- Department of Neurosurgery, Kuki General Hospital, 418-1 Kamihayami Kuki, Japan
- Department of Neurosurgery, National Defense Medical College, Namiki 3-2, Tokorozawa, Saitama, Japan
Correspondence Address:
Hiroshi Kageyama
Department of Neurosurgery, Kuki General Hospital, 418-1 Kamihayami Kuki, Japan
DOI:10.4103/2152-7806.156633
Copyright: © 2015 Kageyama H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Kageyama H, Toyooka T, Osada H, Tsuzuki N. Infratentorial arteriovenous malformation associated with persistent primitive hypoglossal artery. Surg Neurol Int 07-May-2015;6:71
How to cite this URL: Kageyama H, Toyooka T, Osada H, Tsuzuki N. Infratentorial arteriovenous malformation associated with persistent primitive hypoglossal artery. Surg Neurol Int 07-May-2015;6:71. Available from: http://surgicalneurologyint.com/surgicalint_articles/infratentorial-arteriovenous-malformation-associated/
Abstract
Background:We report a case of infratentorial arteriovenous malformation (AVM) associated with persistent primitive hypoglossal artery (PPHA). To our knowledge, this is the second reported case of these combined anomalies in the English literature. We discuss the embryological relationship between these two congenital vascular anomalies.
Case Description:An 18-year-old girl, who suddenly developed severe headache and vomiting followed by loss of consciousness, was admitted to our hospital. A computed tomography scan showed intracerebellar hemorrhage with obstructive hydrocephalus. Digital subtraction angiography revealed an AVM in the left cerebellar hemisphere and an ipsilateral PPHA. After the intracranial pressure was stabilized, the AVM was surgically removed. AVMs develop during the 4th to 8th week of embryonic life. In contrast, carotid-basilar anastomoses (CBAs) including primitive hypoglossal arteries appear and close spontaneously by the 6th week of embryonic life. Thus, AVMs precede CBAs, and a large amount of blood flows into the adjoining AVM via ipsilateral CBAs. As a result, spontaneous closure of a CBA may be disturbed.
Conclusion:We speculate that coexistence of infratentorial AVMs and ipsilateral CBAs is not incidental but inevitable.
Keywords: Arteriovenous malformation, carotid-basilar anastomosis, posterior fossa, persistent primitive hypoglossal artery
INTRODUCTION
Arteriovenous malformations (AVMs) are congenital vascular anomalies that arise as a result of abnormal blood vessel development during the early embryonic period.[
Persistent carotid-basilar anastomosis (CBA) is also a congenital vascular anomaly. It includes persistent primitive trigeminal artery (PPTA), persistent primitive hypoglossal artery (PPHA), persistent primitive otic artery, and persistent primitive proatlantal artery (type 1 and type 2).[
To the best of our knowledge, the incidence of infratentorial AVM with CBA is 2-3 times higher than that of common infratentorial AVM.[
