- Department of Neurosurgery, Queen's Hospital, Essex Neuroscience Centre, Romford, London, UK
Correspondence Address:
Rossana Romani
Department of Neurosurgery, Queen's Hospital, Essex Neuroscience Centre, Romford, London, UK
DOI:10.4103/2152-7806.182740
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Romani R, Pollock J. Spontaneous shrinkage of vestibular schwannoma. Surg Neurol Int 19-May-2016;7:59
How to cite this URL: Romani R, Pollock J. Spontaneous shrinkage of vestibular schwannoma. Surg Neurol Int 19-May-2016;7:59. Available from: http://surgicalneurologyint.com/surgicalint_articles/spontaneous-shrinkage-of-vestibular-schwannoma/
Abstract
Background:“Watch, wait, and rescan” (WWR) has an established place as a successful management option for a significant proportion of vestibular schwannomas (VS) as an alternative to microsurgical removal or stereotactic radiotherapy. VS may grow slowly and continuously, followed by stagnation or even shrinkage. We present two case reports of spontaneous shrinkage of VS along with a review of the literature.
Case Description:A 29-year-old female presented with a progressive history of visual blurring and intermittent diplopia over 2 months. A 29 mm of maximum intracranial diameter (ICD) VS with secondary obstructive hydrocephalus was diagnosed. The patient underwent a ventriculo-peritoneal shunt with resolution of her symptoms and opted for initial WWR management. Interval scanning between 2007 and 2014 showed progressive reduction in the maximum ICD together with reduction in the degree of central tumor enhancement. Maximum ICD at most recent follow up was 22 mm. A 28-year-old female was referred with right sensorineural deafness. A right VS of maximum ICD of 27 mm was diagnosed. Initial WWR management was planned after discussion. Serial imaging showed an initial increase in the size of the tumor followed by progressive reduction in size. The most recent follow up showed a maximum ICD of 20 mm.
Conclusion:Early WWR management can be associated with spontaneous shrinkage of VS over time. Prospective clinical study of larger numbers of such cases using the UK VS database may help to identify predictive factors for the spontaneous regression of VS.
Keywords: Conservative treatment, neurinoma, spontaneous shrinkage, vestibular schwannoma, watch, wait, rescan
INTRODUCTION
Vestibular schwannomas (VS) are benign, slow-growing tumors, which originate in the transition zone between the central and peripheral myelin of the vestibular branches of cranial nerve VIII.[
Non-surgical management with “watch, wait, and rescan” (WWR) policy is a frequent option, especially in asymptomatic patients,[
CASE DESCRIPTION
Case report 1
