- Department of Neurosurgery, Tecnologico de Monterrey, Monterrey, Nuevo León, México
- Department of Neurology, Tecnologico de Monterrey, Monterrey, Nuevo León, México
- Department of Otolaryngology, Tecnologico de Monterrey, Monterrey, Nuevo León, México
Correspondence Address:
Enrique Caro-Osorio
Department of Neurosurgery, Tecnologico de Monterrey, Monterrey, Nuevo León, México
DOI:10.4103/sni.sni_449_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Enrique Caro-Osorio, Alba Espino-Ojeda, Lino Guevara-Maldonado, José C Herrera-Castro. Utility of magnetic resonance cisternography with intrathecal gadolinium in detection of cerebrospinal fluid fistula associated with Mondini dysplasia in a patient with recurrent meningitis: Case report and literature review. 26-Apr-2018;9:92
How to cite this URL: Enrique Caro-Osorio, Alba Espino-Ojeda, Lino Guevara-Maldonado, José C Herrera-Castro. Utility of magnetic resonance cisternography with intrathecal gadolinium in detection of cerebrospinal fluid fistula associated with Mondini dysplasia in a patient with recurrent meningitis: Case report and literature review. 26-Apr-2018;9:92. Available from: http://surgicalneurologyint.com/surgicalint-articles/utility-of-magnetic-resonance-cisternography-with-intrathecal-gadolinium-in-detection-of-cerebrospinal-fluid-fistula-associated-with-mondini-dysplasia-in-a-patient-with-recurrent-meningitis-case-repo/
Abstract
Background:The intrathecal contrast-enhanced magnetic resonance cisternography (MRC) is a diagnostic method that has been proven effective in selected patients with various disorders of the cerebrospinal system, including the detection of cerebrospinal fluid (CSF) leaks. The Mondini dysplasia is a malformation of the inner ear characterized by an incomplete cochlear development. The cerebrospinal fistula associated with Mondini dysplasia usually occurs in the first 5–10 years.
Case Description:The case of a 34-year-old woman with CSF rhinorrhea and recurrent meningitis associated with CSF fistula into the right inner ear, which was detected by MRC with intrathecal gadolinium, is presented. The computed tomography (CT) cisternography failed to detect the exact location of the leak. The right Mondini dysplasia was identified on CT of the temporal bone. A subtotal right-sided petrosectomy and fistula closure into the bony labyrinth were performed. After the procedure the patient no longer presented meningitis or CSF leak.
Conclusions:The radiological identification of the site of CSF leak through sensitive imaging studies such as MRC with intrathecal gadolinium is crucial for surgical approach.
Keywords: Intrathecal gadolinium, Mondini dysplasia, magnetic resonance cisternography, recurrent meningitis
INTRODUCTION
Cisternography with intrathecal gadolinium is defined as the magnetic resonance imaging (MRI) of the cerebrospinal system and associated structures after intrathecal administration of contrast material into the subarachnoid space.[
In CE-MRC, visualization of leakage in T1 of hyperintense contrast images with fat suppression is sufficient for the diagnosis of CSF leaks.[
The precise preoperative leakage site identification is crucial for surgical approach and increases the success rate of surgery while reducing the risk of complications. The primary reason for the repair of CSF leaks is that the overall risk of meningitis in patients with persistent CSF rhinorrhea is 19%.[
Mondini dysplasia is a congenital malformation of the inner ear most commonly associated with CSF fistula in the temporal bone in children.[
CASE REPORT
A 34-year-old female, right handed, with a 2-year history of “intermittent right unilateral hyaline rhinorrhea,” was admitted to our hospital with headaches, vomiting, and consciousness deterioration. A diagnosis of acute meningitis caused by Streptococcus pneumoniae was made, and specific antibiotic treatment was started with excellent results. After the total recovery a CT cisternography (CTC) was performed and the study concluded that the leak came from the cribriform plate to the right ethmoid sinus. An endoscopic exploration of the nasal cavity with fluorescein, in an attempt to closure the leak, revealed no defect in the ethmoidal roof, but leakage from the right Eustachian tube was detected. In that scenario, a second review of CTC suspected a defect at the floor of the middle fossa coming into the oval window. So, a right temporal craniotomy was performed with detachment of some adhesions of dura to the floor with cribriform-like structures and was covered with temporal fascia. However, the patient continued with CSF rhinorrhea and intermittent retronasal discharge as well as symptoms of intracranial hypotension, so it was decided to expand the diagnostic approach.