Case descriptions
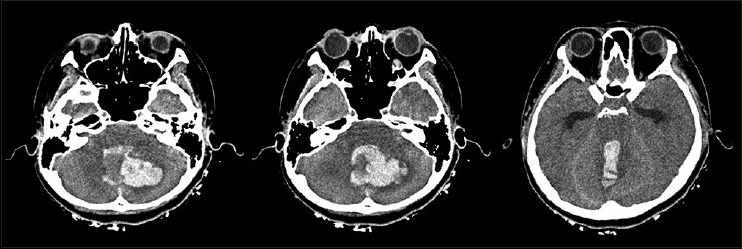
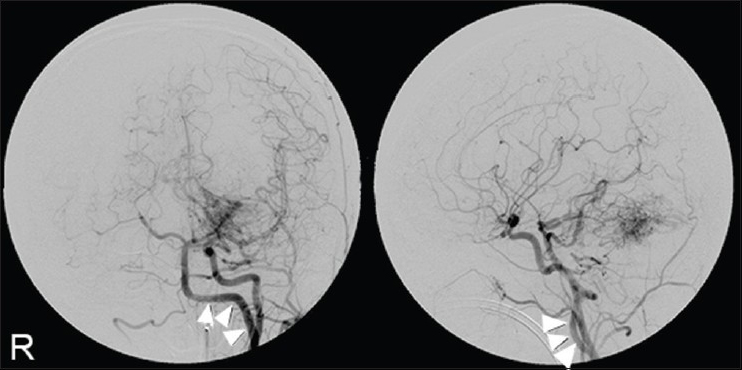
An 18-year-old girl presented with a ruptured infratentorial AVM. The patient's Glasgow Coma Scale score was 3 (E1V1M1). Plain computed tomography scans showed a large hematoma with obstructive hydrocephalus in the left cerebellar hemisphere [
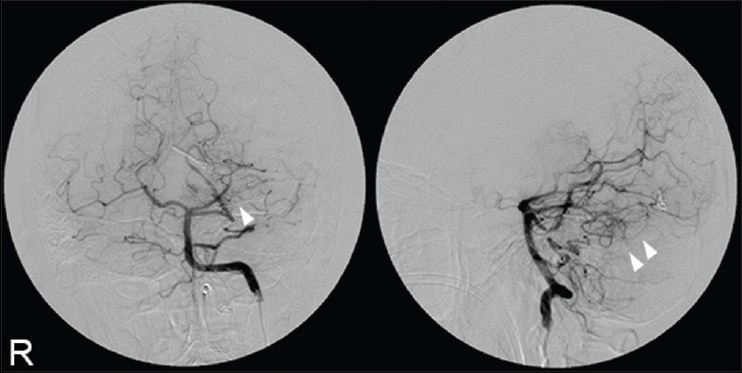
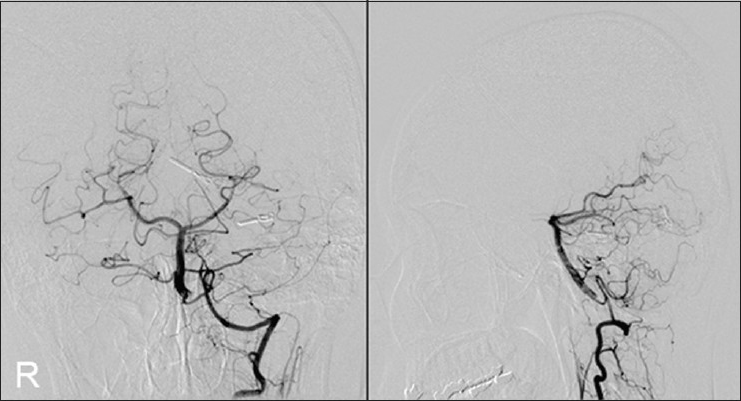
An angiogram of the left PPHA 2 weeks after the operation revealed residual nidus [
DISCUSSION
Intracranial AVMs and CBAs are congenital vascular anomalies. AVMs develop during the late somatic stages of the 4th week of embryonic life and almost no later than the 8th week.[
We hypothesized that the development of infratentorial AVMs disrupt the ability of CBAs to close.
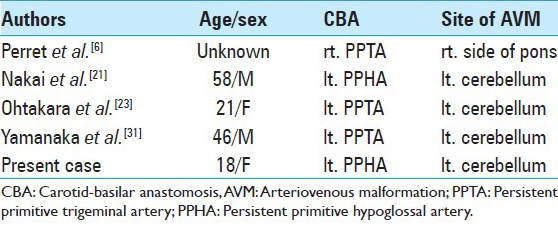
To our knowledge, 28 AVMs associated with CBA have been reported in the English literature;[
These findings strongly indicate a close relationship between infratentorial AVMs and persistent CBAs including PPHA. Embryologically, development of infratentorial AVM precedes the spontaneous closure of CBA. Once an AVM develops, a large amount of blood flows into the adjoining AVM via the ipsilateral vertebrobasilar system including the CBA, and this excess hemodynamic stress is a burden on the CBA. As a result, the spontaneous closure of the ipsilateral CBA may be disturbed. On the contrary, contralateral CBAs are never involved with the blood supply to the infratentorial AVM because bilateral CBAs are independent of each other until the longitudinal neural arteries merge to form the basilar artery at 31 days of embryonic life.[
CONCLUSION
Preexistence of an infratentorial AVM may induce formation of an ipsilateral persistent CBA; thus, coexistence of these two congenital anomalies is not incidental but inevitable.
References
1. Agnoli AL. Vascular anomalies and subarachnoid haemorrhage associated with persisting embryonic vessels. Acta Neurochir (Wien). 1982. 60: 183-99
2. Campbell RL, Dyken ML. Four cases of carotid-basilar anastomosis associated with central nervous system dysfunction. J Neurol Neurosurg Psychiatry. 1961. 24: 250-3
3. Fields WS. The significance of persistent trigeminal artery. Carotid-Basilar anastomosis. Radiology. 1968. 91: 1095-101
4. Gannon WE. Malformation of the brain. Persistent trigeminal artery and arteriovenous malformation. Arch Neurol. 1962. 6: 496-8
5. Garza-Mercado R, Cavazos E, Urrutia G. Persistent hypoglossal artery in combination with multifocal arteriovenous malformations of the brain: Case report. Neurosurgery. 1990. 26: 871-6
6. Harada K, Uozumi T, Kurisu K, Sumida M, Nakahara A, Migita K. Evaluation of cerebro-vascular diseases with persistent carotid-basilar anastomosis. No Shinkei Geka. 1994. 22: 1153-8
