- Division of Neurosurgery, Hôpital Notre-Dame du CHUM, University of Montreal, Montreal, Québec, Canada
- Division of Otolaryngology – Head and Neck Surgery, Hôpital Notre-Dame du CHUM, University of Montreal, Montreal, Québec, Canada
Correspondence Address:
Daniel Shedid
Division of Neurosurgery, Hôpital Notre-Dame du CHUM, University of Montreal, Montreal, Québec, Canada
DOI:10.4103/2152-7806.170450
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Weil AG, Shehadeh M, Ayad T, Abboud O, Shedid D. En bloc resection of a C2–C3 upper cervical chordoma: Technical note. Surg Neurol Int 25-Nov-2015;6:
How to cite this URL: Weil AG, Shehadeh M, Ayad T, Abboud O, Shedid D. En bloc resection of a C2–C3 upper cervical chordoma: Technical note. Surg Neurol Int 25-Nov-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/en-bloc-resection-of-a-c2-c3-upper-cervical-chordoma/
Abstract
Background:Recently, en bloc spondylectomy for upper cervical chordomas has been reported. Most authors utilize the combined approaches (e.g., transoral tumor resection with anterior column reconstruction and primary pharyngeal closure without up-front flap repair). However, the 60% incidence of posterior pharyngeal wall dehiscence delays oral intake, typically requires an additional surgery (e.g. free-flap), and delays radiation therapy.
Methods:Here, we demonstrate the efficacy of en bloc C2–C3 spondylectomy for the treatment of upper cervical chordomas utilizing a combined transoral followed by posterior approach. We used a novel anterior de-epithelialized submental island flap (SIF) as an underlay graft between the pharyngeal wall and cage/hardware to prevent pharyngeal wound dehiscence.
Results:Despite a small pharyngeal fistula, the construct healed and the patient was disease-free 40 months later.
Conclusion:En bloc C2–C3 spondylectomy for the treatment of an upper cervical chordoma typically requires a combined transoral and posterior approaches. This required utilization of an anterior SIF to promote adequate wound healing. This maneuver avoided incurring the typical complications of combined approaches (e.g. transoral tumor resection with anterior column reconstruction and primary pharyngeal closure without up-front flap repair).
