- Department of Neurology-Neurosurgery-Psychiatry, Faculty of Medicine, University of Medicine in Tirana, Tirana, Albania
- Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine in Tirana, Tirana, Albania
Correspondence Address:
Gentian Vyshka
Department of Biomedical and Experimental, Faculty of Medicine, University of Medicine in Tirana, Tirana, Albania
DOI:10.4103/2152-7806.184264
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seferi A, Alimehmeti R, Pajaj E, Vyshka G. Superficial temporal artery pseudoaneurysm presenting as a growing, pulsatile, and tender mass. Surg Neurol Int 17-Jun-2016;7:66
How to cite this URL: Seferi A, Alimehmeti R, Pajaj E, Vyshka G. Superficial temporal artery pseudoaneurysm presenting as a growing, pulsatile, and tender mass. Surg Neurol Int 17-Jun-2016;7:66. Available from: http://surgicalneurologyint.com/surgicalint_articles/superficial-temporal-artery-pseudoaneurysm-presenting-as-a-growing-pulsatile-and-tender-mass/
Abstract
Background:Superficial temporal artery (STA) pseudoaneurysms have been reported in the literature since the mid of seventeenth century from Bartholin, however, there is an increasing number of cases, suggesting a diversity of etiological factors. Among these, traumatic events, even of an iatrogenic nature, have been identified as causative factors for nonspontaneous STA pseudoaneurysms. Regional pain and tenderness, troublesome pulsations of the mass, cosmetic concerns as well as the risk of bleeding warrant a thorough evaluation and a definite interventional approach to the condition.
Case Description:A 21-year-old Caucasian male searched medical advice for a growing, tender, and pulsatile mass on his right temple, with isolated and short episodes of lancinating sensations, after sustaining a blunt trauma following a hit with a stick half a year before the admission. Enhanced cranial computed tomography and angiography confirmed the diagnosis of an STA pseudoaneurysm. A direct percutaneous aspiration, as well as ultrasonography, was performed prior to the neurosurgical intervention, with the complete removal of the mass.
Conclusions:STA pseudoaneurysms require a careful evaluation and a conclusive approach in order to avoid the risk of a growing mass and other nonremote complications such as bone erosions and bleeding. Different treatment options are available, including endovascular obliteration and embolization, however, surgical removal after ligation of the afferent and efferent segments of the vessel seem to be highly effective.
Keywords: Blunt trauma, embolization, needle aspiration, superficial temporal artery pseudoaneurysm, surgical removal
INTRODUCTION
Superficial temporal artery (STA) pseudoaneurysms are rare occurrences, with some several hundred cases reported in the literature. The history of the first ever described aneurysm of temporal artery dates back to the first middle of the seventeenth century, and is related to the work of Thomas Bartholin.[
Albeit relatively rarely reported, the propensity of the STA to form pseudoaneurysms might well be related to the fact that the vessel, in its superficial course, lies directly over the periosteum at the superior temporal line, which renders it vulnerable to trauma.[
CASE REPORT
A 21-year-old Caucasian male was admitted to our Department with a 6-month history of a growing and pulsatile mass on the right temple. The mass was tender but not painful, although the patient referred isolated episodes of lancinating ache in his right hemicranium that subsided spontaneously. The patient sustained a blunt trauma after being hit with a stick 6 months prior to the admission. The contusion at that time resolved uneventfully 2 weeks after the trauma, however, a small pulsatile nodule remained, whose dimensions kept increasing.
The physical examination revealed a 10 × 14 mm sized pulsatile mass on the right temple, within the course of the anterior branch of STA. A direct percutaneous puncture and aspiration was performed within the neurosurgical facility, however, the dimensions of the mass remained unchanged after the procedure.