A CE-MRC was done. The technique has been well described in the literature.[
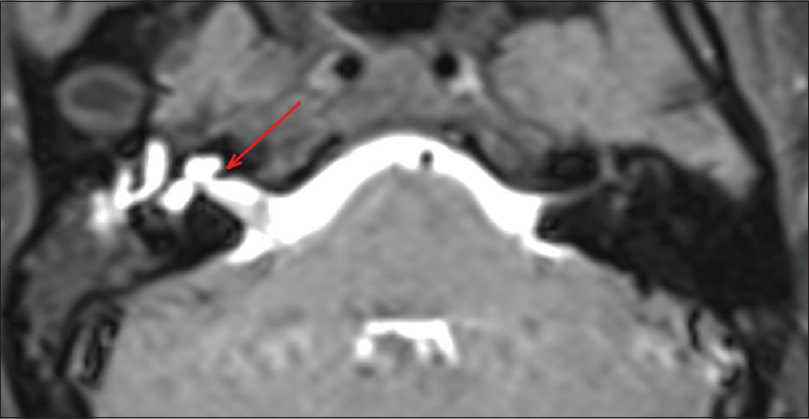
The study showed that the contrast completely filled up the inner ear and went into the middle ear and Eustachian tube; in subsequent acquisitions, it was possible to observe a path that connected to the inner ear with the middle ear located near the oval window [
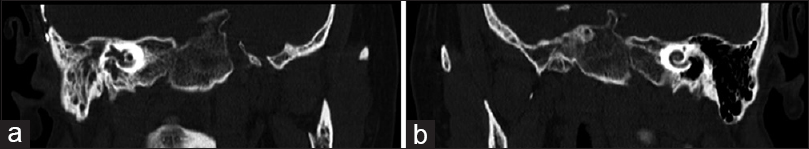
After detecting the CSF leak from the inner ear, a CT scan of the temporal bones was performed and the typical Mondini deformity of the right cochlear apex was identified, formed by cystic enlargement of the vestibular aqueduct [
A right subtotal petrosectomy was performed detecting the fistula in the right bony labyrinth, which was closed with fat and fascia from the temporal region. There have been no new episodes of meningitis or CSF leak up-to-date.
DISCUSSION
Currently, the most widely accepted method for evaluation of patients with suspected CSF leak is the combination of high-resolution CT with contrast cisternography. However, though CT images of thin sections are useful in visualizing bone defects, they may be limited in patients with multiple fractures or intermittent CSF leak.[
On the contrary, with nonenhanced MRC, the leak is characterized by a hyperintense path between the subarachnoid space and sinu-nasal space.[
The CE-MRC with intrathecal gadolinium is a minimally invasive procedure compared to other cisternographic and ventriculographic tests (radionuclide or MRI ventriculography) with the advantages of using MRI images, and, unlike the cisternography without contrast, provides not only morphological but also physiological information.[
Although intrathecal injection of gadolinium-DTPA (gadopentetate dimeglumine) is not approved by the Food and Drug Administration, preliminary clinical studies have reported the success of this method in locating CSF fistulas for patients with rhinorrhea.[
Intrathecal gadolinium-enhanced MRC was first performed in laboratory animals in 1985 by Di Chiro et al.[
Although “gadolinium encephalopathy” has been reported in patients with renal impairment,[
Also gadolinium-DTPA is the safest and most recommended contrast in human studies.[
In a study conducted in 2008 by Aydin et al., a sensitivity of 84% for locating CSF leaks was reported for CE-MRC after evaluating 44 patients with rhinorrhea, 43 of whom results were confirmed during surgery. No patient had adverse reactions related to the study (only headache which resolved with analgesic use in 24% of patients) or neurological symptoms during an average follow-up of 4 years.[
The CE-MRC also allows to identify spinal leaks in patients with spontaneous intracranial hypotension, as shown by Vanopdenbosch et al., in a prospective observational cohort study, who found a spinal epidural leak mainly at the cervicodorsal junction in 9 of 14 patients with spontaneous intracranial hypotension,[
In cases of patients with CSF fistula outside the skull, Chazen et al. found a leak at CE-MRC in 9 of 24 patients (38%) but in only 3 of 24 (13%) patients with CTC (P = 0.011). CT myelography did not identify any leaks that were not found on CE-MRC.[
In the case of our patient, MRC with intrathecal contrast helped identify the origin of the CSF fistula without any adverse events associated with the study, and this helped, in turn, through a detailed analysis of the anatomy of the inner ear via a high-resolution scan of the temporal bone, in the detection of the Mondini dysplasia associated fistula.