Keywords: Chordoma, en bloc, oncology, spine, submental island flap
INTRODUCTION
Only 4–5% of chordomas arise in the cervical spine.[
CASE REPORT
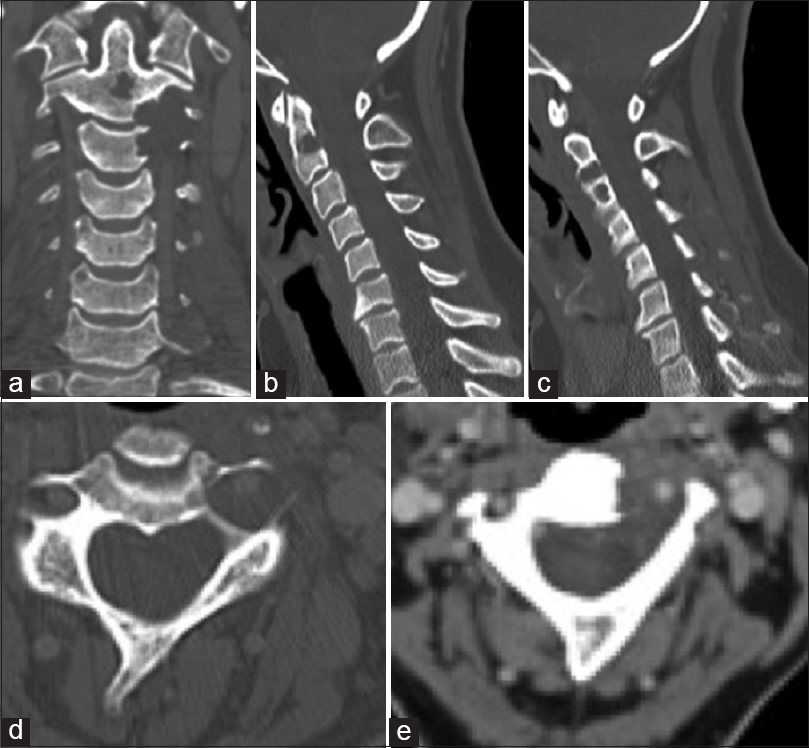
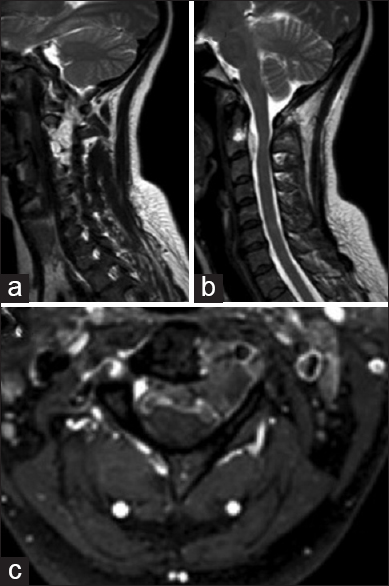
A 46-year-old female presented with neck and shoulder pain following a car accident. The cervical computed tomography (CT) scan and magnetic resonance imaging (MRI) studies revealed an osteolytic lesion involving the left C2 and C3 vertebral bodies. The lesion encased the left VA, and extended foraminally into the epidural space [Figures
Figure 1
Preoperative coronal (a), sagittal (b and c), and axial (d) computed tomography scan showing the bony lesion involving the bodies of C2 and C3, as well as the left C2 and C3 transverse foramina, which are widened. Computed tomography-angiogram (e) confirms the left vertebral artery which is a patent at both C2 and C3 and pushed anteriorly by the tumor
Figure 2
Preoperative sagittal T2-weighted image (a and b) showing the extension of the tumor from the left C2 and C3 vertebral body to the left epidural space. Axial T1-weighted magnetic resonance imaging with gadolinium (c) shows the left C2–C3 tumor involving the left C3 pedicle and transverse foramina
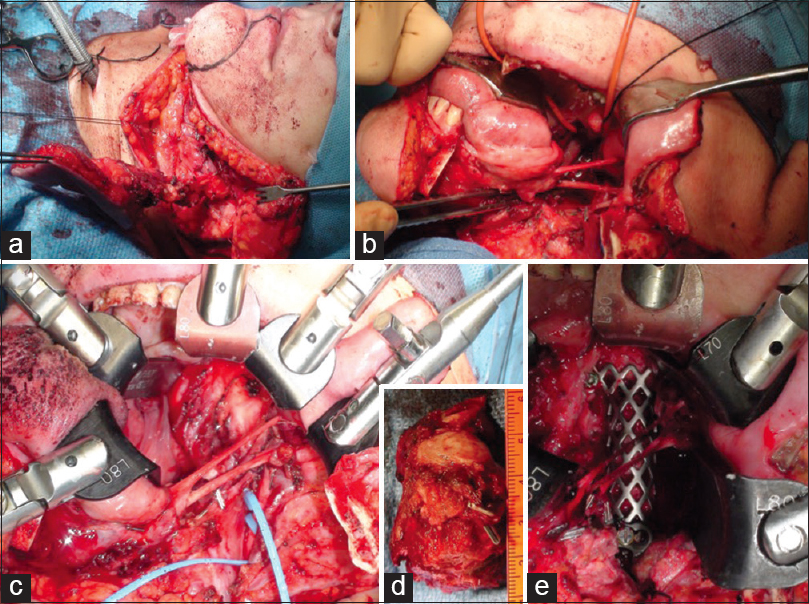
The second stage performed 1-week later involved securing the airway with a tracheotomy, exposing the upper spine from C1 to C5 utilizing a transoral transmandibular, and an extended anterior cervical approach, followed by C2, and C3 corpectomy. This facilitated en bloc resection of the tumor, and anterior column reconstruction with a Harms cage filled with allograft. Protection of the instrumentation with a submental flap, and refixation of the split mandible was followed by closure of the posterior pharyngeal wall and the neck incision [Figures
Figure 3
