- Department of neurosurgery, Hospital do servidor público do estado de São Paulo, 1800 Pedro de Toledo, 04039-901, São Paulo, Capital, Brazil, 551145738379
Correspondence Address:
Ricardo V. Botelho
Department of neurosurgery, Hospital do servidor público do estado de São Paulo, 1800 Pedro de Toledo, 04039-901, São Paulo, Capital, Brazil, 551145738379
DOI:10.4103/2152-7806.160322
Copyright: © 2015 Botelho RV. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Jânio A. Ferreira, Botelho RV. The odontoid process invagination in normal subjects, Chiari malformation and Basilar invagination patients: Pathophysiologic correlations with angular craniometry. Surg Neurol Int 08-Jul-2015;6:118
How to cite this URL: Jânio A. Ferreira, Botelho RV. The odontoid process invagination in normal subjects, Chiari malformation and Basilar invagination patients: Pathophysiologic correlations with angular craniometry. Surg Neurol Int 08-Jul-2015;6:118. Available from: http://surgicalneurologyint.com/surgicalint_articles/the-odontoid-process-invagination-in-normal-subjects-chiari-malformation-and-basilar-invagination-patients-pathophysiologic-correlations-with-angular-craniometry/
Abstract
Background:Craniometric studies have shown that both Chiari malformation (CM) and basilar invagination (BI) belong to a spectrum of malformations. A more precise method to differentiate between these types of CVJM is desirable. The Chamberlain's line violation (CLV) is the most common method to identify BI. The authors sought to clarify the real importance of CLV in the spectrum of craniovertebral junction malformations (CVJM) and to identify possible pathophysiological relationships.
Methods:We evaluated the CLV in a sample of CVJM, BI, CM patients and a control group of normal subjects and correlated their data with craniocervical angular craniometry.
Results:A total of 97 subjects were studied: 32 normal subjects, 41 CM patients, 9 basilar invagination type 1 (BI1) patients, and 15 basilar invagination type 2 (BI2) patients. The mean CLV violation in the groups were: The control group, 0.16 ± 0.45 cm; the CM group, 0.32 ± 0.48 cm; the BI1 group, 1.35 ± 0.5 cm; and the BI2 group, 1.98 ± 0.18 cm. There was strong correlation between CLV and Boogard's angle (R = 0.82, P = 0.000) and the clivus canal angle (R = 0.7, P = 0.000).
Conclusions:CM's CLV is discrete and similar to the normal subjects. BI1 and BI2 presented with at least of 0.95 cm CLV and these violations were strongly correlated with a primary cranial angulation (clivus horizontalization) and an acute clivus canal angle (a secondary craniocervical angle).
Keywords: Arnold–Chiari malformation, basilar impression, cephalometry, platybasia
INTRODUCTION
The most common adult craniocervical junction malformations (CVJM) are Chiari malformation (CM) [
Craniometric studies have shown that both of these malformations belong to a spectrum of malformations whose common characteristic is the underdevelopment of the occipital bone and consequent neural and cerebrospinal fluid (CSF) flow compression at the craniocervical junction. BI is the more substantial malformation and differs from CM by the displacement of the cervical spine toward the foramen magnum and ventral brainstem compression.[
Increasing evidence has identified two subgroups of BI: One is associated with craniovertebral instability in which the tip of the odontoid process projects inside the foramen magnum,[
Classically, the Chamberlain's baseline violation (CLV) has been used to diagnose BI, but in the literature, this criterion has varied between extreme values of 1 and 6.6 mm above the CLV.[
In order to reveal the relationship between CLV in BI, CM patients and normal subjects, we correlated their data with craniocervical angular craniometry to identify possible pathophysiological relationships.
MATERIALS AND METHODS
This study was approved by the Research Ethics Committee (Instituto de Assistencia Médica ao Servidor Público Estadual - sp-caae07284212000005463).
To study the degree of odontoid process invagination, we evaluated magnetic resonance imaging (MRI) scans of the craniocervical junction in T1 and T2 midline sagittal scan acquisitions from a CVJM patient sample consecutively treated by the authors between 1996 and 2012. Computed tomography (CT) scans were used only in specific cases, when necessary, to clarify details of bone anatomy.
The measurements were performed by an observer who was unaware of other study data.