A 29-year-old female patient presented with a progressive history of visual blurring and double vision over 2 months in 2006. She was assessed by an optician who noted bilateral papilloedema. Clinical assessment performed in our hospital confirmed the presence of bilateral Grade 2 papilloedema. She had preserved speech discrimination on the right and double vision on the extreme left lateral downgaze. Audiometry in February 2007 showed slight loss of hearing on the right with no apparent high tone preponderance. MRI in 2007 disclosed a lesion in the right cerebellopontine angle (CPA) of maximum intracranial diameter (ICD) of 29 mm in continuity with the acoustic nerve, with associated secondary hydrocephalus [
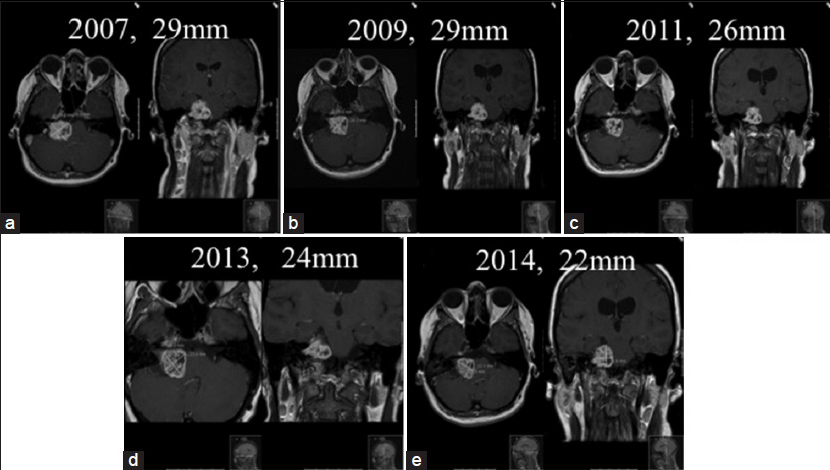
Figure 1
Right medium-sized (29 mm) vestibular schwannoma in 2007 (a) remaining stable in size in 2009 (b) and then showing a progressive reduction in the maximum intracranial diameter with conspicuous reduction in the degree of central tumor enhancement (c and d). Maximum intracranial diameter of 22 mm at most recent follow-up (e)
Following surgery, the papilloedema and the diplopia resolved. Computed tomography (CT) scan showed immediate improvement in the hydrocephalus. Following the complete resolution of her symptoms, the patient was managed with WWR. The tumor remained stable in ICD for 2 years with a maximum ICD of 29 mm [
Case report 2
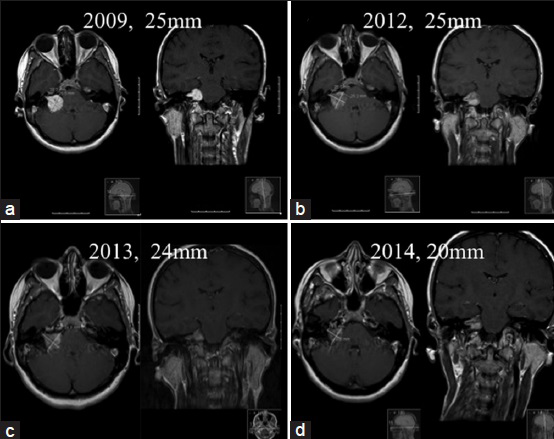
A 28-year-old female was referred to us by an ENT surgeon for right-sided hearing loss with preservation of speech discrimination. There was no impairment of coordination. A CT scan demonstrated the presence of a right VS with an extrameatal component in the CPA of maximum ICD of 25 mm [
DISCUSSION
Watch, wait, and rescan has an established place as a successful treatment option for a significant proportion of small VSs, as an alternative to microsurgical removal or stereotactic radiotherapy.[
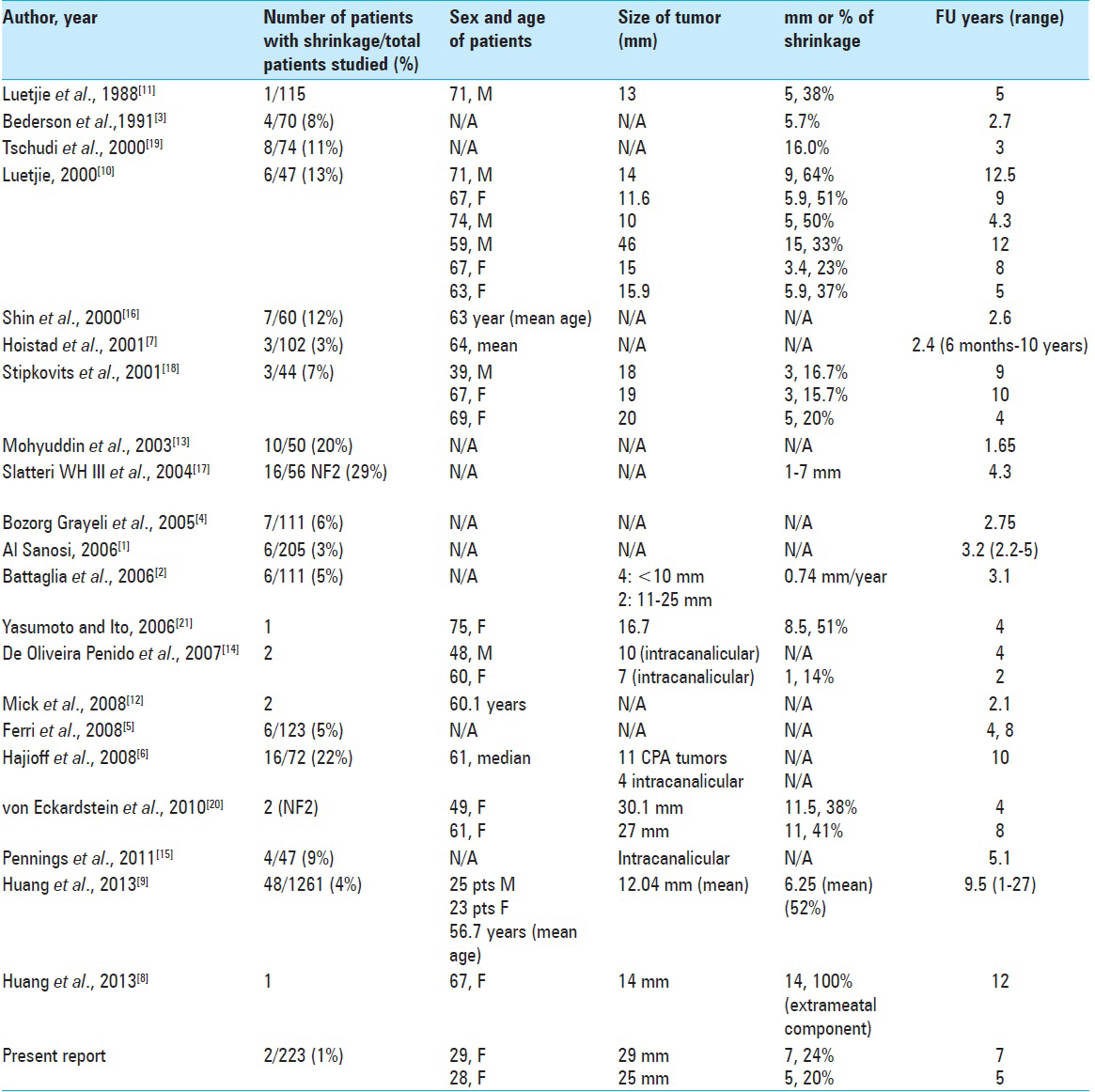
In 21 previous studies, between 1988 and 2013, the incidence of shrinkage of these tumors ranged between 1 and 29% during follow-up of 6 months to 27 years. The degree of tumor shrinkage identified ranged between 5.38 and 100% during the same follow-up period.[
Tumor size can be classified as follows: Intracanalicular, small (<10 mm)-, medium (range, 11–25 mm)-, large (range, 25–40 mm)-, giant (>40 mm)-sized neurinoma.[
In the present report, we assessed tumor size by measurement of the largest CPA tumor diameter, as reported by Rosenberg in 2000.[
Intracanalicular tumors tend to exhibit a slow growth rate, as reported by several authors.[
In patients affected by neurofibromatosis type 2 (NF2) with bilateral VSs, the gene responsible for NF2 is known to be localized on chromosome 22;[
The mechanism of tumor shrinkage is not well understood. Environmental factors and/or genetic-molecular hypothesis should be considered. A reduction in vascular supply is hypothesized, which could lead to ischemic necrosis and fibrosis with associated shrinkage.[
