- Department of Neurosurgery, Chiba Hokuso Hospital, Nippon Medical School, Inzai, Chiba, Japan
- Department of Neurosurgery, Kushiro Rosai Hospital, Kushiro, Hokkaido, Japan
- Department of Neurosurgery, Nippon Medical School, Tokyo, Japan
- Department of Neurology, Sapporo Yamanoue Hospital, Spporo, Hokkaido, Japan
Correspondence Address:
Kyongsong Kim
Department of Neurology, Sapporo Yamanoue Hospital, Spporo, Hokkaido, Japan
DOI:10.4103/2152-7806.170455
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kim K, Isu T, Chiba Y, Iwamoto N, Yamazaki K, Morimoto D, Isobe M, Inoue K. Treatment of low back pain in patients with vertebral compression fractures and superior cluneal nerve entrapment neuropathies. Surg Neurol Int 25-Nov-2015;6:
How to cite this URL: Kim K, Isu T, Chiba Y, Iwamoto N, Yamazaki K, Morimoto D, Isobe M, Inoue K. Treatment of low back pain in patients with vertebral compression fractures and superior cluneal nerve entrapment neuropathies. Surg Neurol Int 25-Nov-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/treatment-of-low-back-pain-in-patients-with-vertebral-compression/
Abstract
Background:Superior cluneal nerve entrapment neuropathy (SCN-EN) may contribute to low back pain (LBP). However, it is often misdiagnosed as lumbar spine disorder and poorly understood.
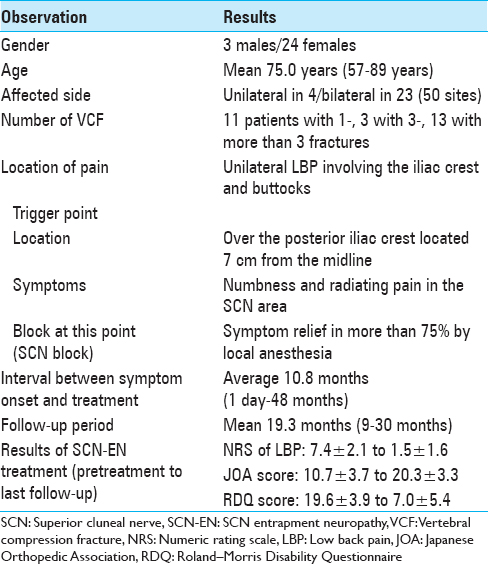
Methods:Between April 2012 and September 2013, we treated 27 patients (3 men, 24 women; mean age 75.0 years) with LBP due to SCN-EN elicited by vertebral compression fractures. Symptoms were unilateral in 4 patients and bilateral in 23 patients. The interval between symptom onset and treatment averaged 10.8 months; the mean postoperative follow-up period was 19.0 months. The clinical outcomes were assessed utilizing the numeric rating scale (NRS) for LBP, the Japanese Orthopedic Association (JOA) score, and the Roland–Morris Disability Questionnaire (RDQ) before and after treatment (e.g., until the latest follow-up).
Results:LBP in 17 patients was immediately improved by SCN block only. The remaining 10 patients required surgery (involving 18 sites) as SCN blocks were only transiently effective. Operative intervention resulted in the immediate and continued improvement of their LBP. Notably, their NRS decreased from 7.4 to 1.5, their RDQ scores from 19.6 to 7.0, and their JOA scores increased from 10.7 to 20.3.
Conclusions:In this series, 27 patients with LBP due to SCN-EN responded either to SCN blocks (17 patients) or surgical release of SCN entrapment (10 patients at 18 sites).