Patients with CVJM were divided into three groups: CM patients, basilar invagination type 1 (BI1) patients and basilar invagination type 2 (BI2) patients.[
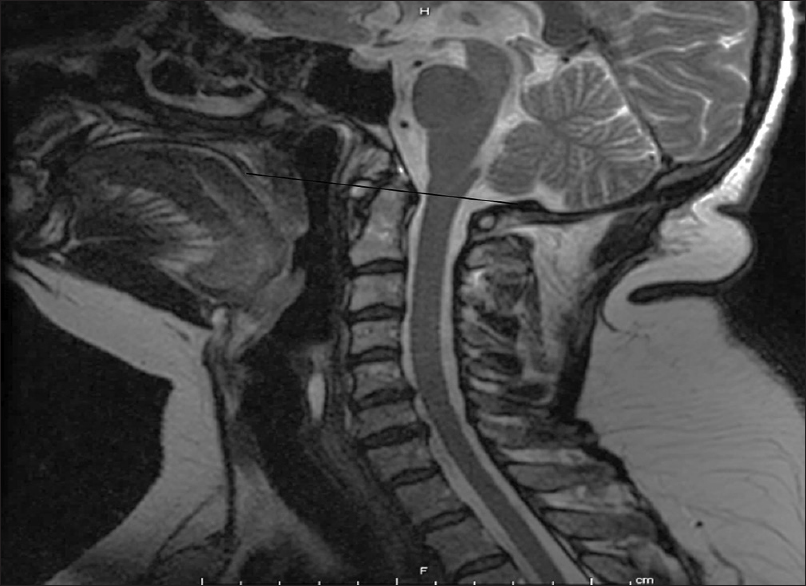
Patients with CM had symptomatic cerebellar tonsil herniation and/or posterior fossa structure and cisterna magna compressions [
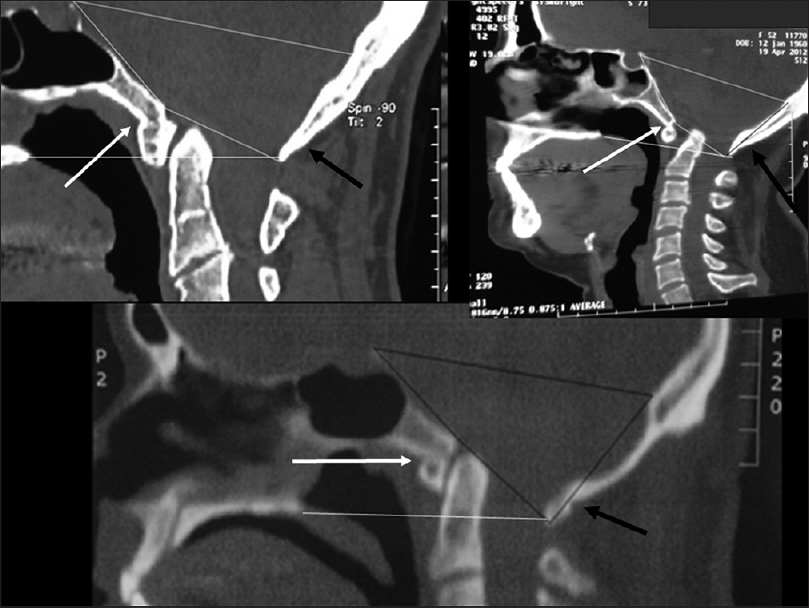
Patients with BI were divided into two groups: Those with axis dens invagination into the foramen magnum were referred to as type I (BI1) [
Patients with invagination of the dens toward the base of the skull but not toward the inside of the foramen magnum were classified as BI2 [
The studied sample was based on primary craniovertebral junction malformations without any immediate evident inflammatory, bone, or connective tissue disease.
To compare these findings with the odontoid process invagination in normal subjects (control group), images from 32 consecutive normal subjects were evaluated [
Patients who had normal MRI scans that were performed by the Radiology Department of the Hospital do Mandaqui to clarify cervical spine or head symptoms and who were matched by age and sex to the CCJM group made up the control group. Patients with tumors, trauma, and any diagnostic pathology were excluded from this study.
