- Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
Correspondence Address:
Sajjad Muhammad
Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
DOI:10.4103/sni.sni_188_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Sajjad Muhammad, Mika Niemelä. Surgical management of coexisting trigeminal neuralgia and hemifacial spasm. 23-Oct-2018;9:214
How to cite this URL: Sajjad Muhammad, Mika Niemelä. Surgical management of coexisting trigeminal neuralgia and hemifacial spasm. 23-Oct-2018;9:214. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9049
Abstract
Background:Coexisting hemifacial spasm (HFS) and trigeminal neuralgia (TN) without any mass lesion in the posterior fossa is a rare condition. Hence, the surgical strategy of coexisting HFS and TN has rarely been discussed.
Case Description:We present a rare case of coexisting HFS and TN without any mass lesion in posterior fossa having microvascular confliction of trigeminal nerve with superior cerebellar artery (SCA) and facial nerve with anterior inferior cerebellar artery (AICA). Single surgery was performed for both trigeminal nerve and facial nerve. Mobilization of vessels and placement of Teflon between the nerve and vessel relieved the symptoms immediately after the operation. We have reviewed the literature for cases with coexistent HFS and TN. The treatment strategy for such cases has been discussed. The surgical treatment has been demonstrated with a video.
Conclusion:A single surgery is a safe and effective option to treat coexistent HFS and TN due to microvascular confliction.
Keywords: Combined hyperactive syndrome of cranial nerves, decompression surgery, hemifacial spasm, trigeminus neuralgia
INTRODUCTION
Combined hyperactive dysfunction syndrome (HDS) of cranial nerves is a rare condition. Taking all combined hyperactive cranial nerve syndromes together in about 3% of the cases more than one cranial nerve is involved.[
We report a rare case of coexisting HFS and TN, where two separate vessels compress two different nerves without any vertebrobasilar anomaly or other pathologies such as tumor, aneurysm, or AVM. A single surgery was performed that completely relieved both HFS and TN.
CASE HISTORY
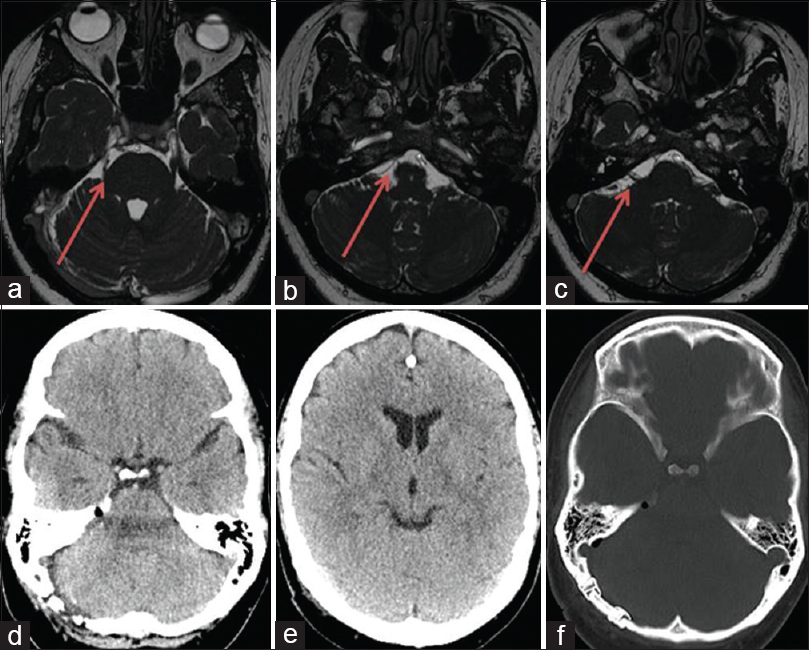
We present a case of 48-year-old female with two years history of right-sided TN in V2 and hemifacial spasm. The HFS was limited around the eye. The symptoms of electric pain in V2 were provoked by chewing, speaking, etc., reflecting the typical TN. After the failure of medical treatment, brain MRI scan was performed that showed no mass lesions. The MRI scan showed a clear conflict of SCA with TN and AICA with facial nerve [Figure
A literature review was performed using PubMed and Ovid Medline. We searched treatment options for cases with coexisting HFS and TN. Key words, “trigeminal neuralgia” and “hemifacial spasm” showed 320 published articles. Adding key word “microvascular decompression (MVD)” yielded 175 articles, 30 case reports, one clinical trial, and 24 review articles. After a critical review of these articles, 21 articles with coexisting HFS and TN treated surgically or with radiosurgery were considered relevant and had been discussed in the manuscript.
