- Division of Neurosurgery, Institute of Medical Research A. Lanari, University of Buenos Aires, Buenos Aires, Argentina
- Department of Pathology, Institute of Medical Research A. Lanari, University of Buenos Aires, Buenos Aires, Argentina
Correspondence Address:
Alejandra T. Rabadán
Department of Pathology, Institute of Medical Research A. Lanari, University of Buenos Aires, Buenos Aires, Argentina
DOI:10.4103/2152-7806.195566
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alejandra T. Rabadán, Diego Hernandez, Leonardo Paz. Extent of resection and postoperative functional declination of Klekamp's type A intramedullary tumors in adult patients. 12-Dec-2016;7:
How to cite this URL: Alejandra T. Rabadán, Diego Hernandez, Leonardo Paz. Extent of resection and postoperative functional declination of Klekamp's type A intramedullary tumors in adult patients. 12-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/extent-of-resection-and-postoperative-functional-declination-of-klekamps-type-a-intramedullary-tumors-in-adult-patients/
Abstract
Background:The most commonly primary intramedullary spinal cord tumors (ISCT) in adults are the noninfiltrative lesions, corresponding to Klekamp's type A classification. There are few reports exclusively considering this type of lesions, their resectability and postoperative functional declination risk, and to our knowledge, none from Latin America. This led us to evaluate our results to provide information that might contribute to the decision making process in our region.
Methods:A retrospective observational study was conducted comprising a cohort of 21 adults having primary Klekamp's type A ISCT. Diagnosis was made by magnetic resonance imaging (MRI), along with diffusion tensor/tractography in the last 7 cases. Preoperative functional status was assessed using the McCormick's modified scale (mMs), which was also used for the postoperative assessment within postoperative 90 days period. MRI was used to confirm the extent of resection.
Results:Radical resection was obtained in 20/21 cases. The postoperative functional status was stable in 42.8% of the cases, and in 57.4% was even better than in the preoperative period. Temporary declination was observed in 2 cases in the early postoperative period. There were 2 cases with complications; one patient had cerebrospinal fluid fistula with meningitis, which was conservatively resolved, and another patient died from pulmonary embolism.
Conclusion:Although the number of patients in this series does not allow to conclude from a statistical point of view, the outcomes showed that the modern surgery of Klekamp's type A ISCT permits a complete resection with low functional declination risk.
Keywords: Intramedullary tumor, spinal cord tumor, surgical results
INTRODUCTION
The incidence of primary spinal cord tumors both extra and intramedullary is 74 in 100,000 people per year. Among them, only purely intramedullary spinal cord tumors (ISCT) amount to 30%.[
ISCTs in adults usually appear during the productive stages of life, they manifest deceptively, and although their growth is often slow, their progress is unvaryingly constant, generally leading to serious and incapacitating neurological deficits unless they receive treatment.[
According to Klekamp's classification, there are three types of ISCTs, namely, type A, noninfiltrative; type B, infiltrative; and type C. Taking into account the literature, approximately 70% correspond to type A and are represented by the ependymoma as the most common tumor, followed by a heterogeneous group of other lesions such as malignant neuroepithelial tumors, cavernomas, hemangioblastomas, dermoid, and epidermoid cysts.[
There are few reports considering exclusively the Klekamp's type A ISCT, their resectability and postoperative functional declination risk, and to our knowledge, none from Latin America. This led us to evaluate our results to provide information that might contribute to the decision-making process in our region.