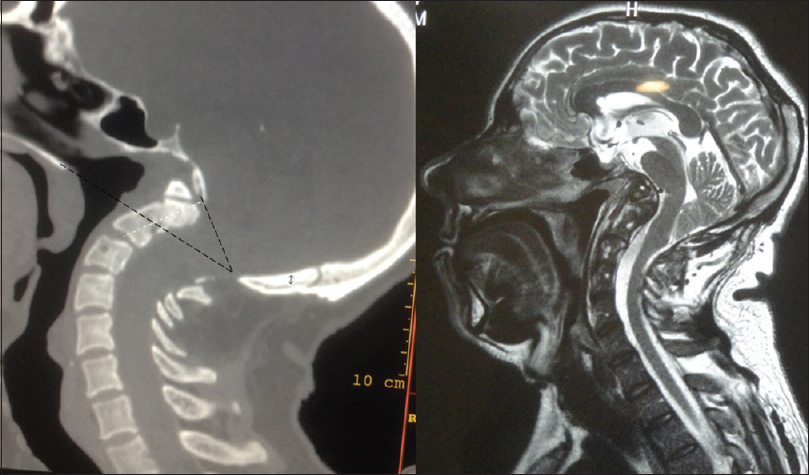
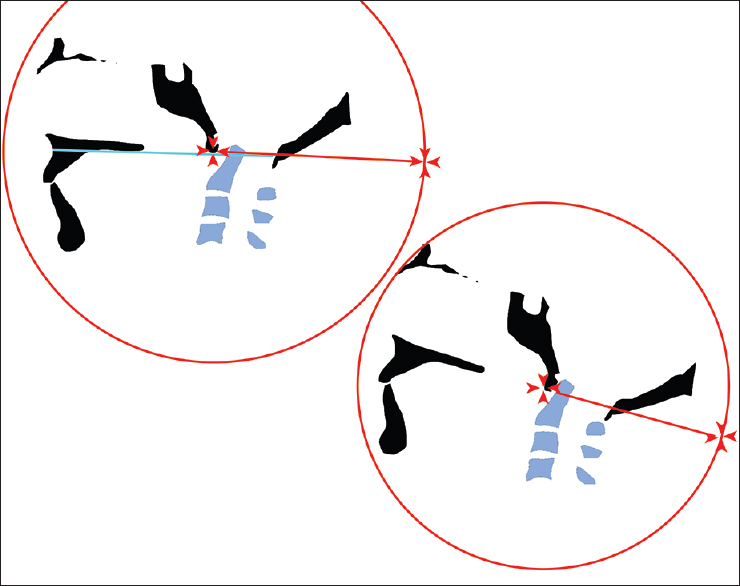
The amount of Chamberlain's basal line violation (CLV) was measured as follows [
Figure 5
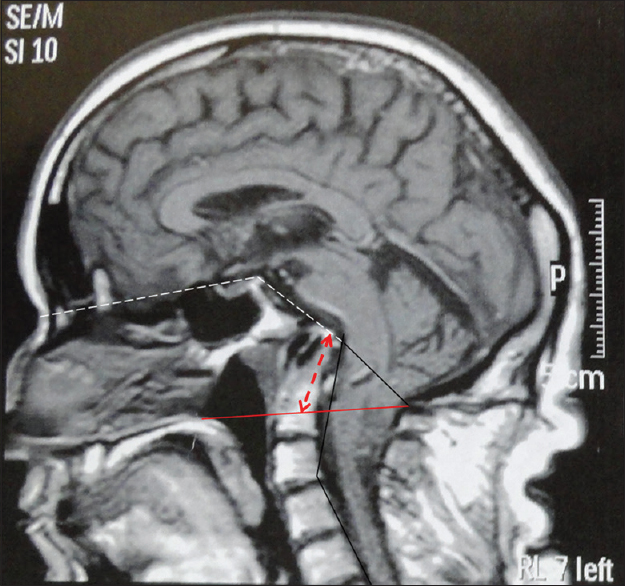
Type 2 Basilar invagination. The red line is the Chamberlain's Line (CL). The dotted red arrow represents CLV. Dotted white lines above represents Welcher's angle. The angle formed by the inferior dotted white line and solid black line is the Boogard's angle. The vertical lines along with C2 and C7 axis forms the cervical spine lordosis angle
Images from the midline craniocervical MRI (or CT) were digitalized, and the CLV was traced from the hard palate to the opistion. The distance above or below the CLV was measured using the Meazure 3.2 software and the image ruler. The distance above the CLV was considered positive measurements, and the distance below the CLV was considered negative measurements. The 95% confidence interval was set as the limits for BI diagnosis.