Mondini deformity refers to the absence of apical modiolus and interscalar septum, resulting in an incomplete segmentation of the cochlea and enlarged vestibular aqueduct and dilated vestibule.[
The fistula associated with Mondini dysplasia usually presents with rhinorrhea if the tympanic membrane is intact, as was the case of our patient.
In our patient, despite having a congenital malformation of the inner ear, Mondini dysplasia, curiously, the meningoencephalic infections did not begin until 10 years of age. The literature reports that about two-thirds of cases with congenital fistulas begin with these recurrent infections before 18 months of age.[
Managing Mondini dysplasia depends on the clinical presentation. In the case of a fistula tract, after locating your site, closure of the defect as soon as possible is indicated. Adipose tissue was used in our case, to fill the vestibule which was reinforced with a temporal fascia implant, and the middle ear was obliterated with abdominal adipose tissue. Although it is reported that recurrence after surgical repair occurs in 30–60% of the patients,[
CONCLUSION
The radiological identification of the site of CSF leak through sensitive imaging studies such as MRC with intrathecal gadolinium is crucial for surgical approach. Also, the successful repair of CSF leaks is important to prevent damage and repeated episodes of meningitis. The Mondini dysplasia should be included in the differential diagnosis of a patient with recurrent bacterial meningitis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akbar JJ, Luethmer PH, Schwartz KM, Hunt CH, Diehn FE, Eckel LJ. The Role of MR Myelography with Intrathecal Gadolinium in Localization of Spinal CSF Leaks in Patients with Spontaneous Intracranial Hypotension. Am J Neuroradiol. 2012. 33: 535-40
2. Albayram S. Gadolinium-enhanced MR Cisternography to Evaluate Dural Leaks in Intracranial Hypotension Syndrome. AJNR AM J Neuroradiol. 2008. 29: 116-21
3. Algin O, Hakyemez B. Phase-contrast MRI and 3D-CISS versus Contrast-enchanced MR Cisternography on the Evaluation of the Aqueductal Stenosis. Neuroradiology. 2010. 59: 99-108
4. Algin O, Hakyemez B. Phase-contrast MRI and 3D-CISS versus Contrast-enhanced MR Cisternography for the Detection of Spontaneous Third Ventriculostomy. J Neuroradiol. 2011. 38: 98-104
5. Algin O, Hakyemez B. The contribution of 3D-CISS and Contrast-enhanced MR Cisternography in Detecting Cerebrospinal Fluid leak in Patients with Rhinorrhoea. Br J Radiol. 2010. 83: 225-32
6. Algin O, Taskapilioglu O. Detection of CSF leaks with Magnetic Resonance Imaging in Intracranial Hypotension Syndrome. J Neuroradiol. 2011. 38: 175-77
7. Algin O, Turkbey B. Intrathecal Gadolinium-Enhanced MR Cisternography: A Comprehensive Review. AJNR Am J Neuroradiol. 2013. 34: 14-22
8. Arbelaez A, Medina E, Rodríguez M, Londoño AC, Castillo M. Intrathecal Administration of Gadopentetate Dimeglumine for MR Cisternography of Nasoethmoidal CSF Fistula. AJR. 2007. 188: W560-4
9. Arlt S, Cepek L. Gadolinium encephalopathy due to accidental intrathecal administration of gadopentetate dimeglumine. J Neurol. 2007. 254: 810-2
10. Aydin K, Guven K, Sense S, Jinkins JR, Minareci O. MRI cisternography with gadolinium-containing contrast medium: Its role, advantages and limitations in the investigation of rhinorrhoea. Neuroradiology. 2004. 46: 75-80
11. Aydin K, Terzibasioglu E. Localization of Cerebrospinal Fluid Leaks by Gadolinium-Enhanced Magnetic Resonance Cisternography: A 5-year single-center experience. Neurosurgery. 2008. 62: 584-9
