- Department of Neurosurgery, NIMHANS, Bengaluru, Karnataka, India
- Department of Neuropathology, NIMHANS, Bengaluru, Karnataka, India
Correspondence Address:
A. Arivazhagan
Department of Neurosurgery, NIMHANS, Bengaluru, Karnataka, India
DOI:10.4103/2152-7806.198731
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: S. J. Balaparameswara Rao, Amey R. Savardekar, B. N. Nandeesh, A. Arivazhagan. Management dilemmas in a rare case of pituitary apoplexy in the setting of dengue hemorrhagic fever. 19-Jan-2017;8:4
How to cite this URL: S. J. Balaparameswara Rao, Amey R. Savardekar, B. N. Nandeesh, A. Arivazhagan. Management dilemmas in a rare case of pituitary apoplexy in the setting of dengue hemorrhagic fever. 19-Jan-2017;8:4. Available from: http://surgicalneurologyint.com/surgicalint_articles/management-dilemmas-in-a-rare-case-of-pituitary-apoplexy-in-the-setting-of-dengue-hemorrhagic-fever/
Abstract
Background:Pituitary apoplexy occurs due to infarction or hemorrhage, within a pituitary adenoma or a nontumorous pituitary gland and can have catastrophic consequences. Dengue hemorrhagic fever (DHF) is a severe manifestation of the spectrum of dengue virus infection and is characterized by high-grade fever, thrombocytopenia, hemorrhagic tendencies, and increased vascular permeability. Cases of incidentalomas complicated by DHF and presenting with apoplexy are extremely rare.
Case Description:We describe the case of a 45-year-old gentleman who suffered an attack of pituitary apoplexy while being treated for DHF. The issues pertaining to the management of hydrocephalus, timing of surgical intervention, and treatment of electrolyte imbalances encountered in the dual setting of DHF and pituitary apoplexy are discussed with reference to the outcome in our case.
Conclusion:Although patients suffering from DHF harbor multiple factors, which may be precipitants of pituitary apoplexy, the association between these two conditions is rare and only few case reports document their coexistence. We review the pertinent literature and discuss the management dilemmas faced by us while dealing with these dual pathological states.
Keywords: Dengue hemorrhagic fever, hydrocephalus, pituitary apoplexy, surgical management, thrombocytopenia
INTRODUCTION
Pituitary apoplexy (PA) is an acute clinical syndrome characterized by sudden headache, vomiting, visual disturbances, ophthalmoplegia, and/or altered consciousness, secondary to infarction or hemorrhage within a pituitary tumor or nontumorous pituitary gland.[
CASE REPORT
Clinical presentation
A 45-year-old man presented with a history of high-grade fever of 7-day duration. He was evaluated at a general hospital, and was noted to have NS1 IgM positive serology for Dengue infection and low platelet counts. Patient was diagnosed as DHF in view of severe thrombocytopenia and was managed accordingly with resuscitative measures. On the 7th day of the fever, the patient developed severe headache, multiple episodes of vomiting, and altered sensorium. Electrocardiograph (ECG) showed sinus bradycardia and computed tomography (CT) scan of the brain showed sellar and suprasellar hemorrhagic lesion with obstruction of the foramen of Monro, leading to hydrocephalus [