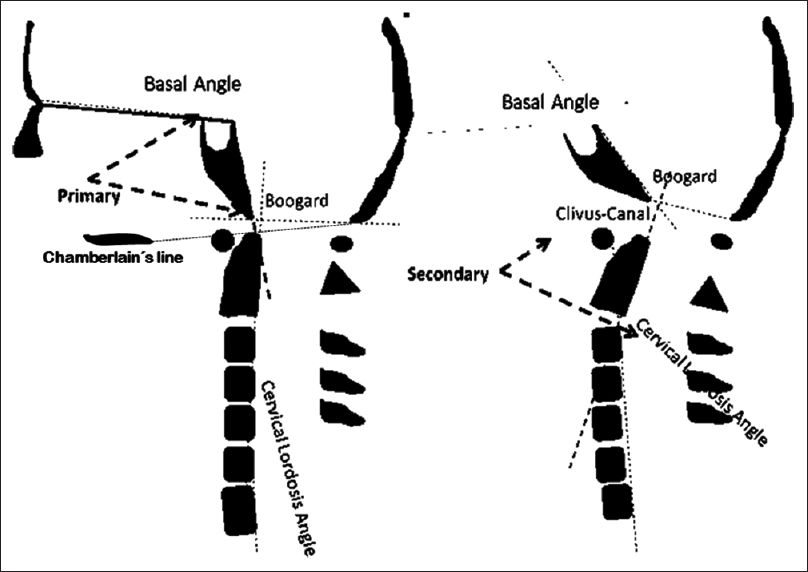
One study evaluating craniovertebral angulations among CCJM and normal subjects revealed significant differences between the groups.[
Basal angle (BA): Defined as the angle measured from the nasion, top of the dorsum sellae, and the basion.[
CC: The angle between the line extending from the top of the dorsum sellae to the basion and the line between the inferodorsal portions of C2 to the most superodorsal part of the dens.
BOO: The angle between the top of the dorsum sellae, basion, and opisthion.[
CL: The angle between a line drawn from the most inferodorsal to the most superodorsal part of C2 (dens of the axis) and another line drawn between the supero- and inferodorsal regions of the C7 posterior vertebral body.[
The degree of CLV was correlated to the primary cranial angles and secondary craniovertebral angles.
Statistics: Demographic data and descriptive statistics are expressed as the media, standard deviation and 95% confidence intervals. The Kolmogorov–Smirnov test was used to evaluate the normality of the numeric variable distribution. The Levine test was used to verify the variance homogeneity. Gender distributions were compared with the Chi-squared test. The ANOVA Kruskal–Wallis test was used to compare the media of the four groups, and Bonferroni's (correction) test was used as a post hoc test. The correlations between CLV and the cranial and craniovertebral angles were tested with the Spearman correlation test. The correlation strength was classified as follows: 0: Absence of correlation; 0.1–0.3: Weak correlation; 0.4–0.6: Moderate correlation; >0.6–0.9: Strong correlation; and 1: Perfect correlation.
RESULTS
A total of 97 subjects were studied: 32 normal subjects in the control group, 41 CM patients, 9 BI1 patients and 15 BI2 patients.
The mean age of the control group was 44.8 ± 12 years, and the mean age in the craniovertebral junction malformation groups was 46.9 ± 11 years (t test: P = 0.40).
Among the 32 normal subjects, 17 were male, and among the 65 malformation patients, 30 were male (Chi-square, P = 0.51).