7. HD G.editors. Intracranial arteriovenous malformatons. New York: McGraw-Hill; 1996. p.
8. Hernesniemi JA, Dashti R, Juvela S, Vaart K, Niemela M, Laakso A. Natural history of brain arteriovenous malformations: A long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery. 2008. 63: 823-9
9. Jayaraman A, Garofalo M, Brinker RA, Chusid JG. Cerebral arteriovenous malformation and the primitive trigeminal artery. Arch Neurol. 1977. 34: 96-8
10. Karasawa JK, Furuse S, Kawai S, Uchida Y, Sakaki T. Studies on 2 cases of a persistent primitive hypoglossal artery. Case reports on a 9-year-old male patient with arteriovenous malformation and a 55-year-old male patient with brain stem syndrome. No To Shinkei. 1973. 24: 91-8
11. Karasawa J, Terano M, Nishikawa M, Kyoi K, Kikuchi H. Case of persistent bilateral carotid-basilar anastomoses (primitive otic artery and primitive trigeminal artery) with multiple vascular anomalies. No To Shinkei. 1972. 24: 91-8
12. Lamb J, Morris L. The carotid-basilar artery. A report and discussion of five cases. Clin Radiol. 1961. 12: 179-86
13. Luh GY, Dean BL, Tomsick TA, Wallace RC. The persistent fetal carotid-vertebrobasilar anastomoses. AJR Am J Roentgenol. 1999. 172: 1427-32
14. GÜNER MS. Arteriovenous malformation and persistent trigeminal artery association. Case report Turk Neurosurg. 1996. 6: 33-6
15. Moody RA, Poppen JL. Arteriovenous malformations. J Neurosurg. 1970. 32: 503-11
16. Mori HA, Maruyama K, Shin M, Tago M, Matsumoto T, Yoshikawa T. Parietal arteriovenous malformation associated with ipsilateral persistent primitive hypoglossal artery. Riv Neuroradiol. 2002. 15: 769-72
17. Mullan S, Mojtahedi S, Johnson DL, Macdonald RL. Embryological basis of some aspects of cerebral vascular fistulas and malformations. J Neurosurg. 1996. 85: 1-8
18. Nakai Y, Yasuda S, Hyodo A, Yanaka K, Nose T. Infratentorial arteriovenous malformation associated with persistent primitive trigeminal artery--case report. Neurol Med Chir (Tokyo). 2000. 40: 572-4
19. Nakajima K, Ito Z, Hen R, Uemura K, Matsuoka S. Congenital anomalies of cerebral artery and intracranial aneurysm. No To Shinkei. 1976. 28: 197-201
20. Nishida C, Ashikaga R, Araki Y, Nakamatsu K, Ono Y, Fujii K. Persistent hypoglossal artery associated with arteriovenous malformation: A case report. Eur J Radiol. 2000. 33: 59-62
21. Ohtakara K, Kuga Y, Murao K, Kojima T, Taki W, Waga S. Posterior fossa arteriovenous malformation associated with persistent primitive trigeminal artery--case report. Neurol Med Chir (Tokyo). 2000. 40: 169-72
22. Oran I, Parildar M, Memis A, Yunten N. Catheter and MR angiography of persistent trigeminal artery associated with occipital arteriovenous malformation. Comput Med Imaging Graph. 2000. 24: 33-5
23. Pasco A, Papon X, Bracard S, Tanguy JY, Ter Minassian A, Mercier P. Persistent carotid-vertebrobasilar anastomoses: How and why differentiating them?. J Neuroradiol. 2004. 31: 391-6
24. Perret G, Nishioka H. Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section VI. Arteriovenous malformations. An analysis of 545 cases of cranio-cerebral arteriovenous malformations and fistulae reported to the cooperative study. J Neurosurg. 1966. 25: 467-90
25. Purkayastha S, Jayadevan ER, Gupta AK, Bodhey NK. Cerebral Arteriovenous Malformation Embolized through Persistent Primitive Hypoglossal Artery. A Case Report. Interv Neuroradiol. 2005. 11: 392-
26. Sahoo YM, Mallikarjunaiah GS, David BS, Parida S. Persistent hypoglossal artery. Indian J Radiol. 1988. 42: 144-6
27. Shibata Y, Hyodo A, Saito A, Yoshii Y, Nose T. Large arteriovenous malformation associated with persistent primitive hypoglossal artery - case report. Neurol Med Chir (Tokyo). 1991. 31: 804-8
28. Tomsick TA, Lukin RR, Chambers AA. Persistent trigeminal artery: Unusual associated abnormalities. Neuroradiology. 1979. 17: 253-7
29. Uchino A, Matsunaga M, Ohno M. Arteriovenous malformation of the corpus callosum associated with persistent primitive trigeminal artery-case report. Neurol Med Chir (Tokyo). 1989. 29: 429-32
30. Wakai S, Ueda Y, Nagai M. Cerebrovascular anomalies associated with primitive trigeminal artery-report of three cases. Neurol Med Chir (Tokyo). 1987. 27: 633-6
31. Yamanaka K, Noguchi K, Hayasaki K, Matsuoka Y. Persistent primitive hypoglossal artery associated with arteriovenous malformation-case report. Neurol Med Chir (Tokyo). 1990. 30: 949-55
32. Yamauchi Y, Aoyama T, Sugitani Y, Koama M, Nukada T. Persistent hypoglossal artery associated with arteriovenous malformation-a study on cerebral circulation. Rinsho Shinkeigaku. 1974. 14: 539-47