- Department of Neurosurgery, Campo Limpo Municipal Hospital, São Paulo, Brasil
- Department of Neurosurgery, Caja Petrolera de Salud Hospital, Santa Cruz de la Sierra, Bolivia
- School of Medicine, University City of São Paulo, São Paulo, Brasil
- Department of Neurosurgery, School of Medicine, Franz Tamayo University, Santa Cruz de la Sierra, Bolivia
Correspondence Address:
Carlos B. Dabdoub
Department of Neurosurgery, School of Medicine, Franz Tamayo University, Santa Cruz de la Sierra, Bolivia
DOI:10.4103/2152-7806.166195
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dabdoub CB, Salas G, N. Silveira Ed, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int 29-Sep-2015;6:155
How to cite this URL: Dabdoub CB, Salas G, N. Silveira Ed, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int 29-Sep-2015;6:155. Available from: http://surgicalneurologyint.com/surgicalint_articles/review-of-the-management-of-pneumocephalus/
Abstract
Background:Pneumocephalus (PNC) is the presence of air in the intracranial cavity. The most frequent cause is trauma, but there are many other etiological factors, such as surgical procedures. PNC with compression of frontal lobes and the widening of the interhemispheric space between the tips of the frontal lobes is a characteristic radiological finding of the “Mount Fuji sign.” In addition to presenting our own case, we reviewed the most relevant clinical features, diagnostic methods, and conservative management for this condition.
Case Description:A 74-year-old male was diagnosed with meningioma of olfactory groove several years ago. After no improvement, surgery of the left frontal craniotomy keyhole type was conducted. A computed tomography (CT) scan of the skull performed 24 h later showed a neuroimaging that it is described as the silhouette of Mount Fuji. The treatment was conservative and used continuous oxygen for 5 days. Control CT scan demonstrated reduction of the intracranial air with normal brain parenchyma.
Conclusion:The review of the literature, we did not find any cases of tension pneumocephalus documented previously through a supraorbital keyhole approach. There are a few cases reported of patients with Mount Fuji signs that do not require surgical procedures. The conservative treatment in our report leads to clinical and radiological improvement as well as a reduction in hospitalization time.
Keywords: Mount Fuji sign, olfactory meningioma, pneumocephalus, supraorbital keyhole approach, tension pneumocephalus
INTRODUCTION
The terms pneumocephalus (PNC) and tension pneumocephalus (TP) were created by Wolff[
CASE REPORT
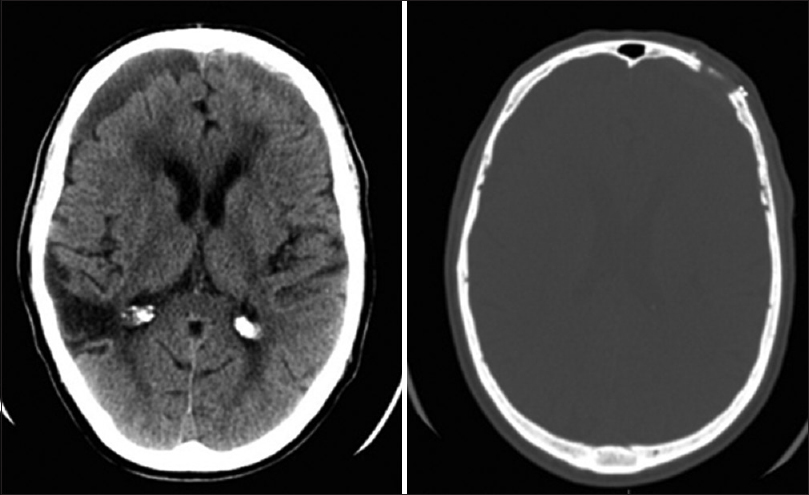
A 74-year-old right-handed male was diagnosed with meningioma of olfactory groove several years ago. He presented with psychomotor agitation, confusion, and vertiginous crises. Among its antecedents, surgery for maxillary sinusitis, heart, and mesenteric thrombosis were mentioned. It more recently referred to a mild head injury. On neurological examination, motor or sensory deficits were not evidenced. The cranial nerve examination was normal. The patient underwent magnetic resonance imaging (MRI) that showed olfactory groove meningioma and significant perilesional edema around the tumor. He was initially treated with dexamethasone at a dosage of 4 mg every 6 h. After no improvement, surgery of the left frontal craniotomy keyhole type was conducted. The rigid endoscope was used to complete the resection. A computed tomography (CT) scan of the skull performed 24 h later showed bi-frontal subdural PNC with Mount Fuji sign with a slight shift to the right ventricular system and no frontal sinus breaches was identified [
The family called for the transfer of the patient to a neighboring country, a request that was rejected because of the risk that implied. It was decided to observe the evolution of the patient with the use of antibiotics, acetazolamide, analgesics, and continuous oxygen at 5 L/min for 5 days. On 5th postoperative day, his level of consciousness improved. Control CT scan demonstrated reduction of the intracranial air with normal surface contours and parenchyma [
