- Department of Neurosurgery, PGIMER, Chandigarh, India
- Department of Histopathology, PGIMER, Chandigarh, India
Correspondence Address:
Ankur Kapoor
Department of Histopathology, PGIMER, Chandigarh, India
DOI:10.4103/2152-7806.185009
Copyright: © Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Singla N, Kapoor A, Chatterjee D. Diagnosing early upward cerebellar herniation by computed tomography: A diagnostic boom, a savior. Surg Neurol Int 29-Jun-2016;7:72
How to cite this URL: Singla N, Kapoor A, Chatterjee D. Diagnosing early upward cerebellar herniation by computed tomography: A diagnostic boom, a savior. Surg Neurol Int 29-Jun-2016;7:72. Available from: http://surgicalneurologyint.com/surgicalint_articles/diagnosing-early-upward-cerebellar-herniation-computed-tomography-diagnostic-boom-savior/
Sir,
Preoperative diversion of cerebrospinal fluid (CSF) is a common procedure for posterior fossa lesions. Although rare in incidence, upward cerebellar herniation may occur after such procedures, and is associated with a high mortality. Most of these patients present with sudden apnea and neurological deterioration with imaging showing dense intratumoral hemorrhage.[
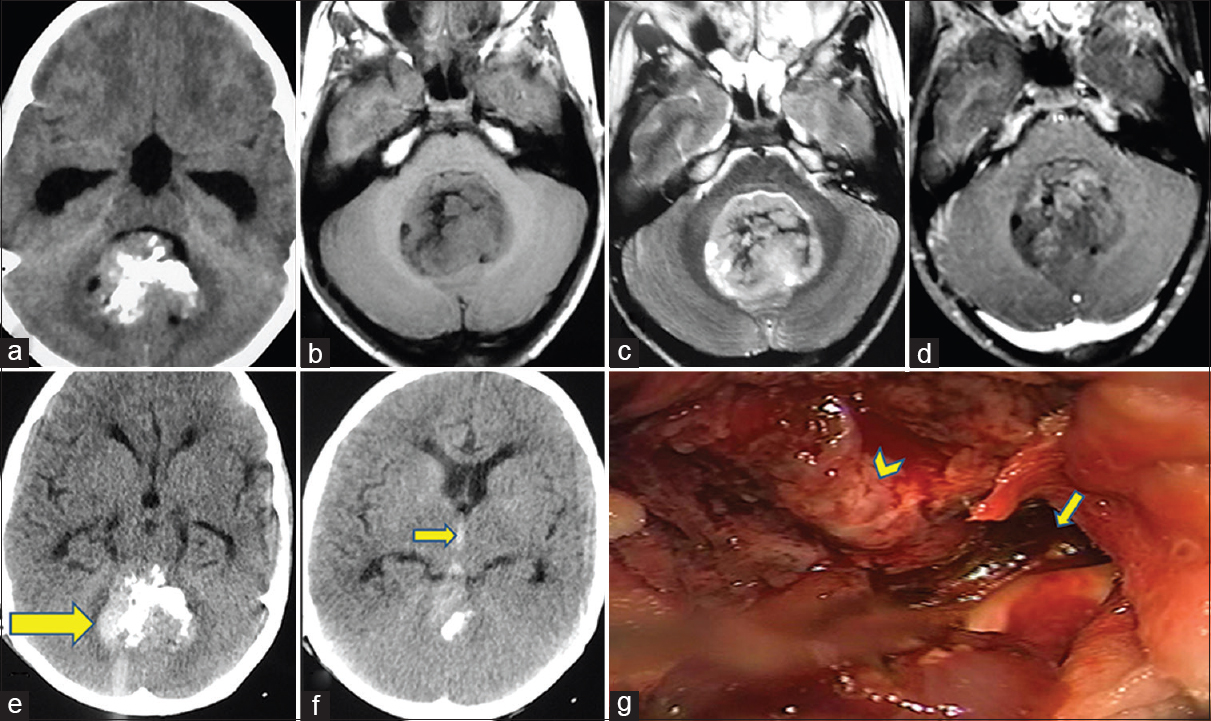
A 10-year-old male presented with the history of headache and gait imbalance for 3 weeks. Examination revealed gait ataxia, dysmetria, and papilloedema. CT scan suggested a midline cerebellar lesion. Magnetic resonance imaging (MRI) revealed a vermian lesion that appeared hypointense on T1-weighted (T1W) image, hyperintense on T2W image with focal hypointensity, and slight enhancement on Gadolinium. Associated mass effect on the brainstem with hydrocephalus was remarkable and so was the focal calcification [
Figure 1
(a) Computed tomography (CT) axial image showing midline cerebellar lesion with hydrocephalus. (b-d) T1-weighted plain, T2-weighted (T2W), and T1-weighted (T1W) contrast axial magnetic resonance images showing vermian lesion hypointense on T1W (b), hyperintense on T2W (c), and faint enhancement (d). (e-f) Post shunt surgery noncontrast CT axial images showing intratumoral hemorrhage (arrow) (e) and intraventricular hemorrhage (arrow) (f). (g) Intraoperative photograph confirming tumor at the roof of fourth ventricle (arrowhead) and clot at anterior aspect near brainstem and aqueduct (arrow)
Spontaneous hemorrhage in intracranial tumors is a known phenomena, the mechanisms of which are varied. It accounts for up to 6–10% of all intracranial hemorrhage.[
The CSF diversion in such cases can be done by VP shunt, external ventricular drain (EVD), and endoscopic third ventriculostomy (ETV). Although, theoretically, VP shunt is better than EVD by providing guarded decompression of ventricles, EVD has its own merits as the CSF output can be carefully monitored and controlled in the inpatient setting. In addition, the CSF diversion with an EVD can be turned off more rapidly than with a VP shunt in the event of symptomatic upward herniation. Furthermore, an EVD can potentially be removed after definitive treatment avoiding a permanent indwelling system. Similarly, ETV is helpful by avoiding the need of a permanent shunt, with the disadvantage being the loss of control of CSF diversion. We believe that any evidence of new onset bleeding within the tumor extending rostrally to supratentorial ventricles after CSF diversion must be considered a sign of upward herniation, despite no neurological worsening. An easily available investigation in the form of CT scan can occasionally provide early diagnosis. We emphasize on early suspicion in case of any new onset intratumoral or intraventricular hemorrhage because prompt action in the form of urgent definitive surgery can help in averting a tragic outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cuneo RA, Caronna JJ, Pitts L, Townsend J, Winestock DP. Upward transtentorial herniation: Seven cases and a literature review. Arch Neurol. 1979. 36: 618-23
2. Elgamal EA, Richards PG, Patel UJ. Fatal haemorrhage in medulloblastoma following ventricular drainage. Case report and review of the literature. Pediatr Neurosurg. 2006. 42: 45-8
3. Gurajala I, Brahmaprasad V, Rajesh A, Ramachandran G, Purohit AK. Reverse brain herniation following ventriculoperitoneal shunt. Indian J Anaesth. 2012. 56: 585-7
4. Kapoor A, Savardekar A, Tewari MK, Chatterjee D, Radotra BD. Spontaneous hemorrhages in pediatric supratentorial pilocytic astrocytomas. Malignant presentation of a benign entity. Childs Nerv Syst. 2015. 31: 1617-20
5. Vaquero J, Cabezudo JM, de Sola RG, Nombela L. Intratumoral hemorrhage in posterior fossa tumors after ventricular drainage. Report of two cases. J Neurosurg. 1981. 54: 406-8