- Department of Neurological Surgery, University of Washington School of Medicine, Seattle, Washington, USA
- Department of Surgery, University of Washington School of Medicine, Seattle, Washington, USA
Correspondence Address:
James Bales
Department of Neurological Surgery, University of Washington School of Medicine, Seattle, Washington, USA
DOI:10.4103/2152-7806.196930
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: James Bales, Ryan P. Morton, Nathan Airhart, David Flum, Anthony M. Avellino. Transanal presentation of a distal ventriculoperitoneal shunt catheter: Management of bowel perforation without laparotomy. 28-Dec-2016;7:
How to cite this URL: James Bales, Ryan P. Morton, Nathan Airhart, David Flum, Anthony M. Avellino. Transanal presentation of a distal ventriculoperitoneal shunt catheter: Management of bowel perforation without laparotomy. 28-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/transanal-presentation-of-a-distal-ventriculoperitoneal-shunt-catheter-management-of-bowel-perforation-without-laparotomy/
Abstract
Background:Bowel perforation is a serious but rare complication after a ventriculoperitoneal shunt (VPS) procedure. Prior studies have reported spontaneous bowel perforation after VPS placement in adults of up to 0.07%. Transanal catheter protrusion is a potential presentation of VPS bowel perforation and places a patient at risk for both peritonitis and ventriculitis/meningitis via retrograde migration of bacteria. This delayed complication can be fatal if unrecognized, with a 15% risk of mortality secondary to ventriculitis, peritonitis, or sepsis.
Case Description:We describe a unique case of a patient with distal VPS catheter protrusion from the anus whose bowel perforation did not cause clinical sequelae of infection. We were able to manage the patient without laparotomy.
Conclusions:A subset of patients can be managed without laparotomy and only with externalization of the ventricular shunt with antibiotics until the cerebrospinal fluid cultures finalize without growth.
Keywords: Bowel perforation, complications, ventriculoperitoneal shunt
INTRODUCTION
Peritoneal complications of ventricular shunt placement (VPS) are uncommon along with serious events.[
Regardless of prompt recognition of this uncommon condition, important and delayed recognition can have significant consequences for patient care.
CASE REPORT
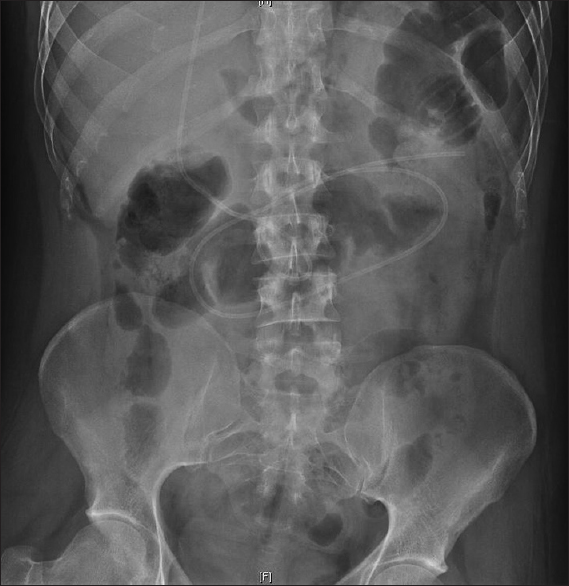
A 29-year-old male with shunted congenital hydrocephalus of unknown etiology with previous revisions in infancy and as a young child initially presented to the neurosurgery clinic with worsening headaches and complaints of blurred vision for more than 18 months. Computerized tomography (CT) of the head demonstrated a slight increase in his ventricular size; physical evaluation noted mild chronic papilledema and reduced visual acuity in his left eye, which was baseline following a car accident a few years earlier. He had a right parietal VPS in place; shunt series X-rays showed no shunt disconnections. In addition, abdominal X-rays demonstrated a retained peritoneal distal catheter from his previous shunt revision operations. Given the concerns for shunt failure, he underwent shunt exploration and revision for management. During the shunt revision surgery, the valve was found to be nonfunctional and was replaced; the retained peritoneal distal catheter was also removed laparoscopically by the general surgery team. His initial postoperative course was uncomplicated, and he was discharged on postoperative day 1 with decrease in his headaches and improvement in his subjective complaint of blurry vision.