DISCUSSION
Pneumocephalus
The accumulation of intracranial air can be acute (<72 h) or delayed (≥72 h).[
At least two possible mechanisms for the development of PNC are described.[
A review of 295 patients with PNC indicates that trauma is the most common cause of PNC, accounting for 75% of cases. Infection, most common chronic otitis media, accounted for 9% of the cases reviewed.[
Clinically, PNC can cause headaches, nausea, vomiting, irritability, dizziness, and seizures. Sometimes the patient reported air entry intracranial space as a “gurgling” sensation in the head, based on the audible gas input.[
Mount Fuji sign
CT is a golden standard for PNC or TP diagnostics. It only requires 0.55 mL of air to be detected, whereas a simple skull radiograph requires at least 2 mL.[
An MRI axial view of fluid-attenuated inversion recovery revealed the Mount Fuji sign with collapsed frontal lobes and widening of the interhemispheric space between the bilateral tips of the frontal lobes.[
The Mount Fuji sign indicates more severe PNC than the peaking sign and the necessity of emergent decompression,[
Treatment of pneumocephalus
Pneumocephalus usually gets absorbed without any clinical manifestations. The conservative treatment involves placing the patient in the Fowler position of 30°, avoiding Valsalva maneuver (coughing and sneezing), administering pain and antipyretic medications to prevent hyperthermia, and osmotic diuretics. With these measures, reabsorption was observed in 85% of cases after 2–3 weeks.[
When clinical signs appear, such as intracranial hypertension or impaired consciousness that endangers the life of the patient, treatment consists of emergent decompression to alleviate pressure on the brain parenchyma. Also, air is toxic to neurons, causing further damage to the already compromised parenchyma, and that leads to cerebral edema surrounding the air that evolves into encephalomalacia.[
Treatment options for TP include the drilling of burr holes, needle aspiration, and closure of the dural defect. If the frontal sinus is open during surgery, it is aggressively managed with exenteration of the mucosa, sinus packing with abdominal fat or a piece of temporal muscle and covered with frontal fascia.[
Pneumocephalus and air evacuation
Traveling by plane is considered high risk because as the height increases, atmospheric pressure decreases, and the gasses expand. Therefore, a pneumothorax could become hypertensive, a bulla could expand or break, and PNC could enlarge and produce more intracranial hypertension. However, Donovan et al.[
Finally, the medical guideline recommends waiting at least 7 days to fly after a transcranial or spinal surgery that could introduce gas into the skull. Neurosurgical procedures could be a cause of residual intracranial air and could create a dormant fistulous tract that opens when the cabin pressure changes. Although it is difficult to make one guideline to apply to all cases, the concern for possible problems during air travel could lead to a consensus among consultant neurosurgeons.[
Supraorbital keyhole craniotomy
The supraorbital craniotomy offers equal surgical possibilities with fewer approach-related morbidity due to limited exposure of the cerebral surface and minimal brain retraction. The short skin incision within the eyebrow and careful soft tissue dissection result in a pleasing cosmetic outcome.[
According to Ormond and Hadjipanayis,[
The main complication reported with the superciliary craniotomy was CSF rhinorrhea. Several papers showed different ranges. In 66 patients operated on using the lateral supraorbital approach applied to olfactory meningiomas, Romani et al.[
CONCLUSIONS
The review of the literature, we did not find any cases of TP documented previously through a supraorbital keyhole approach.