12. Chazen JL, Talbott JF, Lantos JE, Dilon WP. MR Myelography for Identification of Spinal CSF Leak in Spontaneous Intracranial Hypotension. Am J Neuroradiol. 2014. 35: 2007-12
13. Daudia A, Biswas D, Jones NS. Risk of Meningitis with Cerebrospinal Fluid Rhinorrhea. Ann Otol Rhinol Laryngol. 2007. 116: 902-5
14. Di Chiro, Knop RH, Girton ME, Dwyer AJ, Doppman JL, Patronas NJ. MR Cisternography and Myelography with GD-DTPA in Monkeys. Radiology. 1985. 157: 373-7
15. Goel G, Ravishankar S. Intrathecal gadolinium-enhanced magnetic resonance cisternography in cerebrospinal fluid rhinorrhea: Road ahead?. J Neurotrauma. 2007. 24: 1570-5
16. Herther C, Schindler R. Mondini dysplasia with recurrent meningitis. Laryngoscope. 1985. 95: 655e8-
17. Jackler R, Luxford W. Congenital malformations of the inner ear: A classification based on embryogenesis. Laryngoscope. 1987. 97: 2-14
18. Jinkins J, Rudwan M. Intrathecal gadolinium-enhanced MR cisternography in the evaluation of clinically suspected cerebrospinal fluid rhinorrhea in humans: Early experience. Radiology. 2002. 222: 555-9
19. Kline M. Review of recurrent bacterial meningitis. Pediatr Infect Dis J. 1989. 8: 630-4
20. Maramattom BV, Manno EM, Wijdicks EFM, Lindell EP. Gadolinium encephalopathy in a patient with renal failure. Neurology. 2005. 64: 276-8
21. Miyamoto R, Robbins A. Cochlear implantation in the Mondini inner ear malformation. Am J Otol. 1986. 7: 258e61-
22. Mondini C. Anatomia surdi nati sectio: De Bononiensi Scientiarum et Artium Institute atque Academia commentarii. Bononiae. 1971. 7: 419-28
23. Ray D, Cavanagh J. Neurotoxic effects of gadopentetate dimeglumine: Behavioral disturbance and morphology after intracerebroventricular injection in rats. AJNR Am J Neuroradiol. 1996. 17: 365-73
24. Selcuk H, Albayram S. Intrathecal gadolinium enhanced MR cisternography in the evaluation of CSF leakage. AJNR Am J Neuroradiol. 2010. 31: 71-5
25. Shetty Shroff MM, Sahani DV, Kirtane MV. Evaluation of high resolution CT and MR cisternography in the diagnosis of cerebrospinal fluid fistula. Am J Neuroradiol. 1998. 19: 633-9
26. Small M, Cox M, Johnson A, Dornhoffer J. Cerebrospinal fluid otorrhea secondary to non-otogenic meningitis in a child with Mondini dysplasia. Otolaryngol Case Rep. 2017. 2: 16-8
27. Stone J, Castillo M. Evaluation of CSF leaks: High- resolution CT compared with contrast-enhanced CT and radionuclide cisternography. AJNR Am J Neuroradiol. 1999. 20: 706-12
28. Tali ET, Ercan N, Krumina G, Rudwan M, Mironov A, Zeng QY. Intrathecal gadolinium (gadopentetate dimeglumine) enhanced magnetic resonance myelography and cisternography: Results of a multicenter study. Invest Radiol. 2002. 37: 152-9
29. Tyagi I, Syal R. Cerebrospinal fluid otorhinorrhea due to inner ear malformation: Clinical presentation and new perspectives in management. J Laryngol Otol. 2005. 119: 714e8-
30. Vanopdenbosch LJ, Dedeken P, Casselman JW, Vlaminck SA. MRI with intrathecal gadolinium to detect a CSF leak: A prospective open-label cohort study. J Neurol Neurosurg Psychiatry. 2011. 82: 456-8
31. Wenzel R, Leppien A. Gadolinium-myelocisternography for cerebrospinal fluid rhinorrhoea. Neuroradiology. 2000. 42: 874-80
32. Yilmaz C, Bayram N. A case of Mondini dysplasia with recurrent Streptococcus pneumonia meningitis. Eur J Pediatr. 2009. 168: 1533-5
33. Zeng Q, Xiong L, Jinkins JR, Fan Z, Liu Z. Intrathecal gadolinium enhanced MR myelography and cisternography. Am J Roentgenol. 1999. 173: 1109-15