- Madaktari Africa, Lynchburg, VA, USA
- Department of Neurological Surgery, University of California at San Francisco, San Francisco, CA, USA
- Division of Hospital Medicine, University of California at San Francisco, San Francisco, CA, USA
- Department of Neurological Surgery, Northwestern University, Chicago, IL, USA
Correspondence Address:
Michel Kliot
Department of Neurological Surgery, University of California at San Francisco, San Francisco, CA, USA
Department of Neurological Surgery, Northwestern University, Chicago, IL, USA
DOI:10.4103/2152-7806.169538
Copyright: © 2015 Kliot T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Kliot T, Zygourakis CC, Imershein S, Lau C, Kliot M. The impact of a patient education bundle on neurosurgery patient satisfaction. Surg Neurol Int 16-Nov-2015;6:
How to cite this URL: Kliot T, Zygourakis CC, Imershein S, Lau C, Kliot M. The impact of a patient education bundle on neurosurgery patient satisfaction. Surg Neurol Int 16-Nov-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/the-impact-of-a-patient-education-bundle-on-neurosurgery-patient/
Abstract
Background:As reimbursements and hospital/physician performance become ever more reliant on Hospital Consumer Assessment of Health Care Providers and Systems (HCAHPS) and other quality metrics, physicians are increasingly incentivized to improve patient satisfaction.
Methods:A faculty and resident team at the University of California, San Francisco (UCSF) Department of Neurological Surgery developed and implemented a Patient Education Bundle. This consisted of two parts: The first was preoperative expectation letters (designed to inform patients of what to expect before, during, and after their hospitalization for a neurosurgical procedure); the second was a trifold brochure with names, photographs, and specialty/training information about the attending surgeons, resident physicians, and nurse practitioners on the neurosurgical service. We assessed patient satisfaction, as measured by HCAHPS scores and a brief survey tailored to our specific intervention, both before and after our Patient Education Bundle intervention.
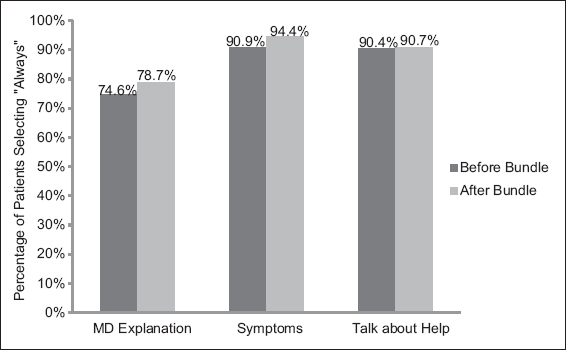
Results:Prior to our intervention, 74.6% of patients responded that the MD always explained information in a way that was easy to understand. After our intervention, 78.7% of patients responded that the MD always explained information in a way that was easy to understand. "Neurosurgery Patient Satisfaction survey" results showed that 83% remembered receiving the preoperative letter; of those received the letter, 93% found the letter helpful; and 100% thought that the letter should be continued.
Conclusion:Although effects were modest, we believe that patient education strategies, as modeled in our bundle, can improve patients' hospital experiences and have a positive impact on physician performance scores and hospital ratings.
Keywords: Hospital Consumer Assessment of Health Care Providers and Systems neurosurgery, patient satisfaction, patient education, quality improvement
EDITOR'S NOTE
It is no longer enough to be a clinically competent doctor. Physicians are expected to be clinically profiicent as well as are being graded and even rewarded for also being kind, considerate, compassionate, timely, responsive, and apologetic when appropriate. The following article provides a template for a letter that physicians at University of California, San Francisco (UCSF) send to their clinic patients prior to a hospital admission for surgery. The letter's goal is to inform patients as to what to expect in terms of who, how, and when they will be treated. In addition to being informative, it is also meant to set realistic expectations that hopefully can be met. This article also shows the utility of providing patients with a photo brochure of their medical team so that they can know and track who is actually taking care of them. Not only do these interventions make sense, but data on patient satisfaction before and after implementation is presented that suggests that patients actually appreciate and benefit from these efforts. This article showcases how physicians can humanize interactions with their patients with simple, considerate actions that can serve as an antidote to the depersonalization of medicine engendered by financial imperatives pressuring physicians to see more patients in a more timely and efficient manner while paying homage to the electronic medical record.
