- Department of Neurosurgery, St. Louis University, St. Louis, Missouri, USA
Correspondence Address:
Jeroen Raymond Coppens
Department of Neurosurgery, St. Louis University, St. Louis, Missouri, USA
DOI:10.4103/2152-7806.173564
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marvin E, Laws LH, Coppens JR. Ruptured pseudoaneurysm of the middle meningeal artery presenting with a temporal lobe hematoma and a contralateral subdural hematoma. Surg Neurol Int 07-Jan-2016;7:
How to cite this URL: Marvin E, Laws LH, Coppens JR. Ruptured pseudoaneurysm of the middle meningeal artery presenting with a temporal lobe hematoma and a contralateral subdural hematoma. Surg Neurol Int 07-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/ruptured-pseudoaneurysm-of-the-middle-meningeal-artery-presenting-with-a-temporal-lobe-hematoma-and-a-contralateral-subdural-hematoma/
Abstract
Background:Traumatic pseudoaneurysms of the middle meningeal artery (MMA) are rare, associated with skull fractures, and have a high mortality rate. When they rupture, MMA pseudoaneurysms frequently cause epidural hematomas and occasionally ipsilateral subdural or subarachnoid hemorrhage. Isolated intraparenchymal hemorrhage has also been reported.
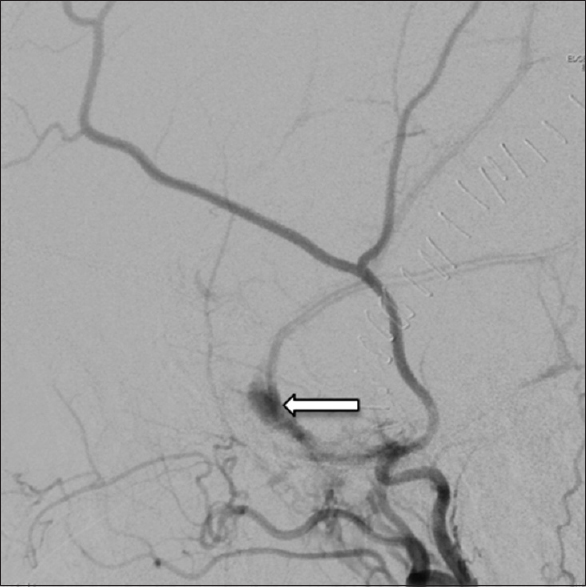
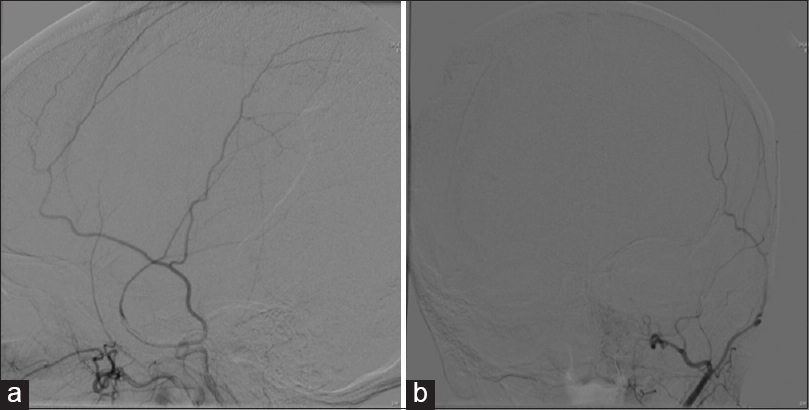
Case Description:A 54-year-old female who suffered a loss of consciousness resulting in a fall presented with a Glasgow Coma Scale of 7t. Imaging demonstrated a right subdural hematoma (SDH) with midline shift, left skull fracture overlying the left MMA, and left temporal lobe intraparenchymal hematoma extending to the surface. The patient underwent a right craniectomy with evacuation of the SDH, and the preoperative computed tomographic angiography revealed abnormal dilation of the left MMA consistent with a pseudoaneurysm. The pseudoaneurysm was treated with endovascular treatment, and the intraparenchymal hematoma was treated conservatively. Her recovery was uneventful, and she received a cranioplasty 3 months after the decompression.