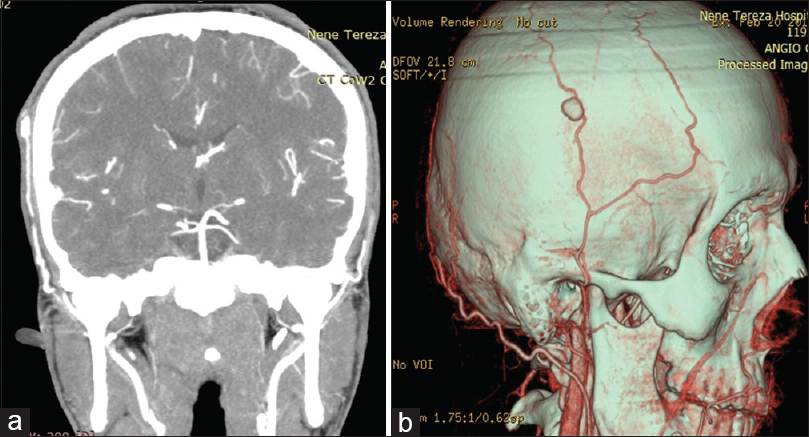
Transcutaneous sonography was highly suggestive for the presumptive diagnosis of STA aneurysm; after that, a computed tomography (CT) angiography with three-dimensional reconstruction visualized a pseudoaneurysm of the parietal division of the right STA. The enhanced CT image and the reconstruction of the mass in the angiography are presented in
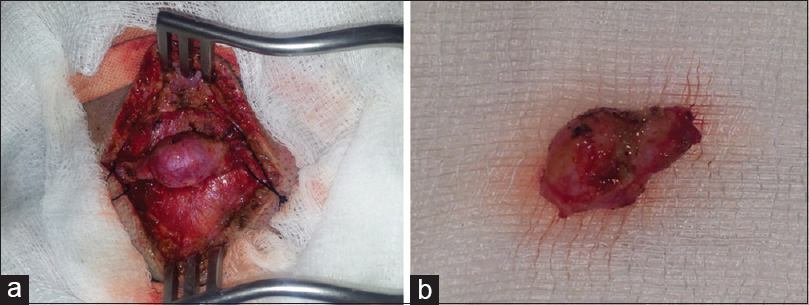
The patient underwent surgery under general anesthesia. The lesion was incised with the patient in a right lateral decubitus, with the incision covering the entire length of the aneurysm (afferent and efferent portions of STA), and reaching approximately 20 mm in our intervention. The entire pseudoaneurysm formation was surgically prepared, after we initially ligated the vessel proximally 5 mm from its sac, where the arterial structure was macroscopically intact. A distal ligature followed, with the removal of the entire mass [
The wound was carefully sutured for an optimal cosmetic outcome, with the patient discharged the day after. In two successive follow-ups (the first 2 months after suture removal, the second after 6 months), the patient had no clinical problems on the right temporal region.
DISCUSSION
After the remote trauma 6 months before, the small remaining nodule over the right temporal region did not interested that much to our patient. That was until some weeks prior to the intervention because the mass grew in dimensions to become visible from a certain distance and to create cosmetic concerns. In addition, the patient felt uneasy to sleep over his right temple, with an uncomfortable but not really painful sensation. These were the reasons for seeking neurosurgical advice, and thereafter for undergoing to intervention we described above.
In fact, reducing the risk of hemorrhage through a potential rupture of the formation, pain and headache relief, and resolving any cosmetic defects are the main objectives of surgical treatment of STA.[
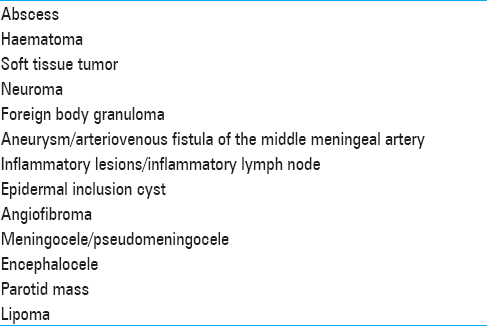
A careful differential diagnosis prior to the intervention, and an overall evaluation of potential conservative options of treatment, need to be performed as well.