INTRODUCTION
Although a national program to measure hospital quality was initiated by the Joint Commission in 1998,[
In addition to its effect on reimbursement, patient satisfaction may also be a marker of clinical quality and patient-centered approaches. In a study of 2429 patients discharged from hospitals across the U.S., Jha et al. showed that higher HCAHPS scores were associated with better clinical quality, as measured by the Health Quality Alliance (HQA) scores for treatment of “acute myocardial infarction, congestive heart failure, and pneumonia – with respect to the prevention of complications of surgery.”[
Efforts to improve patient satisfaction at other hospitals have included performing handoff procedures in front of patients,[
In the UCSF Department of Neurosurgery, we first evaluated our HCAHPS scores to determine potential areas for improvement in patient satisfaction. From July to December 2013, fewer than 80% of neurosurgical patients reported that the MDs explained things in a way that they could understand, that they got information in writing about what symptoms to look out for after they left the hospital, and that hospital staff talked to them about whether they would have the help they needed after they left the hospital. In written comments, several patients also expressed frustration that they oftentimes did not know who their doctor was. Patients were unclear who was making medical decisions, because they were cared for by a large team of different medical professionals, including attending physicians, residents, nurse practitioners, and other hospital support staff.
We addressed several of these issues by (i) writing and distributing preoperative expectation letters and (ii) creating a trifold brochure with names, photographs, and specialty/training information about the care team on the neurosurgical service. The purpose of our Patient Education Bundle was to set clear expectations for the hospitalization, thereby avoiding frustration and confusion due to uncertainty (When is my doctor going to see me? Who is my actual doctor?) and to clarify the identity and roles of the different members of the neurosurgical team.
In this paper, we present the results of our Patient Education Bundle by comparing HCAHPS scores before and after our intervention (which began on January 1, 2014), as well as the results of a brief patient survey specifically regarding the bundled intervention.
MATERIALS AND METHODS
Our resident and faculty team first worked together to write preoperative expectation letters for every neurosurgery attending. Each letter included the following information: Who will see the patient while they are in the hospital (attending, resident, and/or nurse practitioner), what time the resident will round in the morning, how the patient can contact the on-call resident or attending if needed, what other hospital support staff will see the patient daily (nurses, physical therapists, pharmacists), when the patient will be allowed to eat after surgery, how to prepare for discharge home, how to care for their surgical incision, and whom to contact for a follow-up appointment (see
We also created a trifold brochure with pictures and brief descriptions of all of the neurosurgery attendings, residents, and nurse practitioners at the University of California, San Francisco, Parnassus campus [
To evaluate the effectiveness of these two strategies, we analyzed the UCSF neurosurgery department HCAHPS scores 6 months before (July–December 2013) and 6 months after (January–June 2014) implementation of the Patient Education Bundle. We specifically selected the following three questions from the HCAHPS survey as most relevant to our study: “Did the MD explain things in a way you could understand?” (n = 308 July–December 2013; n = 258 January–June 2014); “Did you get information in writing about what health problems or symptoms to look out for after you left the hospital?” (n = 310 July–December 2013; n = 268 January–June 2014); “Did hospital staff talk to you about whether you would have the help you needed after you left the hospital?” (n = 312 July–December 2013; n = 262 January–June 2014). Chi-squared tests were performed and P values calculated for all comparisons using SPSS (IBM Corp. 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
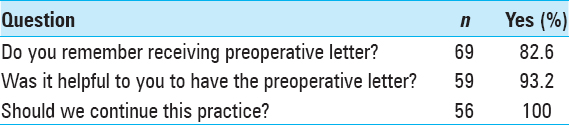
We also created a brief “Neurosurgery Patient Satisfaction Survey” that was distributed by nursing staff on our neurosurgical floor to 69 randomly selected (nonconsecutive) neurosurgical patients who agreed to participate on the day of discharge during January, February, and August of 2014. This survey had four questions: (i) Do you remember receiving the preoperative letter? (Yes/No); (ii) Was it helpful to you to have the preoperative letter? (Yes/No); (iii) How was it helpful? Respond freely; and (iv) Should we continue this practice? (Yes/No).