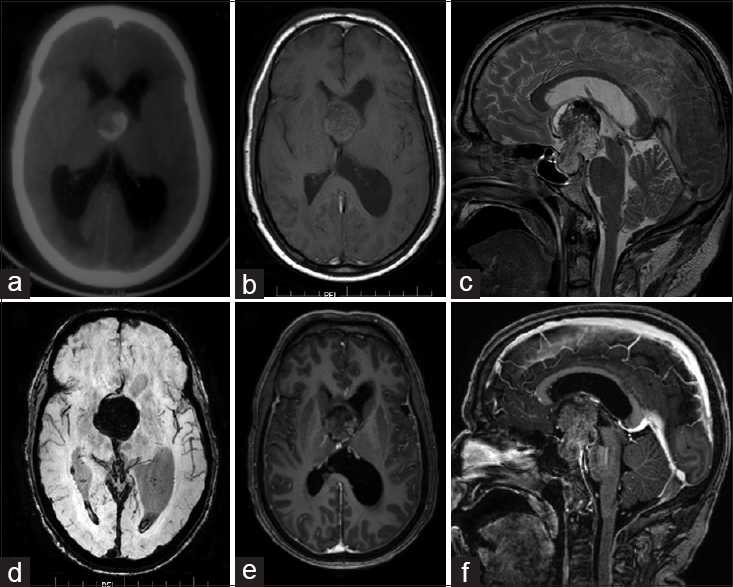
Figure 1
(a) Computed tomography (plain) of the brain at presentation showing the hemorrhagic lesion in the third ventricle obstructing the foramen of Monro and causing hydrocephalus; magnetic resonance imaging demonstrating [(b) T1-weighted axial, (c) T2-weighted sagittal, (d) Susceptibility-weighted Imaging (SWI) axial, (e) contrast-enhanced T1-weighted axial, and (f) contrast-enhanced T2-weighted sagittal images] a pituitary macroadenoma with suprasellar extension with evidence of apoplectic change
Course in the hospital and surgical management
The management issues in this patient were treatment of hydrocephalus and the surgical management of PA in the setting of severe thrombocytopenia. The patient's platelet count at admission was 27000/mm3. Serial platelet transfusions were instituted. While his hematological dysfunction was being corrected, patient deteriorated in sensorium (E1M4V2), was immediately intubated, and a right frontal external ventricular drain (EVD) was placed. Cerebrospinal fluid (CSF) was under high pressure. Patient did not improve in sensorium following EVD and repeat CT brain showed persistent left lateral ventriculomegaly. A left frontal EVD was placed. Following bilateral EVD placement, patient improved in sensorium to drowsy, obeying, and disoriented status.
A magnetic resonance imaging (MRI) of the brain showed a sellar suprasellar lesion extending into the third ventricle up to the foramen of Monro. The lesion was T1 isointense, T2 hyperintense with areas of T2 hypointensity, and was heterogeneously enhancing on contrast [Figure
Histopathology
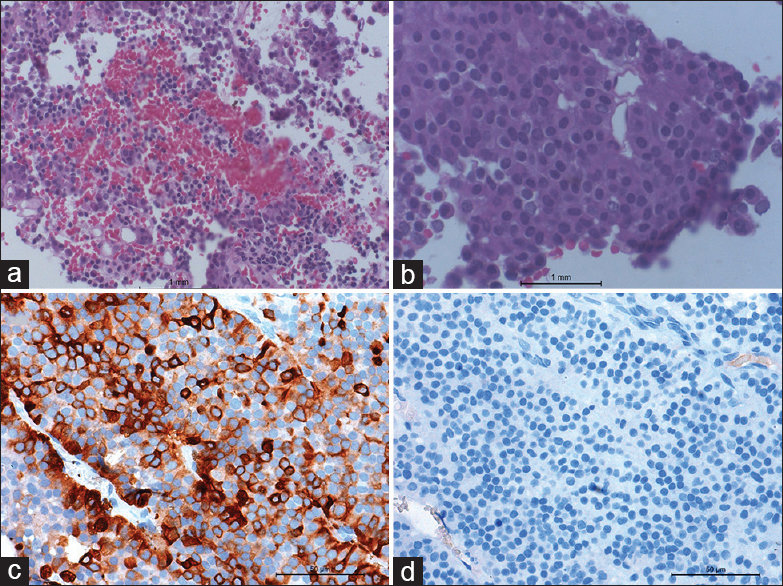
Histopathology sections showed fragments of an endocrine neoplasm composed of sheets, lobules, and papillaroid clusters of round-to-polyhedral cells having moderate amphophilic cytoplasm and a regular round-to-oval nucleus [Figure
Figure 2
(a) Microphotograph showing fragmented bits of a cellular neoplasm with hemorrhage (hematoxylin and eosin ×100). (b) Microphotograph showing an endocrine neoplasm with cells arranged in organoid nests and conglomerate acinar, solid clusters (hematoxylin and eosin ×400). Note the uniform cells and regular nuclei with homogenous chromatin; (c) Microphotograph showing cells positively stained for ACTH immuno-stain (ACTH-IHC ×400) (d) Microphotograph showing cells negatively stained for growth hormone immunostain (GH-IHC ×400)
Postoperative course and follow-up
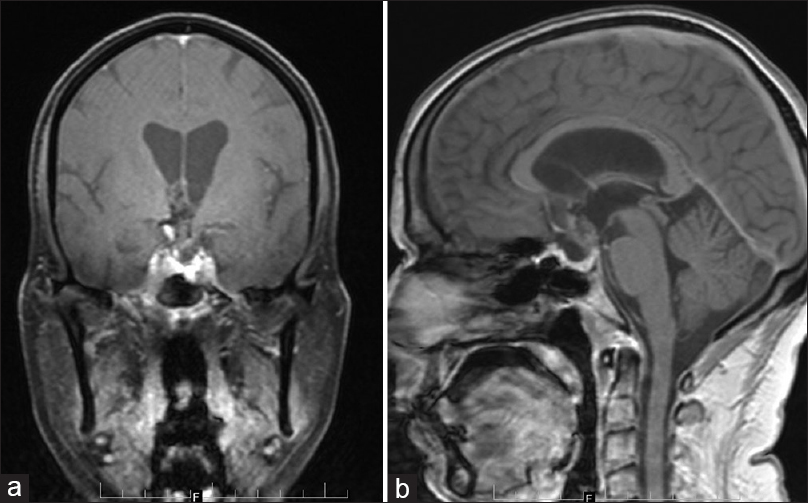
