- Department of Neurosurgery, Warren Alpert Medical School of Brown University, Providence, Rhode Island 02903, USA
Correspondence Address:
Adetokunbo A. Oyelese
Department of Neurosurgery, Warren Alpert Medical School of Brown University, Providence, Rhode Island 02903, USA
DOI:10.4103/2152-7806.181980
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Carnevale JA, Morrison JF, Choi DB, Klinge PM, Cosgrove GR, Oyelese AA. Self-inflicted nail-gun injury with cranial penetration and use of intraoperative computed tomography. Surg Neurol Int 06-May-2016;7:
How to cite this URL: Carnevale JA, Morrison JF, Choi DB, Klinge PM, Cosgrove GR, Oyelese AA. Self-inflicted nail-gun injury with cranial penetration and use of intraoperative computed tomography. Surg Neurol Int 06-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/self%e2%80%91inflicted-nail%e2%80%91gun-injury-with-cranial-penetration-and-use-of-intraoperative-computed-tomography/
Abstract
Background:Management of penetrating cranial trauma remains a high acuity and imaging intense neurosurgical disorder. Imaging of vital structures, including angiography, is typically conducted to understand the proximity of vital structures in comparison to a foreign body and prepare for intraoperative complications such as hemorrhage. Preservation of function following initial injury in cases where minimal neurological deficit exists is essential.
Case Description:Here, we present a case using intraoperative computed tomography to assist in early detection and resolution of hemorrhage in the surgical management of an intact patient with self-inflicted penetrating cranial trauma.
Conclusions:This method may aid in early detection of hemorrhage and prevention of consequential neurological deterioration or emergent need for secondary surgery.
Keywords: Brain trauma, intraoperative computed tomography, penetrating brain injury, self-harm disorder, self-inflicted injury
INTRODUCTION
Use of computed tomography (CT) in penetrating cranial injury has become the standard of care. This allows for localization of the path of the foreign body and indication for further imaging studies. Recently, use of intraoperative CT (IOCT) has become increasingly available in the neurosurgery armamentarium, allowing for real-time assessment of hemorrhage and noninvasive vascular studies during surgery.
Self-harm disorder is a psychiatric disorder defined as intentional, self-inflicted, injury without the intent of suicide, and covers a wide range of personal injuries such as cutting, burning, poisoning, or stabbing.[
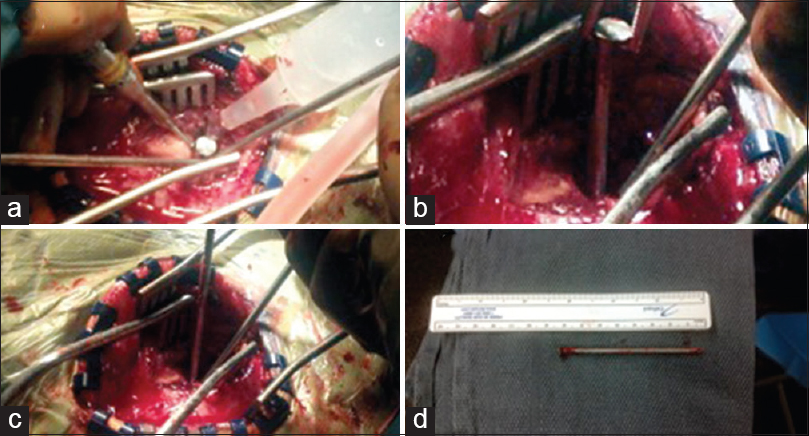
We describe a case wherein a patient with self-harm disorder, self-inflicts multiple nail-gun wounds including a penetrating cranial wound. This condition was operative and successfully treated with the assistance of portable IOCT allowing for both minimal cranial exposure and real-time diagnostic confirmation of hemorrhage free nail extraction.