Keywords: Entrapment neuropathy, less invasive, low back pain, neurolysis, superior cluneal nerve, vertebral compression fracture
INTRODUCTION
Superior cluneal nerve entrapment neuropathy (SCN-EN) may contribute to low back pain (LBP) involving the iliac crest and buttocks.[
MATERIALS AND METHODS
Between April 2012 and September 2013, we treated 27 LBP patients with SCN-EN and vertebral compression fractures (VCFs), it was induced by the movement such as rolling, standing, or walking [
Surgical procedure for superior cluneal nerve entrapment neuropathy
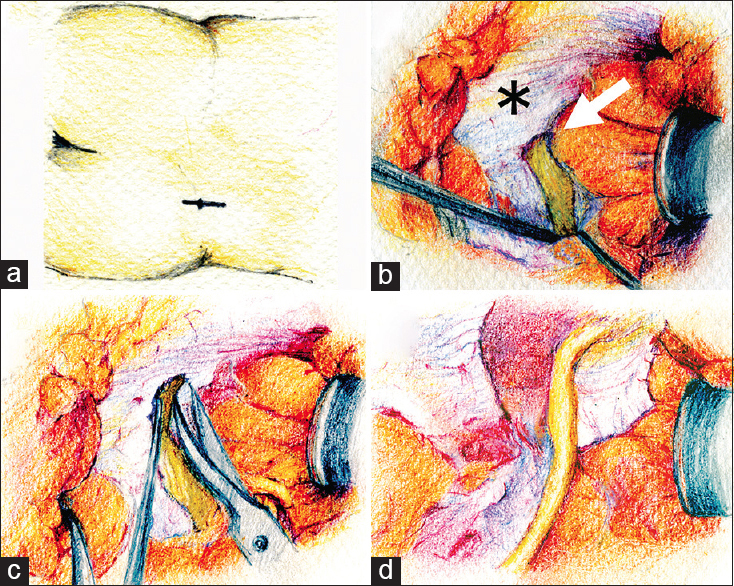
We performed microsurgical release for SCN-EN entrapment in the prone position in 10 patients (at 18 sites). First, a 5-cm-long skin incision was made across the trigger point on the iliac crest; this allowed for identification of the SCN nerve (e.g., located on the fat overlying the subcutaneous compartment) [
Figure 1
(a) A 5-cm-long skin incision is made across the trigger point on the iliac crest. (b) The superior cluneal nerve penetrates the thoracolumbar fascia (*) through the orifice (arrow) just before crossing over the iliac crest. (c) The orifice of the thoracolumbar fascia is opened and released by sharp dissection with microscissors along the superior cluneal nerve. (d) The superior cluneal nerve is decompressed and mobilized
RESULTS
We first performed repetitive SCN block; in 17 patients this produced pain reduction. The senior author (T.I.) operated 18 sites in 10 patients because pain alleviation was transient. One operated patient suffered LBP recurrence and underwent re-operation to address other SCNs. There were no surgical complications. SCN-EN treatment led to significant LBP improvement [
DISCUSSION
In some patients with VCF, LBP is not adequately controlled by conservative measures and pain control medications may be poorly tolerated. Our experience suggests that in some patients SCN-EN contributes to LBP after VCF. Entrapment and irritation of the SCN at the orifice where it penetrates the thoracolumbar fascia produces LBP, and 1.6–12.0% of LBP has been reported to be due to SCN-EN.[
CONCLUSIONS
We report 27 patients with VCF and LBP attributable to SCN-EN. They experienced pain abatement by SCN block or surgical release of the SCN entrapment. We suggest that SCN-EN should be considered and addressed in patients with VCF resulting in LBP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K. Intermittent low back pain attributable to superior cluneal nerve entrapment neuropathy. J Neurosurg Spine. p.
2. Kim K, Isu T, Chiba Y, Morimoto D, Ohtsubo S, Kusano M. The usefulness of ICG video angiography in the surgical treatment of superior cluneal nerve entrapment neuropathy: Technical note. J Neurosurg Spine. 2013. 19: 624-8
3. Kuniya H, Aota Y, Saito T, Kamiya Y, Funakoshi K, Terayama H. Anatomical study of superior cluneal nerve entrapment. J Neurosurg Spine. 2013. 19: 76-80
4. Maigne JY, Doursounian L. Entrapment neuropathy of the medial superior cluneal nerve. Nineteen cases surgically treated, with a minimum of 2 years’ follow-up. Spine (Phila Pa 1976). 1997. 22: 1156-9
5. Morimoto D, Isu T, Kim K, Imai T, Yamazaki K, Matsumoto R. Surgical treatment of superior cluneal nerve entrapment neuropathy. J Neurosurg Spine. 2013. 19: 71-5