- Radioneurosurgery Unit, National Institute of Neurology and Neurosurgery, “Dr. Manuel Velasco Suarez”, Mexico City, Mexico
- Neurosurgery Department, Medical Center, “Adolfo Lopez Mateos”, Health Institute of Mexico State. Toluca, Mexico State, Mexico
- Neurosurgery Department, American British Cowray Medical Center, Mexico City, Mexico
Correspondence Address:
Gutierrez Aceves Guillermo Axayacalt
Radioneurosurgery Unit, National Institute of Neurology and Neurosurgery, “Dr. Manuel Velasco Suarez”, Mexico City, Mexico
DOI:10.4103/2152-7806.193728
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Guillermo Axayacalt GA, Alejandro CE, Marcos RA, Milton Inocencio RF, Jose Alfredo HG. Brain hemorrhage after electrical burn injury: Case report and probable mechanism. Surg Neurol Int 09-Nov-2016;7:
How to cite this URL: Guillermo Axayacalt GA, Alejandro CE, Marcos RA, Milton Inocencio RF, Jose Alfredo HG. Brain hemorrhage after electrical burn injury: Case report and probable mechanism. Surg Neurol Int 09-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/brain-hemorrhage-electrical-burn-injury-case-report-probable-mechanism/
Abstract
Background:High-voltage electric injury may induce lesion in different organs. In addition to the local tissue damage, electrical injuries may lead to neurological deficits, musculoskeletal damage, and cardiovascular injury. Severe vascular damage may occur making the blood vessels involved prone to thrombosis and spontaneous rupture.
Case Description:Here, we present the case of a 39-year-old male who suffered an electrical burn with high tension wire causing intracranial bleeding. He presented with an electrical burn in the parietal area (entry zone) and the left forearm (exit zone). The head tomography scan revealed an intraparenchimatous bleeding in the left parietal area. In this case, the electric way was the scalp, cranial bone, blood vessels and brain, upper limb muscle, and skin. The damage was different according to the dielectric property in each tissue. The injury was in the scalp, cerebral blood vessel, skeletal muscle, and upper limb skin. The main damage was in brain’s blood vessels because of the dielectric and geometric features that lead to bleeding, high temperature, and gas delivering.
Conclusion:This is a report of a patient with an electric brain injury that can be useful to elucidate the behavior of the high voltage electrical current flow into the nervous system.
Keywords: Brain, burn, electrical, injury, hemorrhage
BACKGROUND
High-voltage electric injury may induce lesions in different organs.[
Neurological damage is a common complication. The reported neurological complications include cerebral injury, spinal cord lesions, peripheral nerve injuries, and motor neuropathies depending on the injury site.[
Here, we describe a patient who underwent high-voltage cranial electrical injury and brain hemorrhage.
CASE DESCRIPTION
Our case is about a 39-year-old male, who suffered an electrical burn with high tension wires that caused an intraparenchimal bleeding. The patient was working on the ceiling of a house when he received an electrical discharge on his head. A high voltage wire touched his head, after which, he lost awareness without recovery. He received primary care by paramedic personal, who found the patient with 6 points on the Glasgow Coma Scale (GCS). He was sedated with advanced airway manage and was sent to our medical center. He arrived under the effect of sedation, with the Ramsay scale of 6, therefore, he continued under sedation and with mechanical-assisted ventilation.
On physical examination, he presented an electrical burn in the parietal area (entry zone) with a diameter of approximately 8 cm [
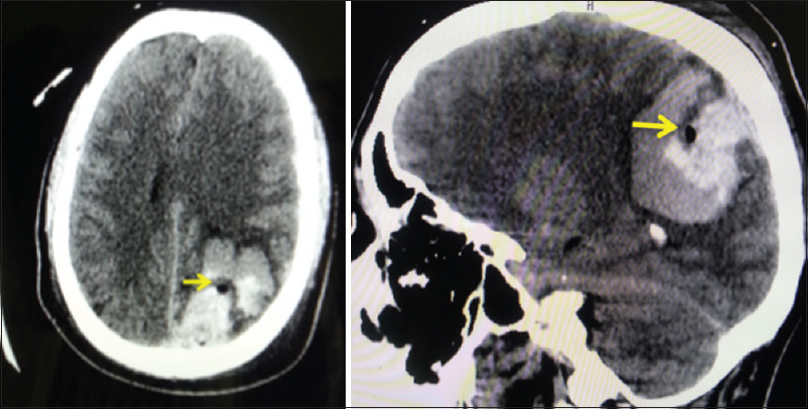
