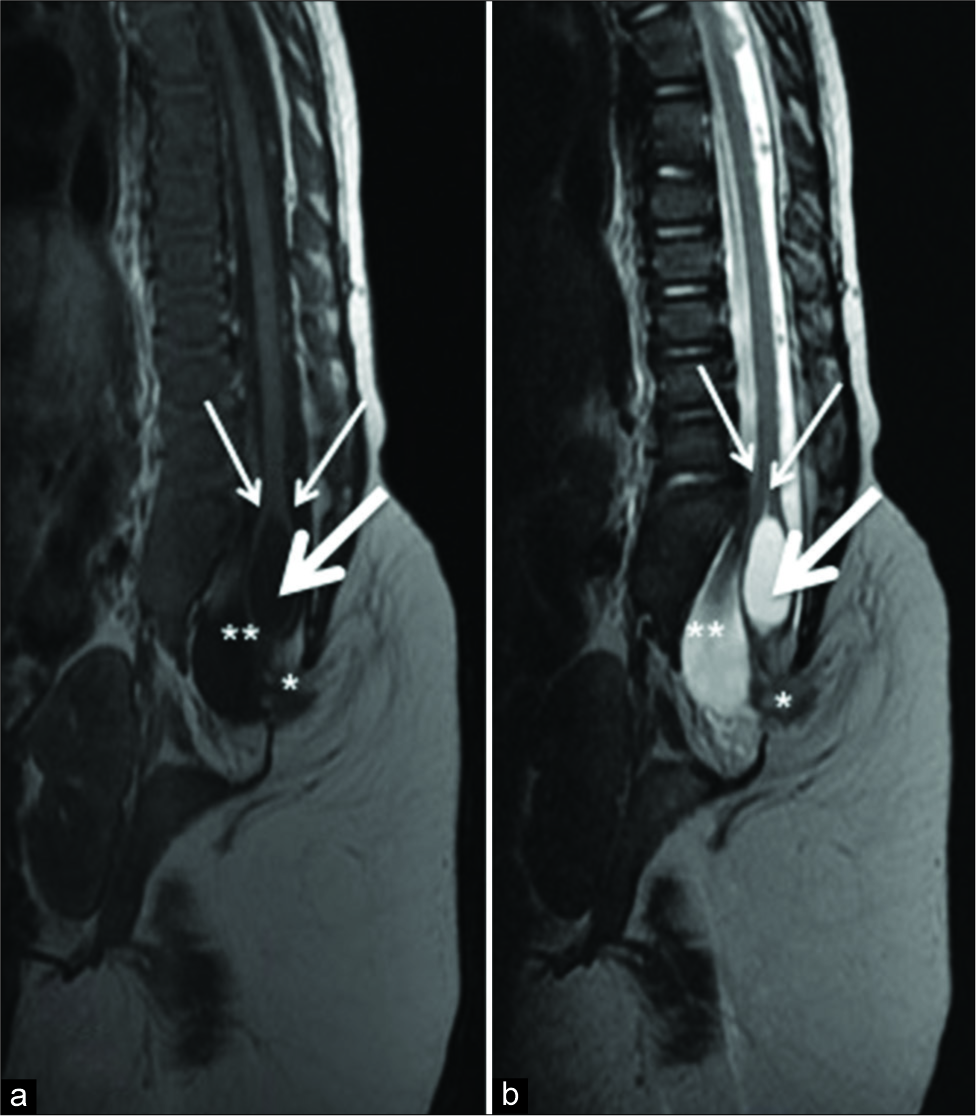
A 9 months old without a history of consanguinity or familial genetic diseases had the prenatal diagnosis of multiple fetal malformations established utilizing ultrasonography. Cesarean section delivery at 39 weeks prompted the performance of repeat ultrasonography followed by computed tomography and magnetic resonance imaging. These studies documented the following anomalies; intramedullary cyst at the L4 level with a tethered cord/lipoma, duplication of the sacrum, intestine, kidneys (e.g., 4 of these), bladder, two functional penises and anuses (one imperforate on the left) with enterovesical fistulas, and several cardiac defects (e.g., ventricular septal defect, interventricular communication, atrial septal defect, and persistent ductus arteriosus). In addition, there was a paramedian ossified appendage, suggestive of a malformed leg [
Surgery
A laparotomy was performed on the 5th day of life due to an acute abdomen; an enterovesical fistula was repaired. At 8 months, the patient underwent a laminectomy at L4 for untethering and resection of the lipoma and intramedullary cyst involving the conus. In the future, a multidisciplinary team will perform corrective surgery of the bones, genitalia, and urinary tracts (e.g., when child reaches the ages of 2–3 [presently 20 months old]). This will warrant; pelvic fusion, malformed leg amputation, amputation of one of the penises with urological and plastic surgery, and correction of the abdominal wall herniation.
DISCUSSION
The rare CDS, first described by Dominguez et al., in 1993, is defined as the association between malformations and duplications involving the gastrointestinal, genitourinary, and spine/spinal cord (e.g., neural tube defects).[
In our literature review, we did not find previous reports of patients who remained neurologically intact. Here, we used a multidisciplinary approach to ensure normal function in this 20-month-old patient with CDS. This first warranted emergently treating an enterovesical fistula at 5 days of age (acute abdomen) followed at 8 months by an L4 laminectomy for the treatment of a tethered cord/lipoma/intramedullary cyst. In other cases, those treated too aggressively sustained poor outcomes (e.g., including an adult with original normal neurological function but postoperative deterioration).[
CONCLUSION
Here, we report on a 9 months old with a CDS syndrome characterized by the duplication of multiple organ systems and neurological spine/spinal cord malformations. The acute abdomen due to an enterovesical fistula was treated 5 days after birth, and the patient underwent spine surgery at 9 months of age consisting of an L4 laminectomy to treat a tethered cord/lipoma and intramedullary cyst. Future operations are planned to address multiple additional duplications (e.g., at ages of 2–3).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, those responsible for the patient has/ have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. Those responsible for the patient understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dominguez R, Rott J, Castillo M, Pittaluga RR, Corriere JN Jr. Caudal duplication syndrome. Am J Dis Child. 1993. 147: 1048-52
2. Harris J, Blackwood B, Pillai S, Kanard R. Caudal duplication: Management of a rare congenital condition. Am Surg. 2016. 82: e227-9
3. Hu T, Browning T, Bishop K. Caudal duplication syndrome: Imaging evaluation of a rare entity in an adult patient. Radiol Case Rep. 2016. 11: 11-5
4. Mei JY, Nguyen MT, Raz S. Female caudal duplication syndrome: A surgical case report with 10-year follow-up and review of the literature. Female Pelvic Med Reconstr Surg. 2018. 24: e16-20
5. Pang D, Dias MS, Ahab-Barmada M. Split cord malformation: Part I: A unified theory of embryogenesis for double spinal cord malformations. Neurosurgery. 1992. 31: 451-80
6. Pang D. Split cord malformation: Part II: Clinical syndrome. Neurosurgery. 1992. 31: 481-500
7. Samuk I, Levitt M, Dlugy E, Kravarusic D, Ben-Meir D, Rajz G. Caudal duplication syndrome: The vital role of a multidisciplinary approach and staged correction. Euro J Pediatr Surg Rep. 2016. 4: 1-5