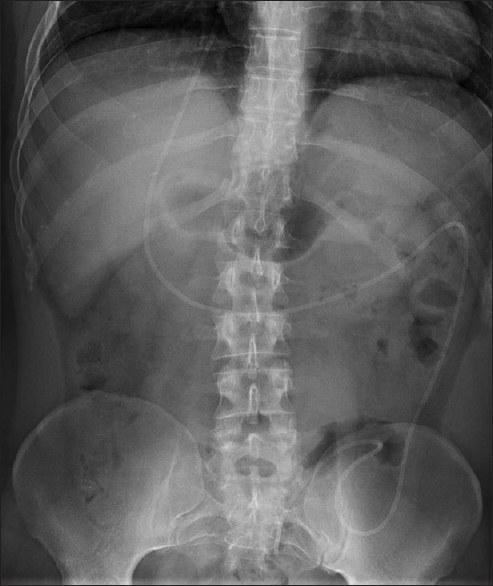
He again presented 17 months later with continual headaches, decrease in vision, and increased ventricular size. This time he was noted to have acute papilledema and worsened visual acuity in his right eye. Given the concern regarding the age of the ventricular and distal catheter in his right parietal system, which had been placed at 4 months of age, it was determined that the placement of a new shunt system would be the best clinical option. He underwent another VPS revision with placement of a new right frontal VPS shunt and a new distal peritoneal catheter placed laparoscopically by the general surgery team [
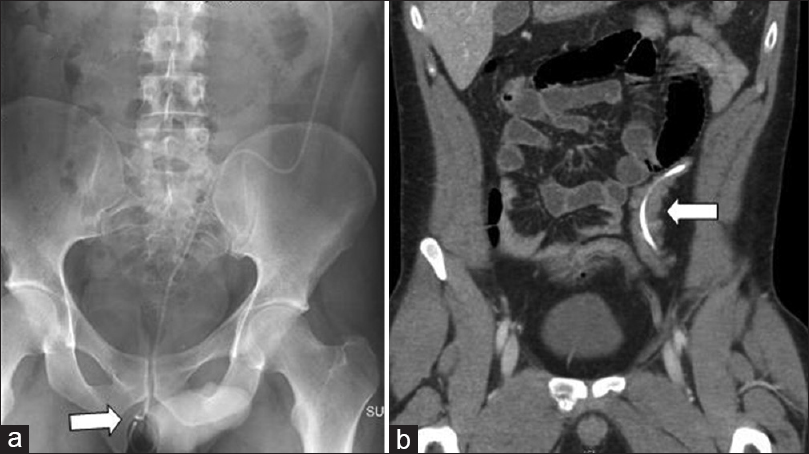
One month later, he presented with continued complaints of an object intermittently protruding from his rectum. During the emergency room evaluation, a neurosurgical consultation was obtained and the rectal exam revealed that the distal peritoneal catheter was protruding through his anus. X-rays corroborated the physical exam [
INTERVENTION PERFORMED
Because the patient was clinical asymptomatic except for the distal catheter protrusion through the anus, the general surgery team was consulted, and we decided to expose and externalize the distal catheter at the clavicle with simultaneous removal of the remaining distal catheter through the previous laparoscopic abdominal incision in a manner described previously.[
POSTOPERATIVE COURSE
The patient was placed on a triple antibiotic regiment of flagyl, vancomycin, and cefepime; daily CSF cultures from the externalized shunt revealed no bacterial growth. After 5 days of negative cultures, he underwent removal of all previous hardware and placement of a new right frontal ventriculoatrial shunt. His antibiotic regimen was continued for 1 day and he was discharged on postoperative day 2 without further antibiotics. At the patient's 6 month postoperative visit, he was doing well with no signs of infection and decreased headaches.
DISCUSSION
At our institution, it is common practice to enlist the assistance of general surgery to place the distal catheter laparoscopically. The reason for this is the theoretical advantage of visualizing the distal catheter within the peritoneal space, thus reducing the likelihood of incorrect placement; it also allows for a small incision and good wound healing at the distal site. However, as with any laparoscopic procedure, it is possible that a bowel injury was caused at the time of operation. The reported incidence of laparoscopic-induced bowel perforation is 0.22%, and most are recognized at the time of surgery.[
The exact pathogenesis of spontaneous bowel perforation is unclear having been first reported by Wilson and Bertran[
Clinical presentation may be straightforward with 44% of the patients having abdominal pain, vomiting, and fever, and 50% with clinical signs of meningitis.[
Management of bowel perforation is highly individualized and dependent upon the presenting signs and symptoms of the patient. Immediate externalization is necessary to maintain shunt patency, as well as to limit the retrograde spread of bacteria along the shunt system which can cause ventriculitis or meningitis.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abu-Dalu K, Pode D, Hadani M, Safar A. Colonic complications of ventriculoperitoneal shunts. Neurosurgery. 1983. 13: 167-9
2. Akcora B, Serarslan Y, Sangun O. Bowel perforation and transanal protrusion of a ventriculoperitoneal shunt catheter. Pediatr Neurosurg. 2006. 42: 129-31
3. Brownlee JD, Brodley JS, Schaefer IK. Colonic perforation by ventriculoperitoneal shunt tubing: A case of suspected silicon allergy. Surg Neurol. 1998. 49: 21-4
4. Ferreira PR, Bizzi JJ, Amantea SL. Protrusion of ventriculoperitoneal shunt catheter through the anal orifice. A rare abdominal complication. J Pediatr Surg. 2005. 40: 1509-10
5. Hornig GW, Shillito J. Intestinal perforation by peritoneal shunt tubing: Report of two cases. Surg Neurol. 1990. 33: 288-90
6. Ibrahim AW. E-coli meningitis as an indicator of intestinal perforation by V-P shunt tube. Neurosurg Rev. 1998. 21: 194-7
7. Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A. Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: Case report and a review of 45 cases. Surg Neurol. 2000. 54: 388-96
8. Schulhof LA, Worth RM, Kalsbeck JE. Bowel perforation due to peritoneal shunt. A report of 7 cases and a review of the literature. Surg Neurol. 1975. 3: 265-9
9. Sells CJ, Loeser JD. Peritonitis following perforation of the bowel: A rare complication of a ventriculoperitoneal shunt. J Pediatr. 1973. 83: 823-4
10. Sharma A, Pandey AK, Radhakrishnan M, Kumbhani D, Das HS, Desai N. Endoscopic management of anal protrusion of ventriculo-peritoneal shunt. Indian J Gastroenterol. 2003. 22: 29-30
11. Snow RB, Lavyne MH, Fraser RA. Colonic perforation by ventriculoperitoneal shunts. Surg Neurol. 1986. 25: 173-7
12. van der Voort M, Heijnsdijk EA, Gouma DJ. Bowel injury as a complication of laparoscopy. Br J Surg. 2004. 91: 1253-8
13. Wilson CB, Bertan V. Perforation of the bowel complicating peritoneal shunt for hydrocephalus. Report of two cases. Am Surg. 1966. 32: 601-3
14. Yousfi MM, Jackson NS, Abbas M, Zimmerman RS, Fleischer DE. Bowel perforation complicating ventriculoperitoneal shunt: Case report and review. Gastrointest Endosc. 2003. 58: 144-8