MATERIALS AND METHODS
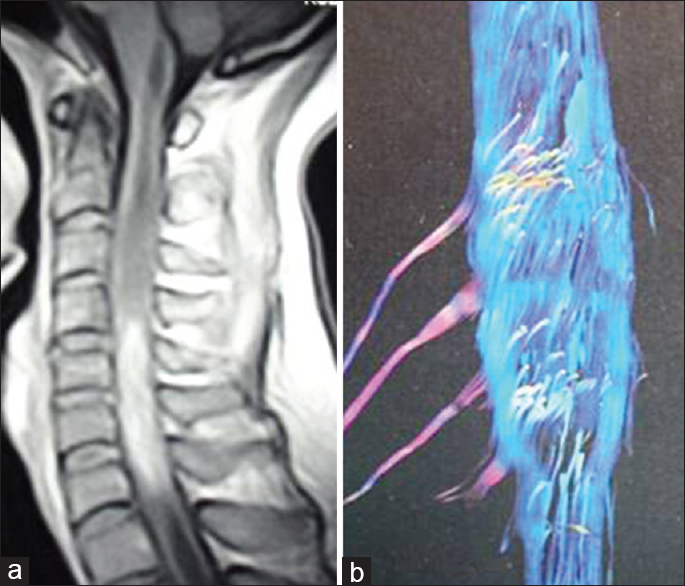
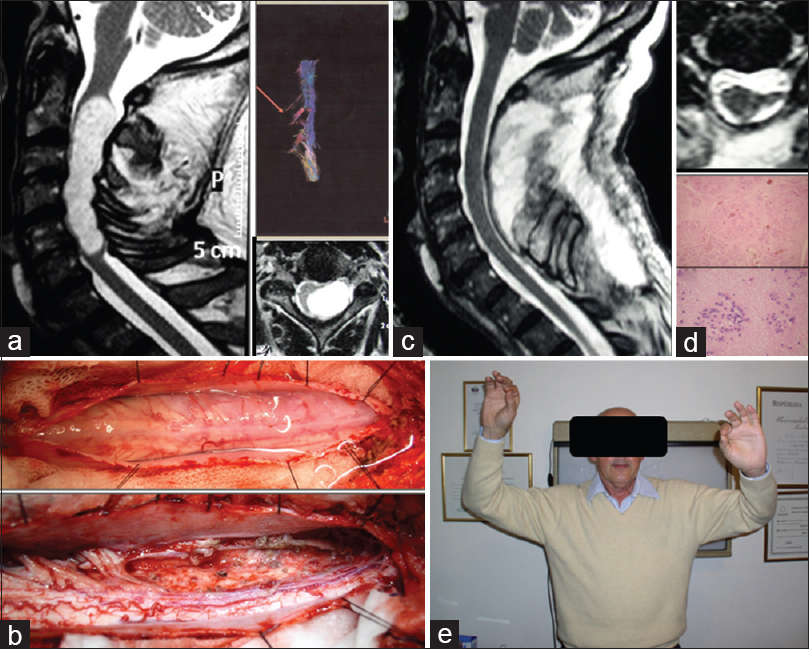
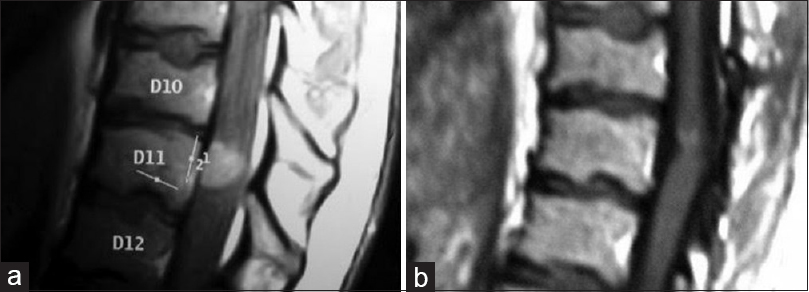
A retrospective study was conducted comprising a cohort of 21 adult patients having lesions corresponding to type A in Klekamp's classification, who were treated from 1998 to 2015 by the senior author (ATR). The lesions were diagnosed through gadolinium magnetic resonance imaging (Gd MRI) and through MR diffusion tensor/tractography in the last 7 cases [
The surgical approach was by laminectomy and laminoplasty on the last 7 patients. Spinal cord surgery was assisted by monitoring evoked potentials. Identification of the posterior raphe to perform the myelotomy was carried out using the middle point of the virtual line that extends between the areas of input of the right and left dorsal roots in addition to the visualization of the incoming vessels to the posterior raphe. Once the lesion had been exposed, a frozen biopsy was performed, which was later complemented by routine techniques of histopathology, immunohistochemistry, and/or molecular biology.