Conclusions:The presence of a fracture over the MMA and intraparenchymal hematoma should prompt suspicion for a traumatic pseudoaneurysm. Pseudoaneurysms of the MMA can cause catastrophic bleeding, and prompt treatment is necessary. Endovascular embolization is an effective method that decreases the hemorrhage risk of MMA pseudoaneurysms.
Keywords: Intraparenchymal hemorrhage, subdural hematoma, traumatic pseudoaneurysm
INTRODUCTION
Traumatic pseudoaneurysms of the middle meningeal artery (MMA) are uncommon. They are often associated with skull fractures[
CASE REPORT
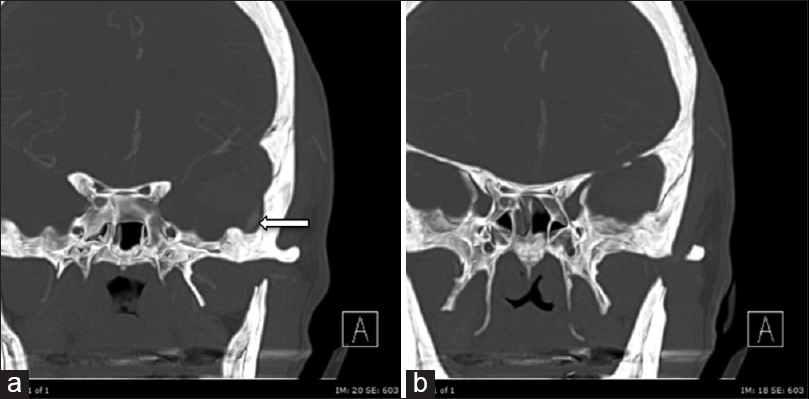
Fifty-four-year-old female transferred from an outside facility after a fall stairs secondary to an episode of loss of consciousness. She presented with a Glasgow Coma Scale of 7t. She was purposeful but not following commands or opening her eyes. Computed tomography (CT) demonstrated a right-sided 0.8 cm thick SDH, with 6 mm of the right-to-left shift, along with a left-sided temporal lobe IPH measuring 8 cm by 2 cm by 1.5 cm [
DISCUSSION
True aneurysms consist of a focal dilation of an artery that contains all normal layers of an arterial wall and an intact adventitia. In contrast, a pseudoaneurysm, also known as a false aneurysm, is usually the consequence of a vascular injury that results in disruption of all layers of the artery. The formation of a hematoma occurs on the outside of the arterial wall. Histologically, the wall of a pseudoaneurysm does not contain normal arterial wall structures, and the hematoma is usually contained by adventitia or surrounding perivascular soft tissue. Schulze first described traumatic MMA pseudoaneurysms in 1957,[
The most frequent presentation of an MMA pseudoaneurysm is an epidural hematoma, occurring in up to 70% of cases.[
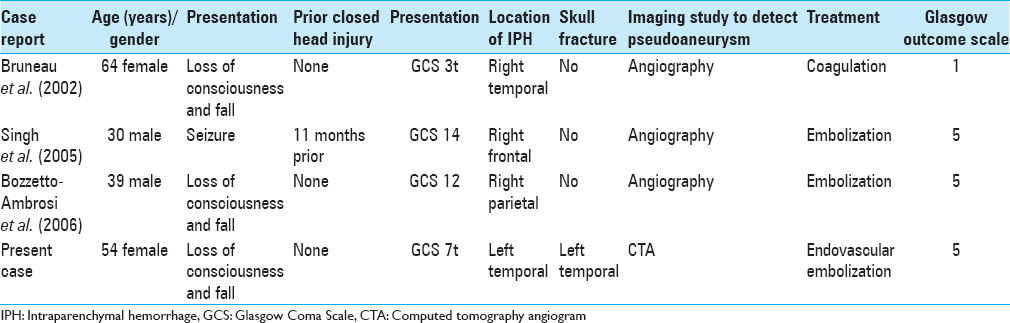
There have been several case reports describing delayed hemorrhages and neurological deterioration related to pseudoaneurysm rupture in patients that had recovered from their initial head injury.[
Delayed presentation seems more common in the cases of IPH.[
Radiographic identification of a pseudoaneurysm of the meningeal vessels may be difficult. There often needs to be a high index of suspicion to diagnose an MMA pseudoaneurysm. Epidural hematomas, for example, rarely require angiographic evaluation because hematomas that are associated with MMA injuries requiring surgical evacuation can be easily treated at the time of surgery. However, arterial injury in patients with nonsurgical epidural hematomas and underlying skull fractures may be underestimated. Active contrast extravasation was found in 71%,[
Of reported ruptured MMA pseudoaneurysm, it is estimated that 10% present with an IPH.[
Because MMA pseudoaneurysms are rare, the prognosis and treatment guidelines are somewhat controversial. The risk of re-hemorrhage in a previously ruptured traumatic pseudoaneurysm is unknown, and these lesions are characteristically unpredictable. Case reports have described spontaneous resolution/thrombosis of MMA pseudoaneurysms[