TP must be treated by surgical revision when it causes intracranial hypertension and/or deterioration of consciousness. There are a few cases reported of patients with Mount Fuji signs that do not require surgical procedures. The conservative treatment in these patients with HBO2 therapy sessions in a monoplace hyperbaric chamber with 100% oxygen concentration or normobaric oxygenation administered continuously at 5 L/min at least for 5 days, may lead to clinical and radiological improvement as well as a reduction in hospitalization time.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agrawal A, Singh BR. Mount Fuji sign with concavo-convex appearance of epidural haematoma in a patient with tension pneumocephalus. Radiol Case. 2009. 3: 10-2
2. Aoki N, Sakai T. Computed tomography features immediately after replacement of haematoma with oxygen through percutaneous subdural tapping for the treatment of chronic subdural haematoma in adults. Acta Neurochir (Wien). 1993. 120: 44-6
3. Bernstein AL, Cassidy J, Duchynski R, Eisenberg SS. Atypical headache after prolonged treatment with nasal continuous positive airway pressure. Headache. 2005. 45: 609-11
4. Blanco-Ulla M, Villa Fernández J. Anatomical basis of the sign of Mount Fuji. Rev Argent Radiol. 2014. 78: 242-4
5. Czirják S, Szeifert GT. The role of the superciliary approach in the surgical management of intracranial neoplasms. Neurol Res. 2006. 28: 131-7
6. Dandy WE. Pneumocepahlus (intracranial pneumatocele or aerocele). Arch Surg. 1926. 132: 949-82
7. Donovan DJ, Iskandar JI, Dunn CJ, King JA. Aeromedical evacuation of patients with pneumocephalus: Outcomes in 21 cases. Aviat Space Environ Med. 2008. 79: 30-5
8. Ectors L. Chronic subdural hematoma. Surgical treatment. (article in French). Acta Chir Belg. 1962. 6: 570-606
9. González Tortosa J, Mendoza Roca A, Poza Poza M. Post-traumatic pneumocephalus, aggravated by hyperbaric chamber treatment.(article in Spanish). Neurocirugía. 1996. 7: 126-8
10. Hokama A, Yara S, Fujita J, Nakamura S, Nakaema M, Kuniyoshi Y. The Mount Fuji sign of the pneumoperitoneum. Emerg Med J. 2009. 26: 300-
11. Huh J. Barotrauma-induced pneumocephalus experienced by a high risk patient after commercial air travel. J Korean Neurosurg Soc. 2013. 54: 142-4
12. Ishiwata Y, Fujitsu K, Sekino T, Fujino H, Kubokura T, Tsubone K. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. J Neurosurg. 1988. 68: 58-61
13. Karavelioglu E, Eser O, Haktanir A. Pneumocephalus and pneumorrhachis after spinal surgery: Case report and review of the literature. Neurol Med Chir (Tokyo). 2014. 54: 405-7
14. Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg. 2012. 77: 713-24
15. Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien). 1967. 16: 1-78
16. Michel SJ. The Mount Fuji sign. Radiology. 2004. 232: 449-50
17. Monajati A, Cotanch WW. Subdural tension pneumocephalus following surgery. J Comput Assist Tomogr. 1982. 6: 902-6
18. Ogando-Rivas E, Navarro-Ramírez PA, Benítez-Gasca PA, Lorenzo-Ruiz M, Ramos-Sandoval F. Asymptomatic massive neumoencephalus (article in Spanish). Rev Med Hosp Gen Méx. 2014. 77: 74-8
19. Ormond DR, Hadjipanayis CG. The supraorbital keyhole craniotomy through an eyebrow incision: Its origins and evolution. Minim Invasive Surg 2013. 2013. p.
20. Paiva WS, de Andrade AF, Figueiredo EG, Amorim RL, Prudente M, Teixeira MJ. Effects of hyperbaric oxygenation therapy on symptomatic pneumocephalus. Ther Clin Risk Manag. 2014. 10: 769-73
21. Paiva-Neto MA, Tella OI. Supra-orbital keyhole removal of anterior fossa and parasellar meningiomas. Arq Neuropsiquiatr. 2010. 68: 418-23
22. Pankaj G. Normobaric oxygen therapy strategies in the treatment of postcraniotomy pneumocephalus. J Neurosurg. 2008. 108: 926-9
23. Penrose-Stevens A, Ibrahim A, Redfern RM. Localized pneumocephalus caused by Clostridium perfringens meningitis. Br J Neurosurg. 1999. 13: 85-6
24. Prakash B, Pranesh MB, Parimalam N, Harish Kumar R. Hyperostosis frontalis interna mimicking Mount Fuji sign. J Assoc Physicians India. 2011. 59: 181-3
25. Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994. 80: 1008-12
26. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55
27. Romani R, Lehecka M, Gaal E, Toninelli S, Celik O, Niemelä M. Lateral supraorbital approach applied to olfactory groove meningiomas: Experience with 66 consecutive patients. Neurosurgery. 2009. 65: 39-52
28. Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, Carrillo-Yagüe R. Intraventricular tension pneumocephalus after transsphenoidal surgery: A case report and literature review. Neurocirugia (Astur). 2007. 18: 134-7
29. Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000. 84: 115-7
30. Solomiichuk VO, Lebed VO, Drizhdov KI. Posttraumatic delayed subdural tension pneumocephalus. Surg Neurol Int. 2013. 4: 37-
31. Tazón-Varela MA, Hernández-Herrero M, Alonso-Vega L, Pérez-Mier LA, Gallastegui Menéndez A. Severe head injury: The Mount Fuji sign.(article in Spanish). Emergencias. 2011. 23: 415-
32. Venkatesh SK, Bhargava V. Clinics in diagnostic imaging (119). Post-traumatic intracerebral pneumatocele. Singapore Med J. 2007. 48: 1055-9
33. Webber-Jones JE. Tension pneumocephalus. J Neurosci Nurs. 2005. 37: 272-6
34. Wolff E. Air accumulation in the right lateral ventricle of the brain (Pneumocephalus) (article in German). Münch Med Wochenschr. 1914. 61: 899-
35. Yamashita S, Tsuchimochi W, Yonekawa T, Kyoraku I, Shiomi K, Nakazato M. The Mount Fuji sign on MRI. Intern Med. 2009. 48: 1567-8