- Department of Neurosurgery, University Hospital, Linköping, Sweden
Correspondence Address:
Johanna Eneling
Department of Neurosurgery, University Hospital, Linköping, Sweden
DOI:10.4103/2152-7806.196369
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Johanna Eneling, Per M. Karlsson, Sandro Rossitti. Sphenopalatine arteriovenous fistula complicating transsphenoidal pituitary surgery: A rare cause of delayed epistaxis treatable by endovascular embolization. 21-Dec-2016;7:
How to cite this URL: Johanna Eneling, Per M. Karlsson, Sandro Rossitti. Sphenopalatine arteriovenous fistula complicating transsphenoidal pituitary surgery: A rare cause of delayed epistaxis treatable by endovascular embolization. 21-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/sphenopalatine-arteriovenous-fistula-complicating-transsphenoidal-pituitary-surgery-a-rare-cause-of-delayed-epistaxis-treatable-by-endovascular-embolization/
Abstract
Background:Vascular injuries in transsphenoidal surgery for pituitary adenomas are uncommon but can result in serious disability or death.
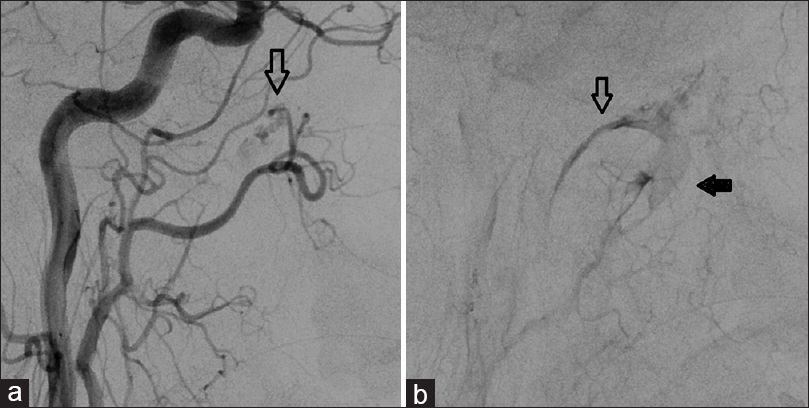
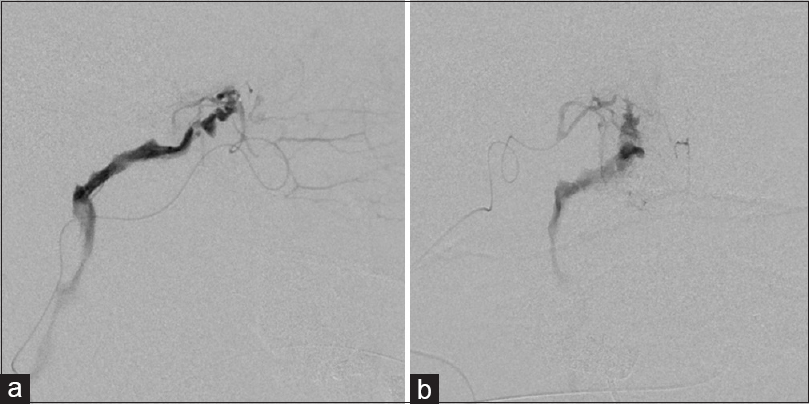
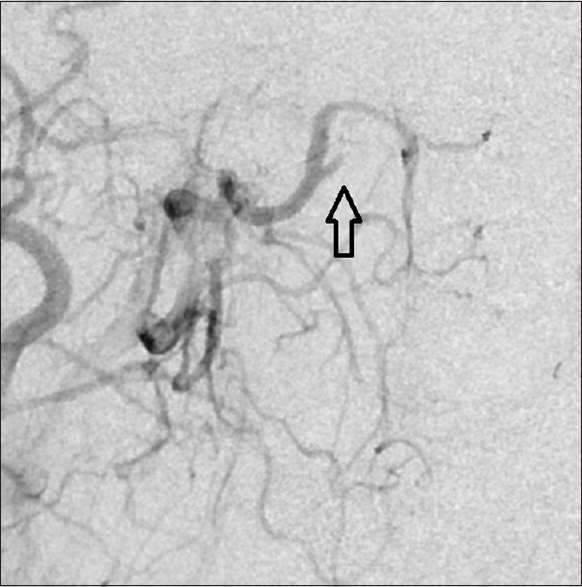
Case Description:A 46-year-old man, who underwent resection of a pituitary adenoma with suprasellar extension via a transsphenoidal approach, presented with massive epistaxis five days postoperatively. Angiography revealed an arteriovenous fistula (AVF) between the right sphenopalatine artery and a deep vein draining to the right internal jugular vein, as well as contrast agent extravasation at the fistula point. The AVF was catheterized and successfully occluded with N-butyl-2-cyanoacrylate.