After preoperative embolization of left vertebral artery and posterior approach with C2–C3 laminectomy, left facetectomy and sectioning of the left C2 and C3 nerve roots and occipito-cervico-thoracic fusion, the patient underwent an anterior approach. Intraoperative photographs demonstrating the transoral/transmandibular/extended anterior cervical approach. A submental flap was included in the incision and later used to cover the hardware (a). The subaxial cervical spine was exposed following the mandibulotomy, submandibular gland resection, with the preservation of the lingual, hypoglossal and glossopharyngeal nerves (b). The upper cervical spine was exposed following the soft palate and posterior pharyngeal wall incision and retraction. With the synframe retractor in place, a wide anterior exposure extending from the mid-clivus to the level of C5 inferiorly was obtained (c). Following en bloc removal of the tumor (d), the anterior column was reconstructed with a titanium T-shaped Harms (e) which was fixed to the lateral masses of C1 with screws and buttressed in place on the body of C4 with an anterior plate extending from C4 to C5
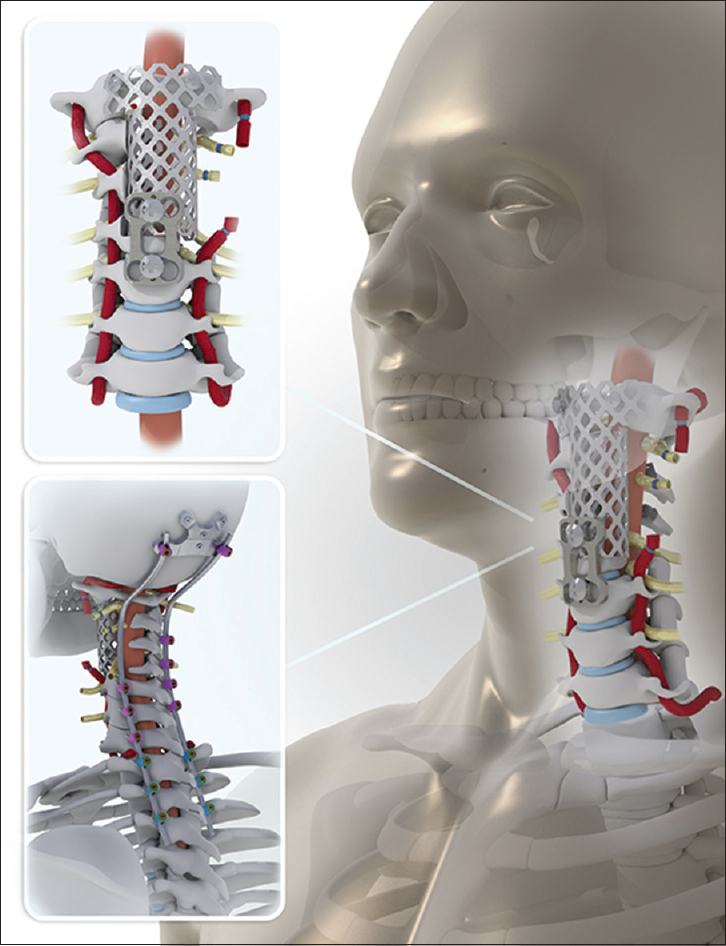
Figure 4
Lateral (a) anteroposterior (b) and oblique (c) cervical radiographs demonstrating the posterior occipito-cervico-thoracic instrumentation and anterior reconstruction with titanium mesh cage and C4–C5 anterior plate. The embolized left vertebral artery has been removed with the tumor expert for coils above and below the points of ligation (d) Computed tomography scan showing the C1 lateral mass screw through the T-shaped titanium cage (e) and C1 lateral mass
Postoperative morbidity following the second surgery included: Transient facial/glossal edema, ventilation until the seventh postoperative day due to the diaphragmatic weakness from C2–C3 nerve root sacrifice (which progressively resolved), and partial left eleventh nerve palsy. Thirty-five days after the second surgery (anterior approach), the patient underwent a third surgery to realign the head by about 15° posteriorly at the occipito-cervical junction utilizing a posterior approach. Severe dysphagia initially required a nasogastric tube and later a gastrostomy; 60 days later, she was finally started on oral feeding. At the final 40 months follow-up, the patient was functioning normally, including no deficits in speech and swallowing. The repeat cervical CT and MRI revealed no tumor recurrence.