In the postoperative period, patients received prophylaxis for deep venous thrombosis (DVT) through pneumatic compression on the lower limbs, elastic stockings, and/or low molecular weight heparin. Early physical therapy was also prescribed.
RESULTS
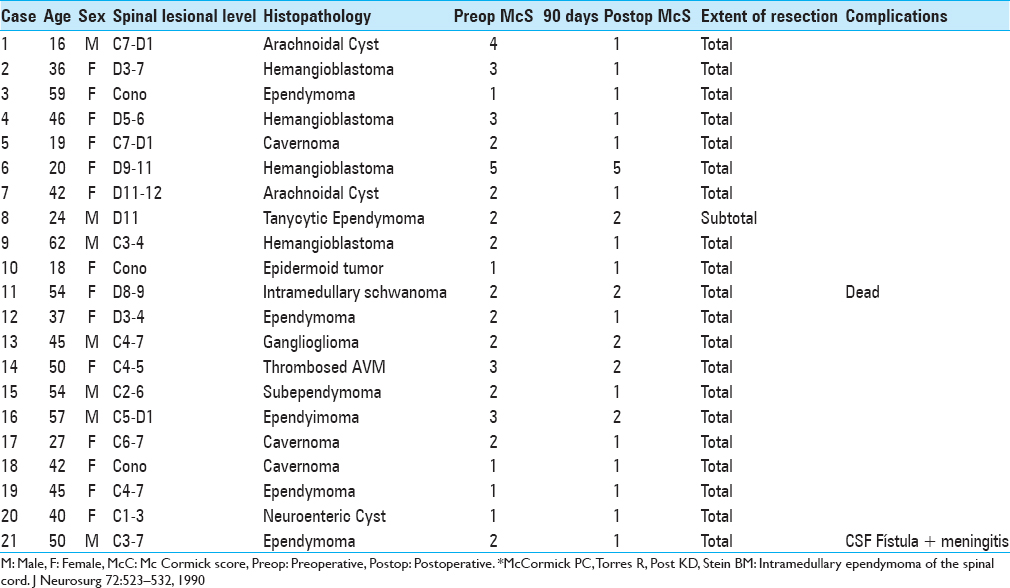
Patients’ median age was 39.8 years (range: 16–62). The locations of the lesions were: Cervical: 11; dorsal: 6; and conus: 4 cases. In the preoperative period, 5 patients had mMs = 1; 10 cases mMs = 2; 4 cases mMs = 3; 1 case mMs = 4; and 1 case mMs = 5. In summary, 19 cases had mMs >3 and 2 cases mMs <4.
Total resection was performed in 20 cases (95.2%) [
The intraoperative frozen biopsy permitted the differentiation of infiltrative lesions from noninfiltrative ones in all cases. Later on, pathological analysis confirmed 5 ependymomas, 1 tanycytic ependymoma, 4 hemanglioblastomas, 1 ganglioglioma, 1 subependymoma, 1 intramedullary schwannoma, 1 epidermoid tumor, 3 arachnoid cysts, and 4 vascular malformations.
Preoperatively, 8 cases had secondary syringomyelia that was resolved in all of the cases through surgical excision of the masses without additional treatment.
There were two complications. One patient presented cerebrospinal fluid (CSF) fistula with meningitis, which was conservatively resolved with antibiotic therapy, acetazolamide, and CSF external lumbar drainage for 5 days. Another patient, who was discharged, died from pulmonary thromboembolism on the postoperative 20th day. The assessment of the functional status within the postoperative 90 days showed a stable functional condition in 9 cases (42.8%) and a better condition in 12 cases (57.1%). A temporary decline was observed in 2 cases with recovery before 90 days had passed [
Only 1 patient received postoperative radiotherapy and chemotherapy according to the characteristics of the histopathology; a ganglioglioma with areas of malignancy in the glial sector.