Conclusions:Transsphenoidal pituitary surgery can be complicated by massive epistaxis from a lesion of a small branch of the external carotid artery. Airway protection through intubation and investigation with conventional digital subtraction angiography is recommended. The treatment of choice is endovascular embolization because it can be done immediately at the angiography suite.
Keywords: Complication, epistaxis, pituitary adenoma, sphenopalatine artery, transsphenoidal surgery
INTRODUCTION
Transsphenoidal pituitary surgery has a low complication rate. However when complications do occur they can be devastating and, in the case of vascular injury, potentially lethal. When postoperative epistaxis occurs, a much feared cause is a ruptured pseudoaneurysm of the internal carotid artery. Immediate angiographic investigation should be performed on all patients that develop postoperative epistaxis in the aftermath of transsphenoidal pituitary surgery.[
This article presents, to the best of the authors’ knowledge, the first case of postoperative delayed massive epistaxis from an iatrogenic sphenopalatine arteriovenous fistula after transsphenoidal pituitary surgery.
CASE REPORT
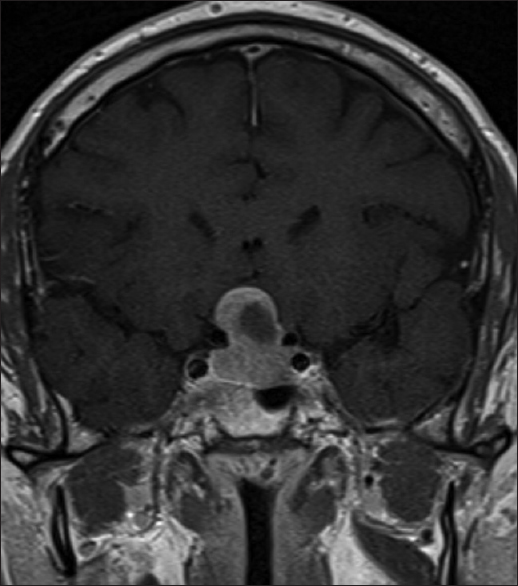
A previously healthy 46-year-old man was referred to our clinic because of visual symptoms and a nonfunctional pituitary adenoma with suprasellar growth that compressed the optic chiasm [
DISCUSSION
Transsphenoidal pituitary surgery is considered to be a safe procedure with reported mortality rates at approximately 1%. Complications include anterior pituitary insufficiency, diabetes insipidus, cerebrospinal fluid fistulas and, less commonly, carotid artery injuries, hypothalamic injuries, loss of vision, and meningitis.[
Arteriovenous fistulas are direct connections between high-pressure arteries and low-pressure veins that bypass the capillary bed. A post-traumatic (or, as in the current case, iatrogenic) arteriovenous fistula can be caused by both penetrating and nonpenetrating trauma to an artery and an adjacent vein, and can develop immediately following injury or in a delayed fashion from a post-traumatic pseudoaneurysm.[
The sphenopalatine artery is the terminal branch of the internal maxillary artery and provides arterial supply to the nasal mucosa. It passes through the sphenopalatine foramen and divides into medial (septal) and lateral branches, the latter giving off branches to the superior, middle, and inferior nasal conchae.[
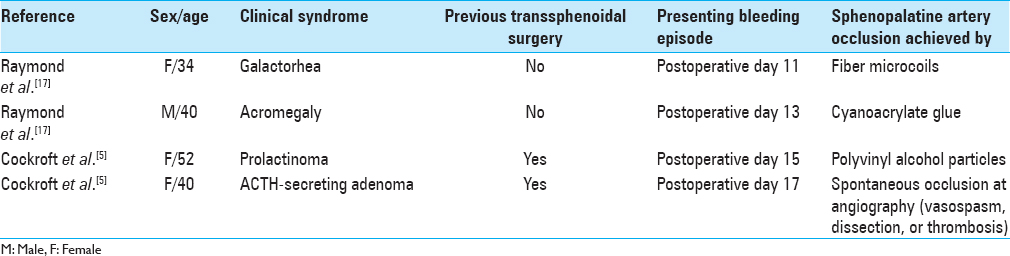
Reports of sphenopalatine artery injuries in relation to transsphenoidal pituitary surgery are much less common than those of the internal carotid artery. We have found a total of 4 patients in two reports who developed angiographically diagnosed sphenopalatine artery pseudoaneurysms after transsphenoidal surgery for pituitary adenomas.[
The decision to let the patient undergo a CT angiography instead of taking him straight to the endovascular suite for DSA can, in retrospect, be viewed as questionable. It did cause a delay in definitive treatment and added an unnecessary contrast bolus. In a patient with life-threatening epistaxis, CT angiography should not be allowed to delay DSA and final treatment of the source of bleeding.