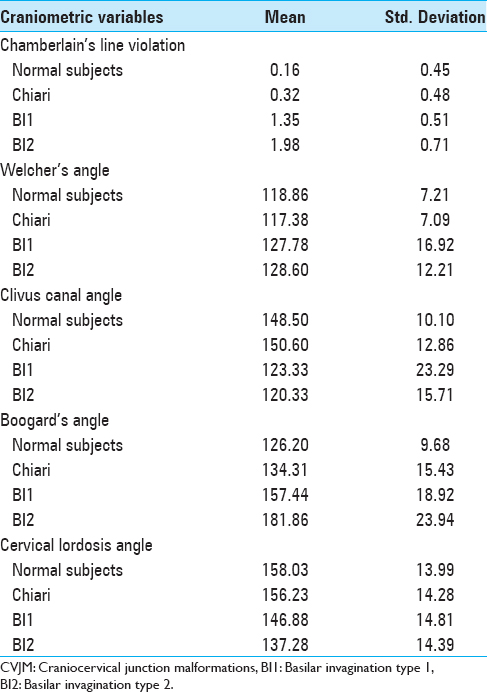
Descriptive data for CLV, Welcher angle, CC, BOO, and CL for all groups are described in
Chamberlain's line violation
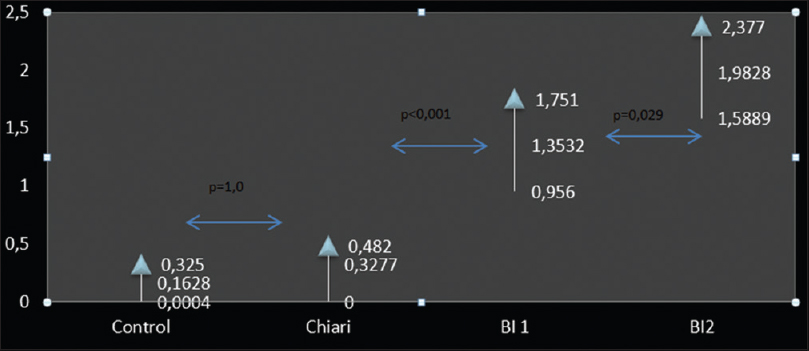
The mean and 95% confidence intervals of CLV in the three groups are illustrated in
The mean CLV values were as follows: The control group (CTRL), 0.16 ± 0.45 cm; the CM group, 0.32 ± 0.48 cm; the BI1 group, 1.35 ± 0.5 cm; and the BI2 group, 1.98 ± 0.18 cm.
The CLV differed among the four groups (ANOVA–Kruskal–Wallis, P < 0.001).
The post hoc (Bonferroni) test revealed that the CLV between the CTRL and CM groups did not differ (P = 1.0). Both groups differed from the BI1 and BI2 groups (Bonferroni; P < 0.001). The IB2 group exhibited significantly greater CLV than the BI1 group (1.98 × 1.35, Bonferroni, P = 0.029).
Correlation among CLV and the craniometric Welcher, Clivus canal, Boogard, and cervical lordosis angle
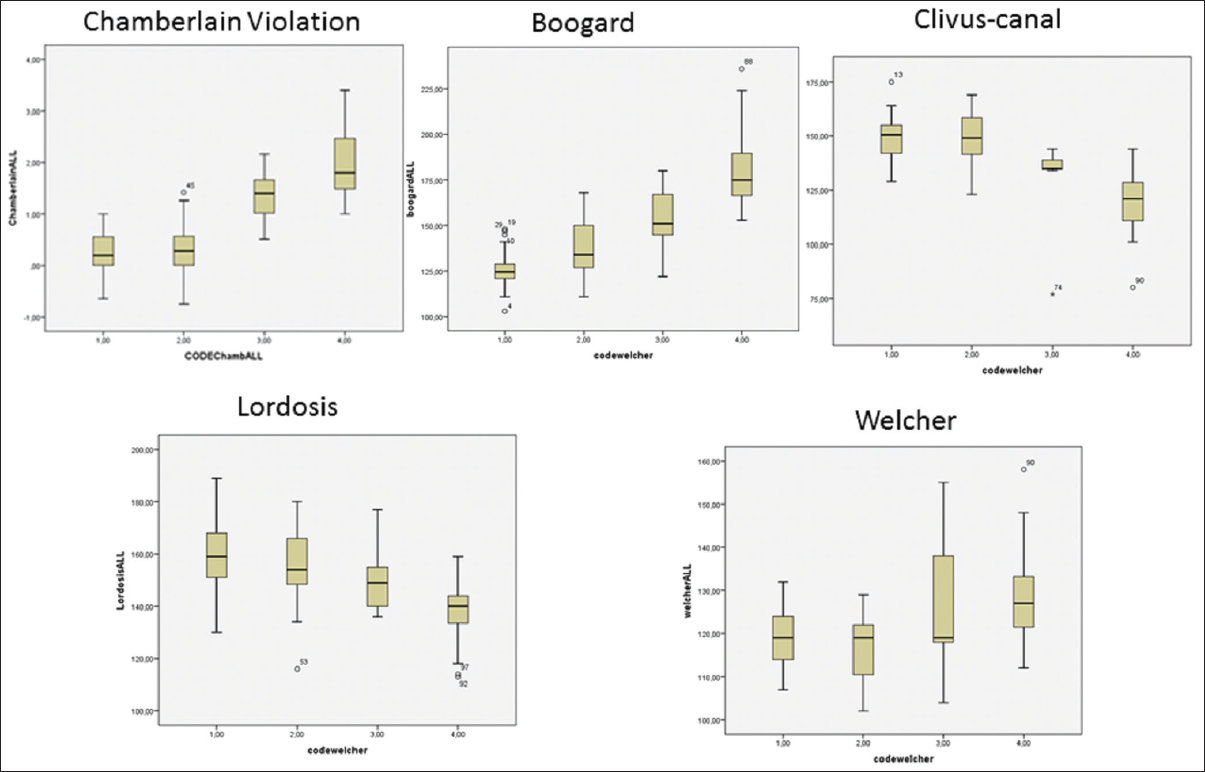
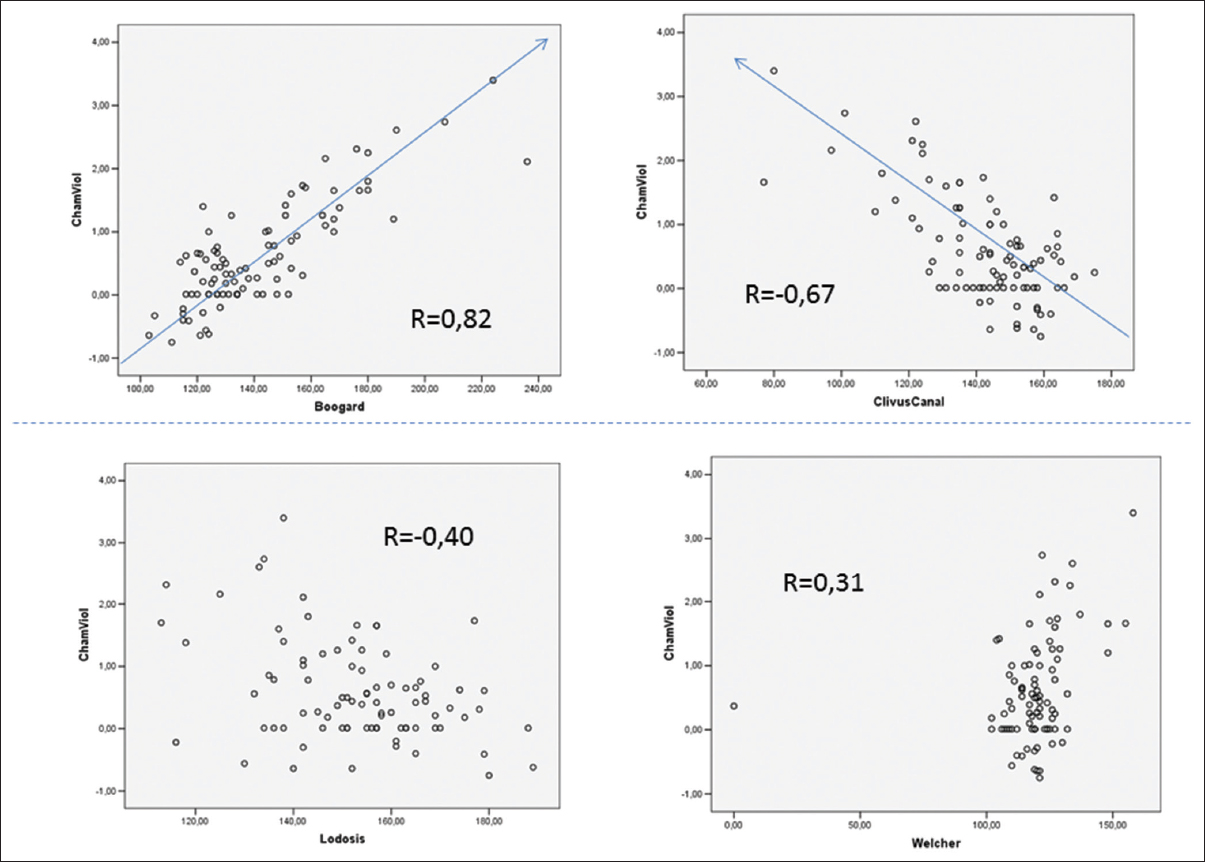
To evaluate the physiopathological association with the cranial or craniocervical angles, a Spearman correlation among these variables was tested [Figures
Figure 8
Illustration of descriptive statistcs for Chamberlain's line violation, Boogard's angle, Clivus canal angle, cervical lordosis angles (Lordosis) and Welcher's angle (Welcher). In the x-axis, 1, 2, 3, and 4 is referred to control group, Chiari malformation, Basilar Invagination type 1 and Basilar invagination type 2 groups, respectively. Note that as the as the CLV increases, Boogard's values increase and Clivus canal and Cervical lordosis angle decrease