CASE DESCRIPTION
History and examination
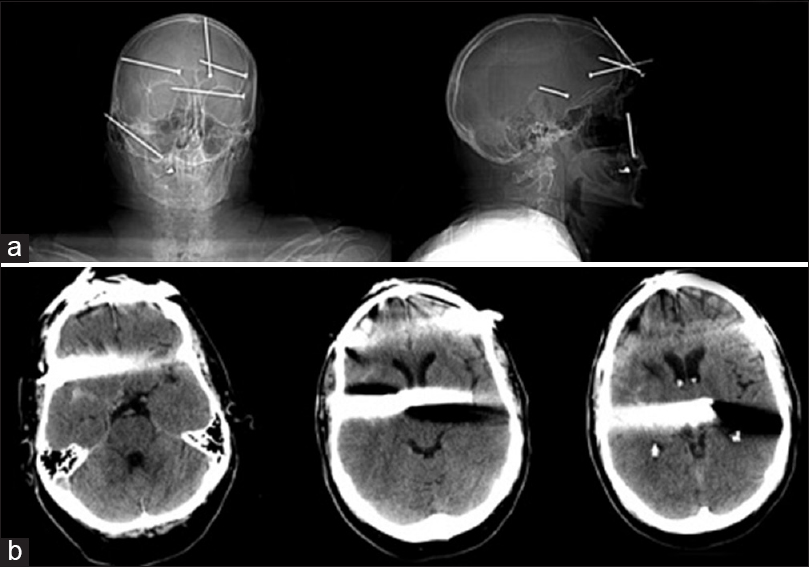
This 60-year-old right-handed male presented to the Emergency Department following self-inflicted injuries to the head, chest, and left arm with a pneumatic powered nail gun. On presentation, he denied suicidal or homicidal ideation. He had several previous demonstration of self-injury, including a table saw injury with distal amputation of left index finger. On presentation, he had a Glasgow Coma Scale (GCS) of 15, several puncture wounds throughout the face and head, and full motor and sensation throughout upper and lower extremities. CT of the brain at admission was consistent with five large nails projected over the face and calvarium [
Figure 1
Computed tomographic examination of the brain. (a) Scout views, anterior/posterior and lateral with multiple cranial nails. (b) Axial computed tomography views upon initial presentation consistent with a right temporal penetrating wound extending through the right and left lateral ventricles to the left basal ganglia with streak artifact from metal within the missile
Operative technique
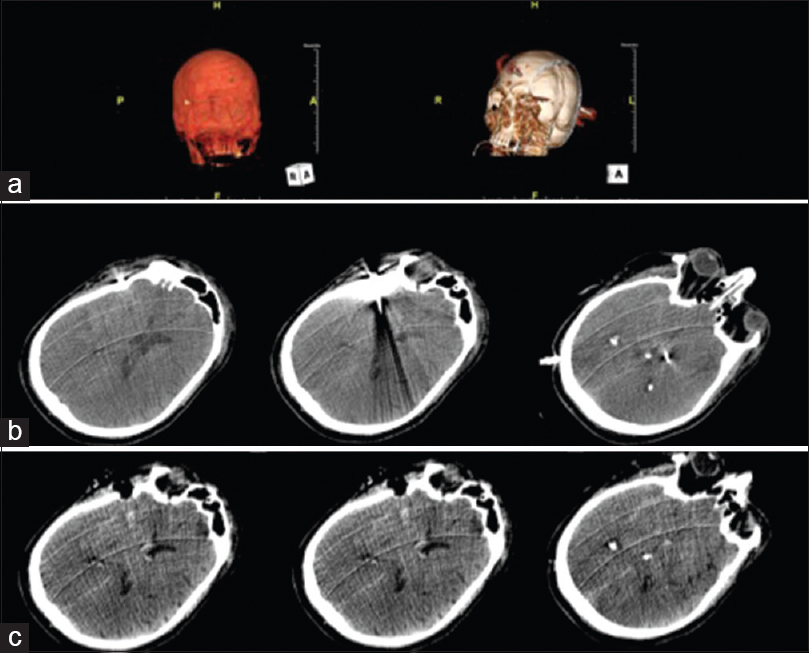
The facial and chest subcutaneous nails were removed at the bedside with sterile technique under local anesthesia. We elected to remove the intracranial nail in the operating room (OR), under general anesthesia, to allow for a controlled, sterile, environment, and possible conversion to craniotomy should hemorrhage occur. A right temporal approach was used with intraoperative 32-slice BodyTom CT (Neurologica, Danvers, MA, USA) imaging. The BodyTom is a portable, full-bore CT-imaging device that can be utilized in any OR. Use of portable intraoperative imaging was chosen for convenience and patient safety, allowing for pre- and post-removal imaging in the operating theater while the patient and instruments remained sterile as well as real-time three-dimensional imaging reconstruction [
Postoperative course
Following the neurosurgical procedure, the patient directly underwent removal of the left humerus nail. Thereafter, he returned to the Neurosusrgery Intensive Care Unit. Infectious disease evaluation was requested for low velocity penetrating cranial injury. Vancomycin, cefepime, and metronidazole were initiated for broad spectrum antibiotic coverage. The patient remained GCS 15, ambulatory, and medically stable and was discharged to an inpatient psychiatry unit on postoperative day 3. Postoperative angiogram was deferred to follow-up. However, the patient was subsequently lost to follow-up.