The patient had a stormy postoperative course. He developed diabetes insipidus with serially rising sodium levels and high urine output. The intravascular volume status was monitored with central venous pressure (CVP) recordings. Patient was managed with hypotonic fluids and subcutaneous pitressin (5 units BD and 5 units in excess if urine output for two consecutive hours was more than 250 ml). The patient was managed with strict hourly input-output monitoring and eighth hourly electrolyte levels. This intensive CVP, input-output, and electrolyte level monitoring was essential in the setting of hypothalamic–hypophyseal dysfunction (in view of pituitary apoplexy) and increased vascular permeability (in view of DHF). On postoperative day 4, the patient regained consciousness. Sequential EVDs were removed with serial CTs not showing evidence of ventriculomegaly after EVD blockade. On discharge, the patient was conscious with visual acuity of 6/36 in both eyes, and fundus examination showing bilateral temporal pallor. At 6-month follow-up, the patient is doing well with only residual bitemporal hemianopia and MRI brain revealed minimal residual lesion [Figure
DISCUSSION
PA (hemorrhage or infarction of a pituitary adenoma or nontumorous pituitary gland) may occur spontaneously or as a result of several precipitating factors such as head trauma, dynamic tests to evaluate pituitary function, surgery (mainly cardiac surgery), coagulation disorders, medications including aspirin, estrogens, heparin, and dopamine agonists, and some conditions such as chronic systemic hypertension, diabetes mellitus, and radiotherapy.[
Thrombocytopenia can be caused by various conditions, infections being one among them. Dengue fever is endemic in tropical countries and can range from a nonspecific febrile illness to DHF, which is characterized by high-grade fever, marked thrombocytopenia (<100,000/μL), and increased vascular permeability.[
In our case, the first challenge was the management of hydrocephalus. Initially, as the patient was maintaining a conscious status, it was decided to correct thrombocytopenia, perform imaging and hormonal evaluation, and then plan transsphenoidal decompression of the tumor. When the patient deteriorated in sensorium, raised ICP due to hydrocephalus or the apoplectic lesion compressing on the hypothalamus were considered to be the cause. A calculated risk of placement of EVD in the setting of severe thrombocytopenia had to be taken. While the EVD placement can resolve the hydrocephalus, it also could result in intraventricular/parenchymal hemorrhage adding to the complexity of the condition.
The second dilemma was timing of the the definitive surgery. After ICP control and stabilizing the hemodynamic parameters and the serum electrolytes, the patient improved in sensorium to a drowsy conscious state. The options of VP shunt followed by delayed surgery at a later date or decompression in the present admission were considered, weighing the risks/benefits of both the options. Management of PA in the setting of thrombocytopenia can be very challenging because the benefit of early intervention has to be carefully weighed against the risk of bleeding during and immediately after surgery.[