Figure 9
Scatter dot plot. Upper part: At left, data from CLV are plotted against Boogard's angle. The “R” numbers are referred to the amount of correlation between data. At right, data from CLV and Clivus canal angle are plotted. Lower left: Relation between cervical lordosis angle and CLV. At right, relation between Welcher angle and CLV
DISCUSSION
BI was originally described by Ackermann in cretins from the Alps.[
In 1939, Chamberlain described four cases of basilar impression, and his method for diagnosing this condition was the “base line.”[
Craniocervical junction patient's identification has significantly improved in the last three decades. MRI has increased the diagnosis of tonsillar herniation through the foramen magnum and has facilitated the identification of BI patients with and without craniovertebral instability but a more precise definition of the malformation types is lacking.[
BI may be “primary” (resulting from a congenital or developmental anomaly) or “secondary” (basilar impression), resulting from bony softening and molding.[
The term CM, as currently defined, have included heterogeneous group of disorders with different pathogenetic origins.[
Two relatively new treatment modalities have been used for treating BI: The anterior transnasal endoscopic approach and the posterior reduction and stabilization approach.[
A careful observation of a series of publications on adult BI cases revealed that BI invaginations associated with instability are a homogeneous group with common characteristics: Anterior atlas assimilation and ventral brainstem compression by the odontoid process invagination through the foramen magnum.[
BI without instability is associated with greater cranial deformity, greater clivus horizontalization, an acute CC, and associated platybasia [Figures
CLV analysis suggests fundamental differences among the CCJM groups. In the CM group, the upper confidence limit is set to below 5 mm. The amount of CLV in this group is small and was not significantly different from the control group. Other angular craniometric CM values did not differ from those in normal subjects.[
The strongest correlation with CLV was shown by the clivus horizontalization measured by BOO, and the second strongest correlation with CLV was shown by the CC. The association of CLV with one primary cranial angle suggests that the skull shape has is a direct determinant of the physiopathology of CLV and ventral brainstem compression. Published data shows that clivus horizontalization is associated with craniovertebral angulation and craniocervical kyphosis.[
CONCLUSIONS
CM patients presented with discrete CLV similar to normal subjects. BI1 presented a CLV of at least of 0.96 cm and BI2 patients had at least 1.5 cm of CLV. There is strong correlation with CLV and clivus horizontalization, suggesting pathopysiologic relationship with the primary cranial angle and, with and CC, a secondary craniocervical angle.