CONCLUSIONS
We would endorse the value of a WWR policy as a valid current treatment option for VS. This should be always considered in patients with small- or medium-sized tumors, with minimum or absent symptoms. We have shown that significant spontaneous tumor shrinkage can occur even in medium-sized VS, and we recommend that patients should be followed up for a minimum of 4 years to seek evidence of this. Furthermore, initial growth of the tumor may not always mandate active treatment even in young patients or in patients with a significant CPA component.
Prospective multicentre studies with a large number of patients such as the UK vestibular schwannoma database will be a valuable future aid in identifying predictive factors for tumor shrinkage. In young patients with an anticipated long-term follow-up, there may be merit in considering biopsy in selected cases for a better understanding of the mechanism of shrinkage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al Sanosi A, Fagan PA, Biggs ND. Conservative management of acoustic neuroma. Skull Base. 2006. 16: 95-100
2. Battaglia A, Mastrodimos B, Cueva R. Comparison of growth patterns of acoustic neuromas with and without radiosurgery. Otol Neurotol. 2006. 27: 705-12
3. Bederson JB, von Ammon K, Wichmann WW, Yasargil MG. Conservative treatment of patients with acoustic tumors. Neurosurgery. 1991. 28: 646-50
4. Bozorg Grayeli A, Kalamarides M, Ferrary E, Bouccara D, El Gharem H, Rey A. Conservative management versus surgery for small vestibular schwannomas. Acta Otolaryngol. 2005. 125: 1063-8
5. Caye-Thomasen P, Dethloff T, Hansen S, Stangerup SE, Thomsen J. Hearing in patients with intracanalicular vestibular schwannomas. Audiol Neurootol. 2007. 12: 1-12
6. Charabi S, Thomsen J, Tos M, Charabi B, Mantoni M, Børgesen SE. Acoustic neuroma/vestibular schwannoma growth: Past, present and future. Acta Otolaryngol. 1998. 118: 327-32
7. Ferri GG, Modugno GC, Pirodda A, Fioravanti A, Calbucci F, Ceroni AR. Conservative management of vestibular schwannomas: An effective strategy. Laryngoscope. 2008. 118: 951-7
8. Graamans K, Van Dijk JE, Janssen LW. Hearing deterioration in patients with a non-growing vestibular schwannoma. Acta Otolaryngol. 2003. 123: 51-4
9. Hajioff D, Raut VV, Walsh RM, Bath AP, Bance ML, Guha A. Conservative management of vestibular schwannomas: Third review of a 10-year prospective study. Clin Otolaryngol. 2008. 33: 255-9
10. Hoistad DL, Melnik G, Mamikoglu B, Battista R, O’Connor CA, Wiet RJ. Update on conservative management of acoustic neuroma. Otol Neurotol. 2001. 22: 682-5
11. Huang X, Caye-Thomasen P, Stangerup SE. Distinct spontaneous shrinkage of a sporadic vestibular schwannoma. Auris Nasus Larynx. 2013. 40: 243-6
12. Huang X, Caye-Thomasen P, Stangerup SE. Spontaneous tumor shrinkage in 1261 observed patients with sporadic vestibular schwannoma. J Laryngol Otol. 2013. 127: 739-43