The patient had a stormy postoperative course, and management of his fluid and electrolyte disturbances was the third demanding task. The impact of the pituitary stalk and hypothalamic dysfunction was compounded by the increased vascular permeability seen in DHF. In addition, hyponatremia (serum sodium level <130 mEq/L) is commonly found in dengue patients and has been hypothesized to be a consequence of salt depletion, excess water from increased metabolism, decreased renal excretion, transient inappropriate antidiuretic hormone, or the influx of sodium into the cells as a result of dysfunction of sodium potassium pump seen in the setting of dengue fever.[
CONCLUSION
An occurrence of pituitary apoplexy in the background of DHF raises multiple complexities in the management. An awareness of the detailed pathophysiology of both the conditions and their interplay at hemodynamic and endocrine levels is essential for the treating physician to actively manage the problem. The management of raised ICP secondary to hydrocephalus, importance of the correct timing of surgical intervention and active intervention to maintain fluid, and electrolyte balance are paramount to achieving a good outcome in the combined setting of pituitary apoplexy and DHF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arafah BM, Taylor HC, Salazar R, Saadi H, Selman WR. Apoplexy of a pituitary adenoma after dynamic testing with gonadotropin-releasing hormone. Am J Med. 1989. 87: 103-5
2. Biousse V, Newman NJ, Oyesiku NM. Precipitating factors in pituitary apoplexy. J Neurol Neurosurg Psychiatry. 2001. 71: 542-5
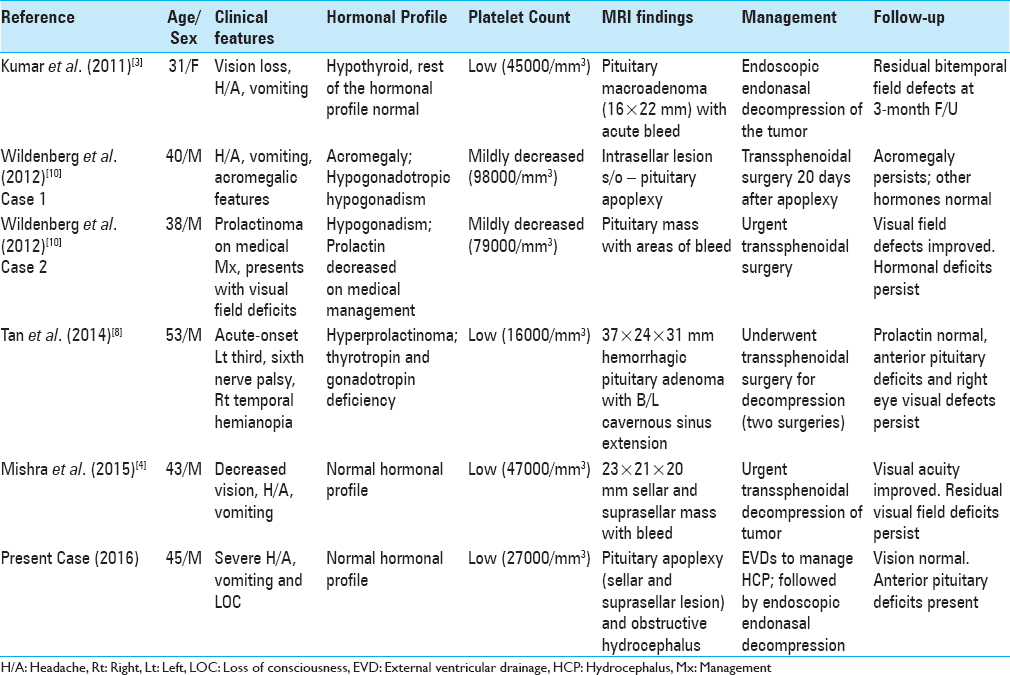
3. Kumar V, Kataria R, Mehta VS. Dengue hemorrhagic fever: A rare cause of pituitary tumor hemorrhage and reversible vision loss. Indian J Ophthalmol. 2011. 59: 311-2
4. Mishra SS, Panigrahi S, Das S. Dengue hemorrhagic fever: A rare case of pituitary apoplexy. Neurol India. 2014. 62: 92-3
5. Möller-Goede DL, Brändle M, Landau K, Bernays RL, Schmid C. Pituitary apoplexy: Re-evaluation of risk factors for bleeding into pituitary adenomas and impact on outcome. Eur J Endocrinol. 2011. 164: 37-43
6. Semple PL, Webb MK, de Villiers JC, Laws ER. Pituitary apoplexy. Neurosurgery. 2005. 56: 65-72
7. Simmons CP, Farrar JJ, Nguyen vV, Wills B. Dengue. N Engl J Med. 2012. 366: 1423-32
8. Tan SK, Seow CJ, Tan E, Chau YP, Dalan R. Pituitary apoplexy secondary to thrombocytopenia due to dengue hemorrhagic Fever: A case report and review of the literature. Endocr Pract. 2014. 20: 58-64
9. Varavithya W, Manu P, Kittikool J, Phongbetchara P, Kashemsant C. Studies on dengue hemorrhagic fever. II. Electrolyte study. J Med Assoc Thai. 1973. 56: 15-23
10. Wildemberg LE, Neto LV, Niemeyer P, Gasparetto EL, Chimelli L, Gadelha MR. Association of dengue hemorrhagic fever with multiple risk factors for pituitary apoplexy. Endocr Pract. 2012. 18: 97-101