References
1. Botelho RV, Ferreira ED. Angular craniometry in craniocervical junction malformation. Neurosurg Rev. 2013. 36: 603-10
2. Botelho RV, Beco Neto E, Patriota GC, Daniel JW, Dumont PAS, Rotta JM. Basilar invagination: Craniocervical instability treated with cervical traction and occipitocervical fixation. J Neurosurg Spine. 2007. 7: 444-9
3. Chamberlain WE. Basilar Impression (Platybasia): A Bizarre Developmental Anomaly of the Occipital Bone and Upper Cervical Spine with Striking and Misleading Neurologic Manifestations. Yale J Biol Med. 1939. 11: 487-96
4. Dahdaleh NS, Dlouhy BJ, Menezes AH. Application of neuromuscular blockade and intraoperative 3D imaging in the reduction of basilar invagination. Technical note. J Neurosurg Pediatrics. 2012. 9: 119-24
5. El-Sayed IH, Wu J, Dhillon N, Ames CP, Mummaneni P. The Importance of Platybasia and the Palatine Line in Patient Selection for Endonasal Surgery of the Craniocervical Junction: A Radiographic Study of 12 Patients. World Neurosurg. 2011. 76: 183-8
6. Goel A, Bhatjiwalem M, Desai K. Basilar invagination: A study based on 190 surgically treated Patients. J Neurosurg. 1998. 88: 962-8
7. Goel A, Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009. 10: 220-7
8. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004. 1: 281-6
9. Hsu W, Zaidi HA, Suk I, Gokaslan ZL, Wolinsky JP. A new technique for intraoperative reduction of occipitocervical instability. Neurosurgery. 2010. 66: S319-
10. Joseph V, Rajshekhar V. Resolution of syringomyelia and basilar invagination after traction. Case illustration. J Neurosurg. 2003. 98: S298-
11. Kim IS, Hong JT, Sung JH, Byun JH. Vertical reduction using atlantoaxial facet spacer in basilar invagination with atlantoaxial instability. J Korean Neurosurg Soc. 2011. 50: 528-31
12. Konigsberg RA, Vakil N, Hong TA, Htaik T, Faerber E, Maiorano T. Evaluation of platybasia with MR imaging. AJNR Am J Neuroradiol. 2005. 26: 89-92
13. Kwong Y, Rao N, Latief K. Craniometric measurements in the assessment of craniovertebral settling: Are they still relevant in the age of cross-sectional imaging?. AJR Am J Roentgenol. 2011. 196: W421-5
14. Mcgirt MJ, Attenello FJ, Sciubba DM, Gokaslan ZL, Wolinsky J. Endoscopic transcervical odontoidectomy for pediatric basilar invagination and cranial settling. J Neurosurg Pediatrics. 2008. 1: 337-42
15. Milhorat TH, Bolognese PA, Nishikawa M, McDonnell NB, Francomano CA. Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and Chiari malformation type I in patients with hereditary disorders of connective tissue. J Neurosurg Spine. 2007. 7: 601-9
16. Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD. Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management. Acta Neurochir. 2010. 152: 1117-27
17. Nishikawa M, Ohata K, Baba M, Terakawa Y, Hara M. Chiari I malformation associated with ventral compression and instability: One-stage posterior decompression and fusion with a new instrumentation technique. Neurosurgery. 2004. 54: 1430-4
18. Nishikawa M, Sakamoo H, Hakuba A, Nakanishi N, Inoue Y. Pathogenesis of Chiari malformation: A morphometric study of the posterior cranial fossa. J Neurosurg. 1997. 86: 40-7
19. Peng X, Chen L, Wan Y, Zou X. Treatment of primary basilar invagination by cervical traction and posterior instrumented reduction together with occipitocervical fusion. Spine. 2011. 36: 1528-31
20. Silva JAG da, Santos AA do, Melo LRS, de Araújo AFA, Regueira GP. Posterior fossa decompression with tonsillectomy in 104 cases of basilar impression, Chiari malformation and/or syringomyelia. Arq Neuropsiquiatr. 2011. 69: 817-23
21. Simsek S, Yigitkanli K, Belen D, Bavbek M. Halo traction in basilar invagination: technical case report. Surg Neurol. 2006. 66: 311-4
22. Smoker WR. Craniovertebral junction: Normal anatomy, craniometry, and congenital anomalies. Radiographics. 1994. 14: 255-77
23. Vet AD. Basilar impression of the skull. J Neurol Psychiatry. 1940. 3: 241-50
24. Young RM, Sherman JH, Wind JJ, Litvack Z, O’Brien J. Treatment of craniocervical instability using a posterior-only approach. J Neurosurg Spine. 2014. 21: 239-48
25. Yu Y, Wang X, Zhang X, Hu F, Gu Y, Xie T. Endoscopic transnasal odontoidectomy to treat basilar invagination with congenital osseous malformations. Eur Spine J. 2013. 22: 1127-36








Donovan Bratsch
Posted March 28, 2017, 7:54 am
I have recently been diagnosed with BI and am preparing to have corrective surgery. This publication was helpful for me to understand my condition. My BI has caused a syrinx from C-1 to T-12 8mm wide.