DISCUSSION
Controversial en bloc spondylectomy
Controversy still exists regarding optimal constructs for en bloc C2 spondylectomy. In clinical series involving spondylectomy and reconstruction of the upper cervical spine, high pseudarthrosis rates of 14–66% have been reported.[
Intralesional resection
In upper cervical chordomas, intralesional resection with adjuvant radiation therapy is associated with a 40% recurrence and 67% mortality rate at 5 postoperative years.[
CONCLUSION
Upper cervical C2–C3 spine chordomas may be managed with en bloc stand-alone resection with negative (marginal) margins, accompanied by the up-front use of a de-epithelialized SIF to prevent the posterior pharyngeal wall dehiscence. Although this approach is associates with a high frequency of pre- and post-operative complications, several technical pearls may reduce the morbidity and potential mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bailey CS, Fisher CG, Boyd MC, Dvorak MF. En bloc marginal excision of a multilevel cervical chordoma. Case report. J Neurosurg Spine. 2006. 4: 409-14
2. Chou D, Acosta F, Cloyd JM, Ames CP. Parasagittal osteotomy for en bloc resection of multilevel cervical chordomas. J Neurosurg Spine. 2009. 10: 397-403
3. Cloyd JM, Chou D, Deviren V, Ames CP. En bloc resection of primary tumors of the cervical spine: Report of two cases and systematic review of the literature. Spine J. 2009. 9: 928-35
4. Guppy KH, Chakrabarti I, Isaacs RS, Jun JH. En bloc resection of a multilevel high-cervical chordoma involving C-2: New operative modalities: Technical note. J Neurosurg Spine. 2013. 19: 232-42
5. Hsieh PC, Gallia GL, Sciubba DM, Bydon A, Marco RA, Rhines L. En bloc excisions of chordomas in the cervical spine: Review of five consecutive cases with more than 4-year follow-up. Spine (Phila Pa 1976). 2011. 36: E1581-7
6. Jiang L, Liu ZJ, Liu XG, Ma QJ, Wei F, Lv Y. Upper cervical spine chordoma of C2-C3. Eur Spine J. 2009. 18: 293-8
7. Molina CA, Ames CP, Chou D, Rhines LD, Hsieh PC, Zadnik PL. Outcomes following attempted en bloc resection of cervical chordomas in the C-1 and C-2 region versus the subaxial region: A multiinstitutional experience. J Neurosurg Spine. 2014. 21: 348-56
8. Rhines LD, Fourney DR, Siadati A, Suk I, Gokaslan ZL. En bloc resection of multilevel cervical chordoma with C-2 involvement. Case report and description of operative technique. J Neurosurg Spine. 2005. 2: 199-205
9. Scheer JK, Tang J, Eguizabal J, Farin A, Buckley JM, Deviren V. Optimal reconstruction technique after C-2 corpectomy and spondylectomy: A biomechanical analysis. J Neurosurg Spine. 2010. 12: 517-24
10. Vassal F, Dumas B, Nuti C. Margin-free, en bloc resection of a multilevel cervical chordoma with C-2 involvement: Case report with 2-year follow-up and description of operative technique. Br J Neurosurg. 2012. 26: 929-31