Traumatic MMA pseudoaneurysms can be treated through surgical resection or by endovascular means. The most common treatment modality used is endovascular embolization with tissue adhesive or hydrogel agents,[
CONCLUSIONS
Despite the unknown natural history of traumatic pseudoaneurysms, the potential for catastrophic bleeding exists, and treatment must be considered when discovered. A high index of suspicion should be maintained in the presence of a fracture overlying the MMA with an underlying IPH. CTA may suffice for screening, but in case of high suspicion, angiography should be considered. Surgical ligation of the MMA can be performed easily if hematoma evacuation is necessitated, but endovascular embolization is a safe and effective method for eliminating the hemorrhage risk in the presence of an MMA pseudoaneurysm if it is felt that surgical decompression is not mandatory.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Albert FK, Oldenkott P, Sigmund E. Subarachnoid hemorrhage and intracerebral hematoma in injury of the middle meningeal artery (aneurysma spurium). Zentralbl Neurochir. 1989. 50: 153-6
2. Benoit BG, Wortzman G. Traumatic cerebral aneurysms.Clinical features and natural history. J Neurol Neurosurg Psychiatry. 1973. 36: 127-38
3. Bozzetto-Ambrosi P, Andrade G, Azevedo-Filho H. Traumatic pseudoaneurysm of the middle meningeal artery and cerebral intraparenchymal hematoma: Case report. Surg Neurol. 2006. 66: S29-31
4. Bruneau M, Gustin T, Zekhnini K, Gilliard C. Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage: Case report and literature review. Surg Neurol. 2002. 57: 174-8
5. de Andrade AF, Figueiredo EG, Caldas JG, Paiva WS, De Amorim RL, Puglia P. Intracranial vascular lesions associated with small epidural hematomas. Neurosurgery. 2008. 62: 416-20
6. Freckmann N, Sartor K, Herrmann HD. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or dural sinuses. Acta Neurochir (Wien). 1981. 55: 273-81
7. Higazi I, el-Banhawy A, el-Nady F. Importance of angiography in identifying false aneurysm of the middle meningeal artery as a cause of extradural hematoma.Case report. J Neurosurg. 1969. 30: 172-6
8. Holmes B, Harbaugh RE. Traumatic intracranial aneurysms: A contemporary review. J Trauma. 1993. 35: 855-60
9. Jay J, Shapiro BM, Komisar A, Lawson W. Posttraumatic pseudoaneurysm of the extracranial middle meningeal artery. Arch Otolaryngol. 1985. 111: 264-6
10. Jussen D, Wiener E, Vajkoczy P, Horn P. Traumatic middle meningeal artery pseudoaneurysms: Diagnosis and endovascular treatment of two cases and review of the literature. Neuroradiology. 2012. 54: 1133-6
11. Kawaguchi T, Kawano T, Kaneko Y, Ooasa T, Ooigawa H, Ogasawara S. Traumatic lesions of the bilateral middle meningeal arteries – Case report. Neurol Med Chir (Tokyo). 2002. 42: 221-3
12. Ko JH, Kim YJ. Traumatic pseudoaneurysm of the middle meningeal artery with an arteriovenous fistula on a non-fractured site. Interv Neuroradiol. 2014. 20: 352-6