SURGICAL MICROVASCULAR DECOMPRESSION
Operative findings
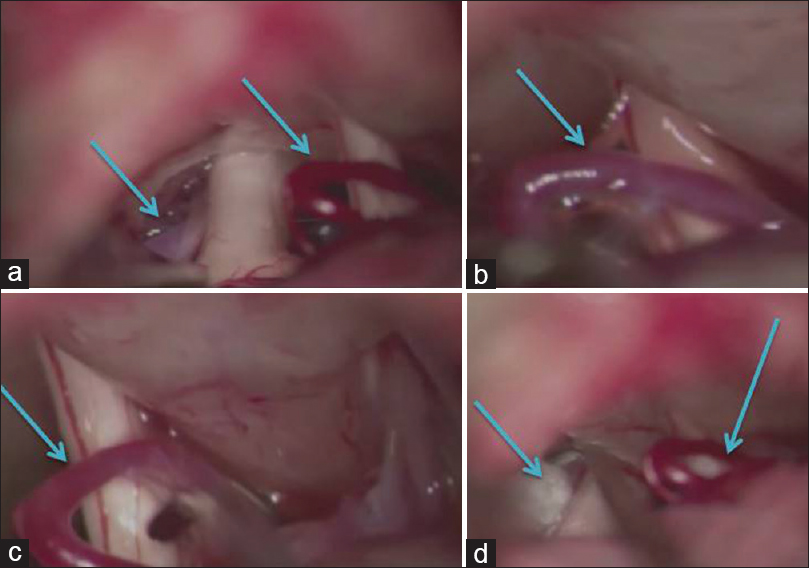
We planned to treat both pathologies in a single surgery. During surgery, normal cisternal anatomy was found. No obvious anatomical anomaly in the size of the posterior fossa. After opening the cisternmagna, we first identified TN and found an arterial confliction with branches of superior cerebellar artery [
Postoperative outcome
Postoperatively, both HFS as well the TN were completely resolved. Post operative CT scan showed no complications [Figure
DISCUSSION
The occurrence of TN, HFS, and glossopharyngeal neuralgia in combination is termed hyperactive dysfunction syndromes. The combination of HFS and TN also termed as painful tic convulsive is a rare condition.[
Case series from literature have reported an association with age and female sex.[
Microsurgical decompression in cases with combined HFS and TN has shown a satisfactory outcome that is comparable to the MVD in single nerve compression syndrome. Although gamma knife radiosurgery as an alternative option in concurrent HFS and TN due to vertebrobasilar, dolichoectasia has been reported.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the support from Ehrnrooth Foundation for the clinical fellowship to Dr. S. Muhammad.