CONCLUSION
Massive postoperative epistaxis following transsphenoidal pituitary surgery requires swift treatment with immediate intubation to secure the airway, bleeding control through nasopharyngeal packing, and investigation with angiography. In this situation, a CT angiography is superfluous and a DSA is the investigation of choice. Although less common, massive epistaxis can result from lesions of a small branch of the external carotid artery such as the sphenopalatine artery. The treatment of choice, because it can be done almost without delay after diagnosis at the angiography suite, is endovascular embolization. There are many endovascular techniques available such as liquid embolics, particles, or coils that can be used. In the present case, embolization with N-butyl-2-cyanoacrylate was a successful method.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Berker M, Aghayev K, Saatci I, Palaoğlu , Önerci M. Overview of vascular complications of pituitary surgery with special emphasis on unexpected abnormality. Pituitary. 2010. 13: 160-7
2. Campbell RG. Sphenopalatine artery pseudoaneurysm after endoscopic sinus surgery: A case report and literature review. Ear Nose Throat J. 2012. 91: E4-11
3. Çinar C, Bozkaya H, Parildar M, Oran I. Endovascular management of vascular injury during transphenoidal surgery. Interv Neuroradiol. 2013. 19: 102-9
4. Ciric I, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: Results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997. 40: 225-36
5. Cockroft KM, Carew JF, Trost D, Fraser R. Delayed epistaxis resulting from external carotid artery injury requiring embolization: A rare complication of transsphenoidal surgery: Case report. Neurosurgery. 2000. 47: 236-9
6. Cohen S, Anastassov GE, Chuang SK. Posttraumatic pseudoaneurysm of the sphenopalatine artery presenting as persistent epistaxis: Diagnosis and management. J Trauma. 1999. 47: 396-9
7. Golshani K, Britz GW, Yoo A, West GA, Winn HR.editors. Traumatic cerebral aneurysms secondary to penetrating intracranial injuries. Youmans Neurological Surgery. Philadelphia, PA: Saunders, Elsevier Inc; 2011. p. 4000-1
8. Gökdoðan O, Kizil Y, Aydil U, Karamert R, Uslu S, Ileri F. Sphenopalatine artery pseudoaneurysm: A rare cause of intractable epistaxis after endoscopic sinus surgery. J Craniofac Surg. 2014. 25: 539-41
9. Halbach W, Hiqashida RT, Hieshima GB, Hardin CW. Arteriovenous fistula of the internal maxillary artery: Treatment with transarterial embolization. Radiology. 1988. 168: 443-5
10. Jane JA, Thapar K, Laws ER, Winn HR.editors. Pituitary tumors: Functioning and nonfunctioning. Youmans Neurological Surgery. Philadelphia: Elsevier Saunders; 2011. p. 1491-2
11. Jho DH, Jho DH, Jho HD, Quiñones-Hinojosa A.editors. Endoscopic endonasal pituitary and skull base surgery. Schmidek & Sweet Operative Neurosurgical Techniques. Philadelphia, PA: Elsevier Saunders; 2012. p. 260-1
12. Kim YW, Baek MJ, Kim HD, Cho KS. Massive epistaxis due to pseudoaneurysm of the sphenopalatine artery: A rare post-operative complication of orthognathic surgery. J Laryngol Otol. 2013. 27: 610-3
13. Luo CB, Teng MM, Chang FC, Chang CY. Transarterial embolisation of acute external carotid blowout syndrome with profuse oronasal bleeding by N-butyl-cyanoacrylate. Am J Emerg Med. 2006. 24: 702-8
14. Martin-Granizo R, Caniego JL, de Pedro M, Dominguez L. Arteriovenous fistula after temporomandibular joint arthroscopy successfully treated with embolization. Int J Oral Maxillofac Surg. 2004. 33: 301-3
15. Mitchell RN, Kumar V, Abbas AK, Aster JC.editors. Blood vessels. Robbins and Cotran Pathologic Basis of Disease. Philadelphia: Elsevier Saunders; 2015. p. 483-522
16. Procopio O, Fusetti S, Liessi G, Ferronato G. False aneurysm of the sphenopalatine artery after Le Fort I osteotomy: Report of 2 cases. J Oral Maxillofac Surg. 2003. 61: 520-4
17. Raymond J, Hardy J, Czepko R, Roy D. Arterial injuries in transsphenoidal surgery for pituitary adenoma: The role of angiography and endovascular treatment. AJNR Am J Neuroradiol. 1997. 18: 655-65
18. Salomon G, Faure J, Raybaud C, Grisoli F, Newton TH, Potts G.editors. The external carotid artery. Section I: Normal external carotid artery. Radiology of the skull and brain. St. Louis: Mosby; 1974. 2: 1246-74
19. Takeuchi S, Takasato Y. Iatrogenic arteriovenous fistula of the superficial temporal artery after manual reduction of temporomandibular joint dislocation. J Craniofac Surg. 2011. 22: 1959-61