13. Kohyama S, Kakehi Y, Yamane F, Ooigawa H, Kurita H, Ishihara S. Subdural and intracerebral hemorrhage caused by spontaneous bleeding in the middle meningeal artery after coil embolization of a cerebral aneurysm. J Stroke Cerebrovasc Dis. 2014. 23: e433-5
14. Lim DH, Kim TS, Joo SP, Kim SH. Intracerebral hematoma caused by ruptured traumatic pseudoaneurysm of the middle meningeal artery: A case report. J Korean Neurosurg Soc. 2007. 42: 416-8
15. Markwalder H, Huber P. Aneurysms of the meningeal arteries. Schweiz Med Wochenschr. 1961. 91: 1344-7
16. Namba K, Ban S, Oda Y, Tazumi M, Ogata M. Case of traumatic false aneurysm of the middle meningeal artery with epidural hematoma - Comparison with a case resulting in spontaneous thrombosis. Rinsho Shinkeigaku. 1972. 12: 165-70
17. Nayil K, Ramzan A, Makhdoomi R, Wani A, Zargar J, Shaheen F. Incidental traumatic pseudoaneurysm of the middle meningeal artery: Case report and literature review. Turk Neurosurg. 2012. 22: 239-41
18. Okumura H, Tenjin H, Ueda S. A case of traumatic pseudoaneurysm of the middle meningeal artery treated with endovascular surgery. No Shinkei Geka. 1998. 26: 929-33
19. Paiva WS, Andrade AF, Amorim RL, Bor-Seng-Shu E, Gattas G, Neville IS. Computed tomography angiography for detection of middle meningeal artery lesions associated with acute epidural hematomas. Biomed Res Int 2014. 2014. p.
20. Pouyanne H, Leman P, Got M, Gouaze A. Traumatic arterial aneurysm of the left middle meningeal artery. Rupture one month after the accident. Temporal intracerebral hematoma. Intervention Neurochirurgie. 1959. 5: 311-5
21. Protasoni M, Sangiorgi S, Cividini A, Culuvaris GT, Tomei G, Dell’Orbo C. The collagenic architecture of human dura mater. J Neurosurg. 2011. 114: 1723-30
22. Rumbaugh CL, Bergeron RT, Kurze T. Intracranial vascular damage associated with skull fractures.Radiographic aspects. Radiology. 1972. 104: 81-7
23. Salazar Flores J, Vaquero J, Garcia Sola R, Rossi E, Martinez R, Martinez P. Traumatic false aneurysms of the middle meningeal artery. Neurosurgery. 1986. 18: 200-3
24. Schulze A. Unusual forms of epidural hematoma. Zentralbl Neurochir. 1957. 17: 40-7
25. Shah Q, Friedman J, Mamourian A. Spontaneous resolution of traumatic pseudoaneurysm of the middle meningeal artery. AJNR Am J Neuroradiol. 2005. 26: 2530-2
26. Singh M, Ahmad FU, Mahapatra AK. Traumatic middle meningeal artery aneurysm causing intracerebral hematoma: A case report and review of literature. Surg Neurol. 2006. 66: 321-3
27. Srinivasan A, Lesiuk H, Goyal M. Spontaneous resolution of posttraumatic middle meningeal artery pseudoaneurysm. AJNR Am J Neuroradiol. 2006. 27: 882-3
28. Vandenabeele F, Creemers J, Lambrichts I. Ultrastructure of the human spinal arachnoid mater and dura mater. J Anat. 1996. 189: 417-30
29. Wang CH, Lee HC, Cho DY. Traumatic pseudoaneurysm of the middle meningeal artery: Possible indicators for early diagnosis in the computed tomography era. Surg Neurol. 2007. 68: 676-81
30. Wu X, Jin Y, Zhang X. Intraparenchymal hematoma caused by rupture of the traumatic pseudoaneurysm of middle meningeal artery. J Craniofac Surg. 2014. 25: e111-3