DISCUSSION
The reported predictors of good outcome of the primary ISCTs are the preoperative functional status, histology of the tumor, and extent of the surgical resection.[
In regards to the results of the functional status reported in the literature, the improvement could be expected in 30–40% of the cases, stability in 50–60%, and decline in 5–10%.[
With regards to the surgical complications that are reported in the literature, these complications vary between 3.8 and 17%, and in most cases are CSF fistulas sometimes complicated with meningitis.[
Although the present study does not allow to reach statistical conclusions, we can conclude that every effort should be made to identify the Klekamp's Type A ISCTs during preoperative planning, and confirmed later on during surgery by frozen biopsies because these data determine the resectability of the lesion, encouraging us to perform radical surgeries with a low risk of functional declination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Dr. Dr Gustavo Sevlever and Dr. Silvia Christiansen for the revision of pathological samples, and Dr. Patricia Maggiora for her valuable assistance.
References
1. Bansal S, Ailawadhi P, Suri A, Kale SS, Sarat Chandra P, Singh M. Ten years’ experience in the management of spinal intramedullary tumors in a single institution. J Clin Neurosci. 2013. 20: 292-8
2. Brotchi J. Intrinsic spinal cord tumor resection. Neurosurgery. 2002. 50: 1059-63
3. Chamberlain MC, Tredway TL. Adult primary intradural spinal cord tumors: A review. Curr Neurol Neurosci Rep. 2011. 11: 320-8
4. Constantini S, Miller DC, Allen JC, Rorke LB, Freed D, Epstein FJ. Radical excision of intramedullary spinal cord tumors: Surgical morbidity and long-term follow-up evaluation in 164 children and young adults. J Neurosurg. 2000. 93: 183-93
5. Epstein FJ, Farmer JP, Freed D. Adult intramedullary spinal cord ependymomas: The results of surgery in 38 patients. J Neurosurg. 1993. 79: 204-9
6. Gelabert-Gonzalez M. Primary spinal cord tumours. An analysis of a series of 168 patients. Rev Neurol. 2007. 44: 269-74
7. Jallo GI, Danish S, Velazquez L, Epstein F. Intramedullary low-grade astrocytomas: Long-term outcome following radical surgery. J Neurooncol. 2001. 53: 61-6
8. Karikari IO, Nimjee SM, Hodges TR, Cutrell E, Hughes BD, Powers CJ. Impact of tumor histology on resectability and neurological outcome in primary intramedullary spinal cord tumors: A single-center experience with 102 patients. Neurosurgery. 2011. 68: 188-97
9. Klekamp J. Treatment of intramedullary tumors: Analysis of surgical morbidity and long-term results. J Neurosurg Spine. 2013. 19: 12-26
10. McGirt MJ, Chaichana KL, Atiba A, Attenello F, Yao KC, Jallo GI. Resection of intramedullary spinal cord tumors in children: Assessment of long-term motor and sensory deficits. J Neurosurg Pediatrics. 2008. 1: 63-7
11. Nakamura M, Ishii K, Watanabe K, Tsuji T, Takaishi H, Matsumoto M. Surgical treatment of intramedullary spinal cord tumors: Prognosis and complications. Spinal Cord. 2008. 46: 282-6
12. Sandalcioglu IE, Gasser T, Asgari S, Lazorisak A, Engelhorn T, Egelhof T. Functional outcome after surgical treatment of intramedullary spinal cord tumors: Experience with 78 patients. Spinal Cord. 2005. 43: 34-41
13. Schellinger KA, Propp JM, Villano JL, Mc Carthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol. 2008. 87: 173-9
14. Shrivastava RK, Epstein FJ, Perin NI, Post KD, Jallo GI. Intramedullary spinal cord tumors in patients older than 50 years of age: Management and outcome analysis. J Neurosurg Spine. 2005. 2: 249-55
15. White JB, Miller Gh, Layton KF, Krauss WE. Nonenhancing tumors of the spinal cord. J Neurosurg Spine. 2007. 7: 403-7
16. Woodwoth GF, Chaichana KL, McGirt MJ, Sciubba DM, Jallo GI, Gokaslan Z. Predictors of ambulatory function after surgical resection of intramedullary spinal cord tumors. Neurosurgery. 2007. 61: 99-106