CONCLUSIONS
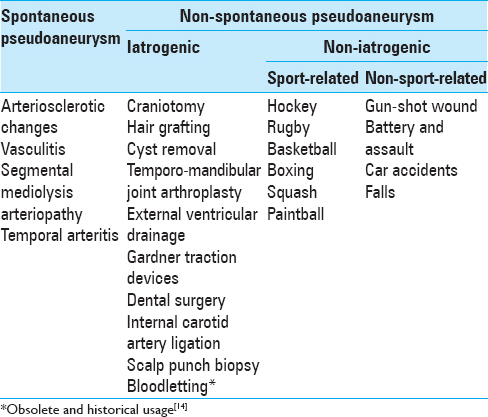
STA pseudoaneurysms are a rare occurrence following traumatic events or other conditions [
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alvarez H, Bravo M, Arancibia N, Chacon G. Superficial temporal artery pseudoaneurysm: Case report and review of the literature. Rev Chilena de Cirugia. 2006. 58: 469-72
2. Andreoli A, Tognetti F, Lanzino G. Traumatic aneurysm of the superficial temporal artery from fist injury. Br J Neurosurg. 1990. 4: 353-4
3. Baker CR, Sajjanshetty M, Baroni ML, Law N. Paintball injury causing temporal artery pseudoaneurysms – A case for better protection. Injury Extra. 2008. 39: 36-7
4. Bartholin T.editorsEpistolarium medicinalum centuria. The Hague: Comitum; 1644. p. 53-
5. Chen SS, Prasad SK. Traumatic pseudoaneurysm of superficial temporal artery: A case report. J Clin Ultrasound. 2009. 37: 312-4
6. Choo MJ, Yoo IS, Song HK. A traumatic pseudoaneurysm of the superficial temporal artery. Yonsei Med J. 1998. 39: 180-3
7. Hakan T, Ersahin M, Somay H, Aker F. Pseudoaneurysm of the superficial temporal artery following revision of a middle cerebral artery aneurysm clipping: Case report and review of the literature. Turk Neurosurg. 2011. 21: 430-4
8. Hong JT, Lee SW, Ihn YK, Son BC, Sung JH, Kim IS. Traumatic pseudoaneurysm of the superficial temporal artery treated by endovascular coil embolization. Surg Neurol. 2006. 66: 86-8
9. Kawai H, Hamasaki T, Imamura J, Tomonori N, Odashiro T, Yamahata H. Three cases of spontaneous superficial temporal artery aneurysm with literature review. Neurol Med Chir. 2014. 54: 854-60
10. Kim JH, Jung YJ, Chang CH. Superficial temporal artery pseudoaneurysm treated with manual compression alone. J Cerebrovasc Endovasc Neurosurg. 2015. 17: 49-53
11. Labropoulos N, Meisner RJ, Gasparis A, Tassiopoulos AK. Management of non-giant cell arteritis disease of the superficial temporal artery. J Vasc Surg. 2011. 53: 200-3
12. Lee HS, Jo KW, Lee SH, Eoh W. Traumatic pseudoaneurysm of the superficial temporal artery due to Gardner traction. J Korean Neurosurg Soc. 2010. 48: 291-3
13. Maheshwari R, Paterson AW. Pseudoaneurysm of the superficial temporal artery. Br J Oral Maxillofac Surg. 2009. 47: 412-3
14. Papavramidou N, Thomaidis V, Fiska A. The ancient surgical bloodletting method of arteriotomy. J Vasc Surg. 2011. 54: 1842-4
15. Pipinos II, Dossa CD, Reddy DJ. Superficial temporal artery aneurysms. J Vasc Surg. 1998. 27: 374-7
16. Roman AA, Arsenault AJ, Jackson KD, Price JM. Novel onset of a posttraumatic superficial temporal artery pseudoaneurysm. Case Rep Emerg Med 2013. 2013. 2013: 369309-
17. Sakamoto T, Sugimoto M, Kakigi A, Iwamura H, Kashio A, Suzuki M. A spontaneous true aneurysm of the superficial temporal artery treated by surgical resection. Auris Nasus Larynx. 2011. 38: 119-22
18. Sardana V, Sundar IV, Jaiswal M, Gupta P, Chopra S. Traumatic pseudoaneurysm of the superficial temporal artery: A case report and review of the literature. Indian J Neurotrauma. 2012. 9: 56-8
19. van Uden DJ, Truijers M, Schipper EE, Zeebregts CJ, Reijnen MM. Superficial temporal artery aneurysm: Diagnosis and treatment options. Head Neck. 2013. 35: 608-14
20. Walker MT, Liu BP, Salehi SA, Badve S, Batjer HH. Superficial temporal artery pseudoaneurysm: Diagnosis and preoperative planning with CT angiography. AJNR Am J Neuroradiol. 2003. 24: 147-50