DISCUSSION
These results suggest that further use of IOCT in penetrating cranial injury could provide useful diagnostic information that may mitigate the need for further procedures due to unseen intraoperative complications. IOCT allows for real-time visualization of acute changes in intracranial processes which are not necessarily evident from surface anatomy in surgical cases with limited exposure.
Removal of low velocity penetrating cranial missiles typically is undertaken either under local anesthesia at bedside or in the OR via craniotomy.[
Perioperative imaging has long been used in both penetrating and nonpenetrating brain injury. Studies are undertaken immediately postoperatively to rule out intraoperative hemorrhage, at the interval with mental status changes, or to evaluate for posttraumatic pseudoaneurysm.[
Dedicated operative suites for intraoperative magnetic resonance imaging or CT have been created for procedures augmented by these imaging modalities. These facilities, however, require a dedicated space and significant capital outlay.[
This study represents not only the first report of use of IOCT in penetrating cranial injury but also the first use of portable IOCT for acute brain pathology. It supports the use of IOCT in patients with penetrating cranial injuries to allow for early identification of surgical complications and minimal cranial exposure and parenchymal manipulation. This portends to decreased hospital stay and ultimately, better outcome and warrants further investigation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Blankenship BA, Baxter AB, McKahn GM. Delayed cerebral artery pseudoaneurysm after nail gun injury. AJR Am J Roentgenol. 1999. 172: 541-2
2. Braca J, Whapham J, Prabhu V. E-035 Ghost image extraction technique utilizing intraoperative angiography for the controlled removal of an intracranial nail. J NeuroInterv Surg. 2012. 4: A60-1
3. Edlich RF, Silloway KA, Rodeheaver GT, Morgan RF, Birk K, Thacker JG. Industrial nail gun injuries. Compr Ther. 1986. 12: 42-6
4. Englot DJ, Laurans MS, Abbed K, Bulsara KR. Removal of nail penetrating the basilar artery. Neurosurg Rev. 2010. 33: 501-4
5. Herpertz S. Self-injurious behaviour. Psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatr Scand. 1995. 91: 57-68
6. McCorkell SJ, Harley JD, Cummings D. Nail-gun injuries. Accident, homicide, or suicide?. Am J Forensic Med Pathol. 1986. 7: 192-5
7. Musa BS, Simpson BA, Hatfield RH. Recurrent self-inflicted craniocerebral injury: Case report and review of the literature. Br J Neurosurg. 1997. 11: 564-9
8. Sakuta Y, Arai S. Penetrating brain injury and traumatic aneurysm caused by a nail gun. No Shinkei Geka. 1997. 25: 357-62
9. Salar G, Costella GB, Mottaran R, Mattana M, Gazzola L, Munari M. Multiple craniocerebral injuries from penetrating nails. Case illustration. J Neurosurg. 2004. 100: 963-
10. Sutherland GR, Louw DF. Intraoperative MRI: A moving magnet. CMAJ. 1999. 161: 1293-
11. Tormenti MJ, Kostov DB, Gardner PA, Kanter AS, Spiro RM, Okonkwo DO. Intraoperative computed tomography image-guided navigation for posterior thoracolumbar spinal instrumentation in spinal deformity surgery. Neurosurg Focus. 2010. 28: E11-
12. Uhl E, Zausinger S, Morhard D, Heigl T, Scheder B, Rachinger W. Intraoperative computed tomography with integrated navigation system in a multidisciplinary operating suite. Neurosurgery. 2009. 64: 231-9