The head tomography scan revealed an intraparenchimatous bleeding in the left parietal area, under the entry zone, with gas density inside the hemorrhage [
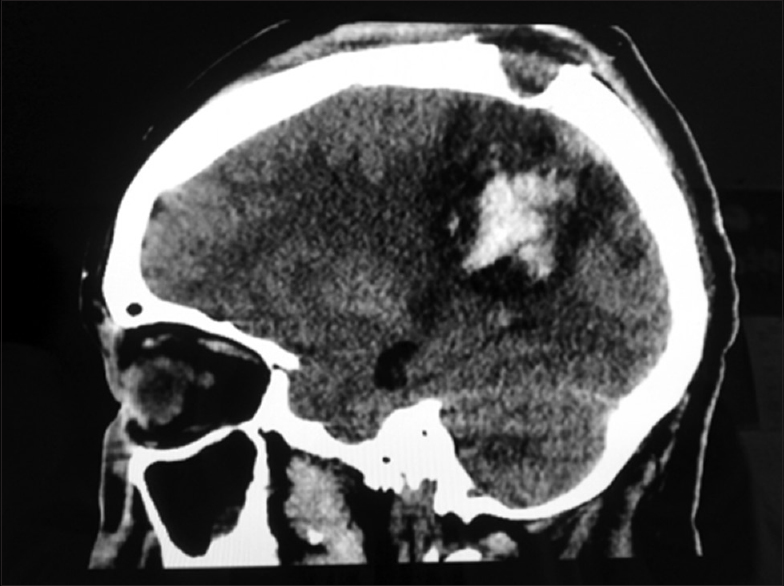
The control tomography scan showed the subtotal evacuation of the hemorrhage and the recovery of midline structures [
After surgery, he stayed in the intensive care unit (ICU) for 5 days where he presented renal failure secondary to rhabdomyolysis. During the ICU monitoring, he had satisfactory evolution. He was extubated and discharged to our hospitalization service, where he stayed for 5 days to complete antibiotic treatment. He was discharged from our hospital with 15 points in the GCS and the skin lesions in epithelialization phase.
The clinical effects of electric injury may be classified into immediate and late manifestations. The immediate manifestations include cardiac and respiratory arrest, loss of consciousness, motor and sensory disturbances, amnesia, and confusion. The late manifestations may be divided into focal and nonfocal deficits and may occur days to months after the electric injury. Focal deficits include cerebral (hemiplegia, aphasia), spinal (transverse myelitis, progressive muscular atrophy, amyotrophic lateral sclerosis), and peripheral nerve (neuropathies, radiculopathies) manifestations. Nonfocal symptoms such as psychoneurotic behavior, personality changes, confusion, amnesia, and headache are common, and their occurrence is not restricted to cases in which the brain lies in the electric current pathway. Abnormal electroencephalograms (EEGs) have been documented in cases in which the brain is outside the current pathway.[
Although the exact mechanism of nerve injury has not been explained, both direct injury by electrical current and/or a vascular cause receive the most attention.[
Four theories have been considered to explain the histopathological findings of electric injury. (1) The electrostatic theory suggests that, if the victim is not grounded, electric charges build up in the body, producing electrostatic effects. Particles with similar charges repel each other, resulting in a sudden expansive force of the body tissues that raises waves of decompression under the skin. This may account for the tissue rupture seen in autopsy, however, it does not explain the unilateral predominance of clinical effects or abnormalities beyond the current pathway. (2) The vascular theory suggests vasoconstriction as the mechanism of the acute manifestations. Initial injuries and subsequent vascular thrombosis may account for the delayed manifestations. Animal studies have shown that pial vessels constrict when exposed to electric stimulation. (3) The mechanical theory suggests that the injury is caused by a violent jarring of the tissue because of the electrical current. (4) The heat theory suggests thermal injury to the brain tissue as the mechanism of the pathological findings. Cerebrospinal fluid temperatures as high as 145°F have been recorded 5 hours after legal electrocution.[
Electrical injury results in direct damage of the tissue because of the electric current and subsequent heat generation. The amount of direct damage depends primarily on the intensity of the current. Ohm’s law states that this current is proportional to the voltage and inversely proportional to the resistance of the tissue. Although we would expect the current density to be higher in nerves and blood vessels because of the low resistance, the tissues act as a volume conductor, with the composite resistance of all the tissue components.
The heat that is generated by the passage of the current can be quantified with Joule’s law, which states that heat is proportional to square of the voltage and inversely proportional to the resistance of the conductor.