RESULTS
Analysis of the neurosurgery department HCAHPS scores before and after our Patient Education Bundle showed a modest trend in improvement in meeting patient information needs, although this was not statistically significant. Specifically, in the 6 months prior to our intervention (July–December 2013), 74.6% of patients responded that the MD always explained information in a way that was easy to understand. After our intervention (January–June 2014), 78.7% of patients responded that the MD always explained information in a way that was easy to understand (P = 0.194) [
Similarly, prior to our Patient Education Bundle, the percentage of patients who responded that they always got information in writing about symptoms/health problems to look out for after leaving the hospital increased from 90.9% to 94.4% after implementation of our intervention (P = 0.103). The number of patients who responded that hospital staff always spoke to them about help that they would need prior to discharge was nearly identical before and after implementation (90.4–90.6%, P = 0.924) [
Given that the HCAHPS scores provide an indirect measure of our intervention's effect, we also performed our own brief “Neurosurgery Patient Satisfaction survey” to directly measure the effect of the preoperative letters. Of the 69 patients who responded to at least one question on the “Neurosurgery Patient Satisfaction survey,” 83% remembered receiving the preoperative letter; of those, 93% found the letter helpful; and 100% thought that the preoperative letter should be continued [
DISCUSSION
Our work suggests that a Patient Education Bundle can provide a modest trend in improvement in HCAHPS scores related to communication and patient information. However, limitations of Chi-squared test include the assumption that the two populations are independent and that it does not account for any existing trends over time. It is important to consider that the improvement in HCAHPS scores is not necessarily only attributable to our intervention, as other systems-wide efforts (including simultaneous nursing efforts) may have also contributed to the improvement in HCAHPS scores observed during this time period. We also need to follow our HCAHPS scores for a longer period of time after our initial intervention (January 2014) to determine if there truly is a sustained, statistically significant improvement.
The “Neurosurgery Patient Satisfaction survey” provides a more direct measure of our specific intervention's effect and shows that our preoperative expectations letter is a promising way to improve the patient experience. Although the survey sampled only a small percentage of the population, the responses were overwhelmingly in favor of our intervention, with >=95% of patients stating that the letter was helpful to them and that we should continue this practice. In fact, one patient stated: “I have had many surgeries and never before did I get something like this. I wish I had gotten this helpful letter in all my other surgeries. Keep me and my family informed.”
We believe that patients responded so positively because the preoperative expectations letter allowed medical professionals to communicate more clearly with patients and set appropriate expectations before their hospitalization. These letters provided insight into an otherwise ambiguous and nerve-wracking process (i.e., the hospitalization for a neurosurgical procedure). The trifold brochures complemented this intervention by clearly defining the roles of an otherwise large, and confusing, group of medical professionals rounding and interacting with the hospitalized patient every day.
We believe that similar Patient Education Bundle interventions would benefit patients in other specialties and hospitals outside UCSF. We continue to look into the relationship between patient satisfaction and clinical outcomes. Our preoperative letters and trifold brochures are a low cost way to address a patient's information needs, and may lead to improved patient satisfaction. Next steps include tracking patient satisfaction over longer time periods for more robust time series analysis and investigating the association with improved patient neurosurgical outcomes.
References
1. Afsar-Manes N, Martin NA. Healthcare reform from the inside: A neurosurgical clinical quality program. Surg Neurol Int. 2012. 3: 128-
2. Chapman KB. Improving communication among nurses, patients, and physicians. Am J Nurs. 2009. 109: 21-5
3. Day MS, Hutzler LH, Karia R, Vangsness K, Setia N, Bosco JA 3 rd. Hospital-Acquired Conditions After Orthopedic Surgery Do Not Affect Patient Satisfaction Scores. J Healthc Qual. 2013. p.
4. Goldstein E, Farquhar M, Crofton C, Darby C, Garfinkel S. Measuring Hospital Care from the Patients’ Perspective: An overview of the CAHPS Hospital Survey Development Process. Health Serv Res. 2005. 40: 1977-95
5. Jha AK, Orav EJ, Zheng J, Epstein A. Patients’ Perception of Hospital Care in the United States. N Engl J Med. 2008. 359: 1921-31
6. Larson CO, Nelson EC, Gustafson D, Batalden PB. The Relationship Between Meeting Patients’ Information Needs and their Satisfaction with Hospital Care and General Health Status Outcome. Int J Qual Health Care. 1996. 8: 447-56
7. Lee KY, Loeb JM, Nadzam DM, Hanold LS. An overview of the Joint Commission's ORYX initiative and proposed statistical methods. Health Serv Outcomes Res Methodol. 2000. 1: 63-73
8. Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: A pilot study. J Hosp Med. 2014. 9: 137-41