13. Luetje CM. Spontaneous involution of acoustic tumors. Am J Otol. 2000. 21: 393-8
14. Luetje CM, Whittaker CK, Davidson KC, Vergara GG. Spontaneous acoustic tumor involution: A case report. Otolaryngol Head Neck Surg. 1988. 98: 95-7
15. Mick P, Westerberg BD, Ngo R, Akagami R. Growing vestibular schwannomas: What happens next?. Otol Neurotol. 2009. 30: 101-4
16. Mohyuddin A, Vokurka EA, Evans DG, Ramsden RT, Jackson A. Is clinical growth index a reliable predictor of tumor growth in vestibular schwannomas?. Clin Otolaryngol Allied Sci. 2003. 28: 85-90
17. Neff BA, Welling DB, Akhmametyeva E, Chang LS. The molecular biology of vestibular schwannomas: Dissecting the pathogenic process at the molecular level. Otol Neurotol. 2006. 27: 197-208
18. Penido Nde O, Tangerina RP, Kosugi EM, Abreu CE, Vasco MB. Vestibular schwannoma: Spontaneous tumor involution. Braz J Otorhinolaryngol. 2007. 73: 867-71
19. Pennings RJ, Morris DP, Clarke L, Allen S, Walling S, Bance ML. Natural history of hearing deterioration in intracanalicular vestibular schwannoma. Neurosurgery. 2011. 68: 68-77
20. Rosenberg SI. Natural history of acoustic neuromas. Laryngoscope. 2000. 110: 497-508
21. Shin YJ, Fraysse B, Cognard C, Gafsi I, Charlet JP, Berges C. Effectiveness of conservative management of acoustic neuromas. Am J Otol. 2000. 21: 857-62
22. Slattery WH 3 r rd, Fisher LM, Iqbal Z, Oppenhiemer M. Vestibular schwannoma growth rates in neurofibromatosis type 2 natural history consortium subjects. Otol Neurotol. 2004. 25: 811-817
23. Stangerup SE, Caye-Thomasen P, Tos M, Thomsen J. The natural history of vestibular schwannoma. Otol Neurotol. 2006. 27: 547-52
24. Stipkovits EM, Graamans K, Van Dijk JE. Vestibular schwannoma: Negative growth and audiovestibular features. Eur Arch Otorhinolaryngol. 2001. 258: 467-71
25. Tschudi DC, Linder TE, Fisch U. Conservative management of unilateral acoustic neuromas. Am J Otol. 2000. 21: 722-28
26. von Eckardstein KL, Beatty CW, Driscoll CL, Link MJ. Spontaneous regression of vestibular schwannomas after resection of contralateral tumor in neurofibromatosis Type 2. J Neurosurg. 2010. 112: 158-62
27. Yasumoto Y, Ito M. Spontaneous regression of a growing vestibular schwannoma. Neurol Med Chir (Tokyo). 2006. 46: 601-4






Virginia Aschieri
Posted February 8, 2022, 3:46 pm
Nice work. I am a patient with a 2.5 max diameter VS, 52 years. Despite my Doctor recommendation to undergo a surgery, I go for they WWR attitude. I was diagnosed in 2019, and 4 MR controls showed no changes in 2 years.
Would like yo learn more about what can help in shrinking..
Sandra McHugh
Posted April 20, 2023, 12:51 pm
2016 14 x 8×8
2017 12x 9×8
2020 9x7x6
2023 9×7 x6
Yes, it is shrinking with no treatment. Diagnosed in 2016- now a 71 year old female- doing great. Thank you for your article. Sandra