Although the resistance and voltage are important for determining the current and the heat generated, other factors that determine the clinical injury include the duration of contact with the conductor and the pathway of the current’s flow. Heat generation due to the passing current causes direct damage to the tissues. Robson et al. demonstrated that electrical injuries result in elevated levels of thromboxane A2. The high thromboxane A2 levels contribute to progressive tissue necrosis by causing vasoconstriction and thrombosis in the microcirculation. Partial or complete vessel occlusion may occur at the time of the injury, especially in smaller nutrient arteries, and delayed arterial thrombosis may also occur. Electrical injury to blood vessels causes varying degrees of damage to different layers of the vessel. Wang et al. examined aorta and pulmonary artery endothelial cells from electrocution victims and found that cell membrane perforations were present within 24 hours of the electrical injury, whereas after 24 hours, the endothelium disintegrated. Jaffe et al. found that electrical injury caused a complete loss of endothelial cells. The muscle fibers of the media were more sensitive to electric current, whereas the adventitia showed little change. The vessels lost their elasticity, and fusiform aneurysms were common.[
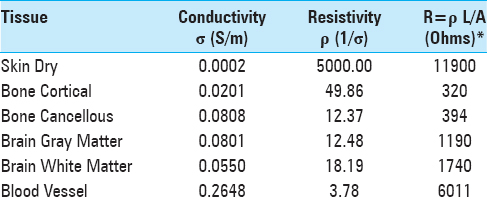
Human body can transport electric current, but in an electric shock situation, similar to the case presented here, current distribution through the body depends specifically on each person as well as on the circumstances of the electric shock. Although dielectric properties of tissue have been described, particular circumstances play a major role in electrical injury, i.e., skin resistance, voltage breakdown of skin, contact area with source voltage, distance between points of contact, and of course source voltage. According to our patient’s set of images, we can try to study the current distribution and possibly the tissue injury in the first centimeters depth, from the contact point in his head. First, let us consider the dielectric properties of tissue shown in
In a macroscopic approach, these properties can be used to analyze the different tissue behavior as a resistive element of current transport; hence, we can present a biological system injury which will have circuit properties of both serial and parallel circuits.
Therefore, the electric power (P = I2 × R, from Ohm’s law) is a helpful measurement to compare the role of each resistive element in this biological circuit system, taking into account specific dielectric and geometrical properties we can estimate power deposition.
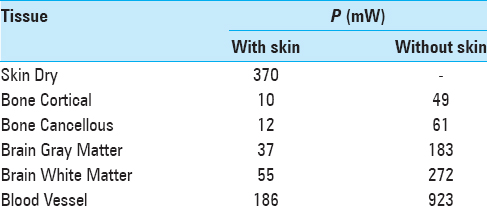
According to power values shown in
In our case, the injury must be secondary to mixed sources, mainly the heat generation hypothesis, i.e. the electric current passing through different tissue resistance damages the vascular tissue, that was the bleeding source, and the heat generation was capable to disrupt the chemical interaction between the oxygen and the hemoglobin. The high temperature leaves the accumulation of gas density in to the hematoma [
In this case, the electric route was the scalp, cranial bone, blood vessels and brain, upper limb muscle, and skin. The damage was different according to the dielectric property of each tissue. The injury was in the scalp, cerebral blood vessel, skeletal muscle, and upper limb skin.
The main damage was in the brain’s blood vessels because of the dielectric and geometric features, leading to bleeding, high temperature, and gas delivering (maybe oxygen or carbon dioxide, delivered from the hemoglobin). It is remarkable to mention that although the blood vessel and brain tissue had similar calorific capacity, the blood vessel has higher resistance and it leads to higher temperature than the brain tissue.
CONCLUSION
This is a report of a patient with electric brain injury that can be useful to elucidate the behavior of the high voltage electrical current flow into the nervous system.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andreuccetti DFossi RPetrucci CLast accessed on 2016 Oct 21. Available at: http://niremf.ifac.cnr.it/tissprop/ .
2. Baumann SB, Wozny DR, Kelly SK, Meno FM. The electrical conductivity of human cerebrospinal fluid at body temperature. IEEE Trans Biomed Eng. 1997. 44: 220-3
3. Erkin G, Akinbingöl M, Uysal H, Keles I, Aybay C, Ozel S. Delayed cervical spinal cord injury after high voltage electrical injury: A case report. J Burn Care Res. 2007. 28: 905-8
4. Gabriel S, Lau RW, Gabriel C. The dielectric properties of biological tissues: II. Measurements in the frequency range 10 Hz to 20 GHz. Phys Med Biol. 1996. 41: 2251-69
5. Isao T, Masaki F, Riko N, Seiichi H. Delayed Brain Atrophy After Electrical Injury. J Burn Care Rehabil. 2005. 26: 456-8
6. Morgenstern LB, Hemphill JC, Anderson C, Becker K, Broderick JP, Connolly ES. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010. 41: 2108-29
7. Patel A, Lo R. Electric injury with cerebral venous thrombosis. Case report and review of the literature. Stroke. 1993. 24: 903-5
8. Patrick RJ.editors. Applied Bioelectricity. From Electrical Stimulation to Electropathology. Springer; 1998. p. 20-53
9. Scholz T, Rippmann V, Wojtecki L, Perbix W, Rothschild MA, Spilker G. Severe brain damage by current flow after electrical burn injury. J Burn Care Res. 2006. 27: 917-22
10. Spies M, McCauley RL, Mudge BP, Herndon DN. Management of acute calvarial burns in children. J Trauma. 2003. 54: 765-9
11. Toy J, Ball BJ, Tredget EE. Carotid rupture following electrical injury: A report of two cases. J Burn Care Res. 2012. 33: e160-5