References
1. Ballantyne ES, Page RD, Meaney JF, Nixon TE, Miles JB. Coexistent trigeminal neuralgia, hemifacial spasm, and hypertension: Preoperative imaging of neurovascular compression. Case report. J Neurosurg. 1994. 80: 559-63
2. Cao J, Jiao J, Du Z, Xu W, Sun B, Li F. Combined hyperactive dysfunction syndrome of the cranial nerves: A retrospective systematic study of clinical characteristics in 44 patients. World Neurosurg. 2017. 104: 390-7
3. Chan LL, Ng KM, Fook-Chong S, Lo YL, Tan EK. Three-dimensional MR volumetric analysis of the posterior fossa CSF space in hemifacial spasm. Neurology. 2009. 73: 1054-7
4. Desai K, Nadkarni T, Bhayani R, Goel A. Cerebellopontine angle epidermoid tumor presenting with ‘tic convulsif’ and tinnitus-case report. Neurol Med Chir (Tokyo). 2002. 42: 162-5
5. Dou NN, Hua XM, Zhong J, Li ST. A successful treatment of coexistent hemifacial spasm and trigeminal neuralgia caused by a huge cerebral arteriovenous malformation: A case report. J Craniofac Surg. 2014. 25: 907-10
6. Fukuda H, Ishikawa M, Okumura R. Demonstration of neurovascular compression in trigeminal neuralgia and hemifacial spasm with magnetic resonance imaging: Comparison with surgical findings in 60 consecutive cases. Surg Neurol. 2003. 59: 93-
7. Grigoryan YA, Dreval ON, Michailova SI. Painful tic convulsif caused by a contralateral vertebral artery. Surg Neurol. 1991. 35: 471-4
8. Hitotsumatsu T, Matsushima T, Inoue T. Microvascular decompression for treatment of trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia: Three surgical approach variations: Technical note. Neurosurgery. 2003. 53: 1436-
9. Jiao W, Zhong J, Sun H, Zhu J, Zhou QM, Yang XS. Microvascular decompression for the patient with painful tic convulsif after Bell palsy. J Craniofac Surg. 2013. 24: e286-9
10. Kobata H, Kondo A, Iwasaki K. Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002. 50: 276-
11. Kobata H, Kondo A, Iwasaki K, Nishioka T. Combined hyperactive dysfunction syndrome of the cranial nerves: Trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia: 11-year experience and review. Neurosurgery. 1998. 43: 1351-
12. Lakhan SE. Teaching NeuroImages: Concurrent hemifacial spasm and trigeminal neuralgia due to vertebrobasilar dolichoectasia. Neurology. 2013. 81: e52-
13. Liu J, Yuan Y, Zang L, Fang Y, Liu H, Yu Y. Hemifacial spasm and trigeminal neuralgia in Chiari's I malformation with hydrocephalus: Case report and literature review. Clin Neurol Neurosurg. 2014. 122: 64-7
14. Miyagi J, Hanabusa Y, Kuramoto S, Kuboyama M, Kajiwara K. Neurovascular decompression in trigeminal neuralgia associated with hemifacial spasm. Case report. Neurol Med Chir (Tokyo). 1986. 26: 900-3
15. Miyazono M, Inoue T, Matsushima T. A surgical case of hemifacial spasm caused by a tortuous, enlarged, and calcified vertebral artery. No Shinkei Geka. 2003. 31: 437-41
16. Revuelta-Gutierrez R, Velasco-Torres HS, Vales Hidalgo LO, Martinez-Anda JJ. Painful tic convulsif: Case series and literature review. Cir Cir. 2016. 84: 493-8
17. Romano-Feinholz S, Medina MP, Nares-Lopez FE, Soto-Hernandez JL, Revuelta-Gutierrez R. An unusual presentation of painful tic convulsive. Rev Neurol. 2017. 64: 264-6
18. Shinoda S, Kusama R, Chou H, Mori S, Masuzawa T. A case of painful tic convulsif due to cerebellopontine angle epidermoid tumor which could not be clearly detected by MRI. No Shinkei Geka. 1995. 23: 599-602
19. Son BC, Kim DR, Sung JH, Lee SW. Painful tic convulsif caused by an arteriovenous malformation. Clin Neuroradiol. 2012. 22: 365-9
20. Verghese J, Mahore A, Goel A. Arachnoid cyst associated with painful tic convulsif. J Clin Neurosci. 2012. 19: 763-4
21. Yang KH, Na JH, Kong DS, Park K. Combined hyperactive dysfunction syndrome of the cranial nerves. J Korean Neurosurg Soc. 2009. 46: 351-4
22. Zhang LW, Zhang Y, Zhu SG. Four patients with painful tic convulsive and a brief review of surgical treatment. J Clin Neurosci. 2012. 19: 740-2
23. Zhong J, Zhu J, Li ST, Guan HX. Microvascular decompressions in patients with coexistent hemifacial spasm and trigeminal neuralgia. Neurosurgery. 2011. 68: 916-20