- Department of Neurosurgery, Graduate School of Medicine and Pharmacological Science, University of Toyama, 2630 Sugitani, Toyama 930-0194, Japan
Correspondence Address:
Shusuke Yamamoto
Department of Neurosurgery, Graduate School of Medicine and Pharmacological Science, University of Toyama, 2630 Sugitani, Toyama 930-0194, Japan
DOI:10.4103/2152-7806.159377
Copyright: © 2015 Yamamoto S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Yamamoto S, Kashiwazaki D, Akioka N, Kuwayama N, Kuroda S. Superficial temporal artery to middle cerebral artery anastomosis for neovascular glaucoma due to common carotid artery occlusion. Surg Neurol Int 25-Jun-2015;6:
How to cite this URL: Yamamoto S, Kashiwazaki D, Akioka N, Kuwayama N, Kuroda S. Superficial temporal artery to middle cerebral artery anastomosis for neovascular glaucoma due to common carotid artery occlusion. Surg Neurol Int 25-Jun-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/superficial-temporal-artery-to-middle-cerebral-artery-anastomosis-for-neovascular-glaucoma-due-to-common-carotid-artery-occlusion/
Abstract
Background:Common carotid artery (CCA) occlusion sometimes requires surgical revascularization to resolve persistent cerebral/ocular ischemia. High-flow bypass is often indicated in these cases, using the interposed graft such as saphenous vein and radial artery. However, high-flow bypass surgery is invasive and may provide excessive blood flow to ischemic brain. In this report, we present a case that developed neovascular glaucoma due to CCA occlusion and was successfully treated with superficial temporal artery to middle cerebral artery (STA-MCA) anastomosis.
Case Description:A 61-year-old male complained of left visual disturbance and was admitted to our hospital. He underwent carotid endarterectomy for left internal carotid artery stenosis in previous hospital 1-year before, but he experienced left visual disturbance after surgery. Postoperative examinations revealed that the CCA was occluded. His visual disturbance gradually progressed, and he was diagnosed as neovascular glaucoma. None of ophthalmological therapy could improve his symptoms. Blood flow measurement showed an impaired reactivity to acetazolamide in the left cerebral hemisphere. Cerebral angiography demonstrated that the left STA was opacified through the muscular branches from the left deep cervical artery. Therefore, he successfully underwent left STA-MCA double anastomosis. His visual acuity improved and new blood vessels around the iris markedly decreased 3 months after surgery.
Conclusions:Precise radiological examination may enable standard STA-MCA anastomosis even in patients with CCA occlusion.
Keywords: Common carotid artery occlusion, neovascular glaucoma, superficial temporal artery to middle cerebral artery anastomosis
INTRODUCTION
Common carotid artery (CCA) occlusion is rare, but sometimes requires surgical revascularization to resolve persistent cerebral ischemia. In patients with CCA occlusion, however, high-flow bypass surgery is often indicated, because the superficial temporal artery (STA), one of the terminal branches of the external carotid artery (ECA), is not available as the donor graft. Usually, saphenous vein graft is used as an interposed graft in high-flow bypass for CCA occlusion.[
In this report, we present a case that developed neovascular glaucoma due to the ipsilateral CCA occlusion. By maximally utilizing the collateral circulation in the external carotid system, standard STA to middle cerebral artery (STA-MCA) double anastomosis could successfully be performed and dramatically improved glaucoma-related symptoms. Less invasive STA-MCA anastomosis may be indicated in a certain subgroup of patients with CCA occlusion, when the STA still keeps enough collateral circulation.
CASE REPORT
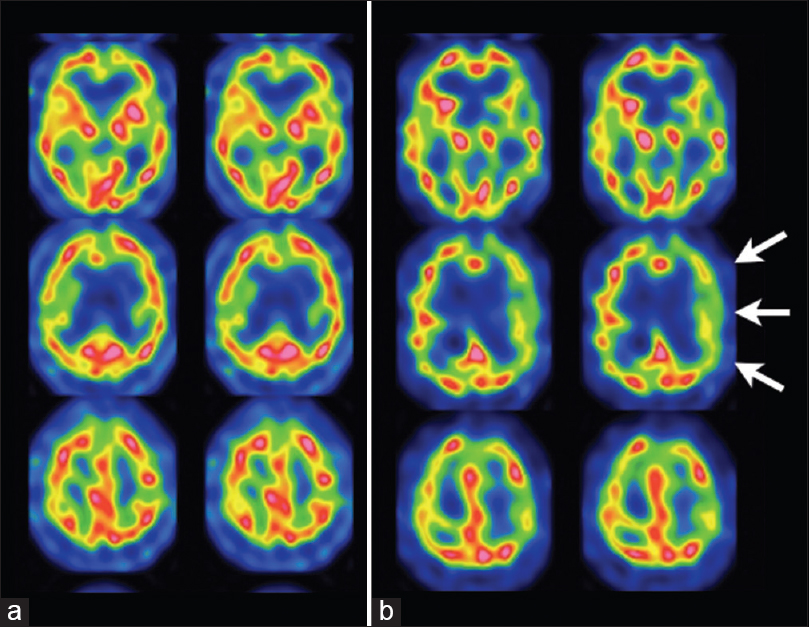
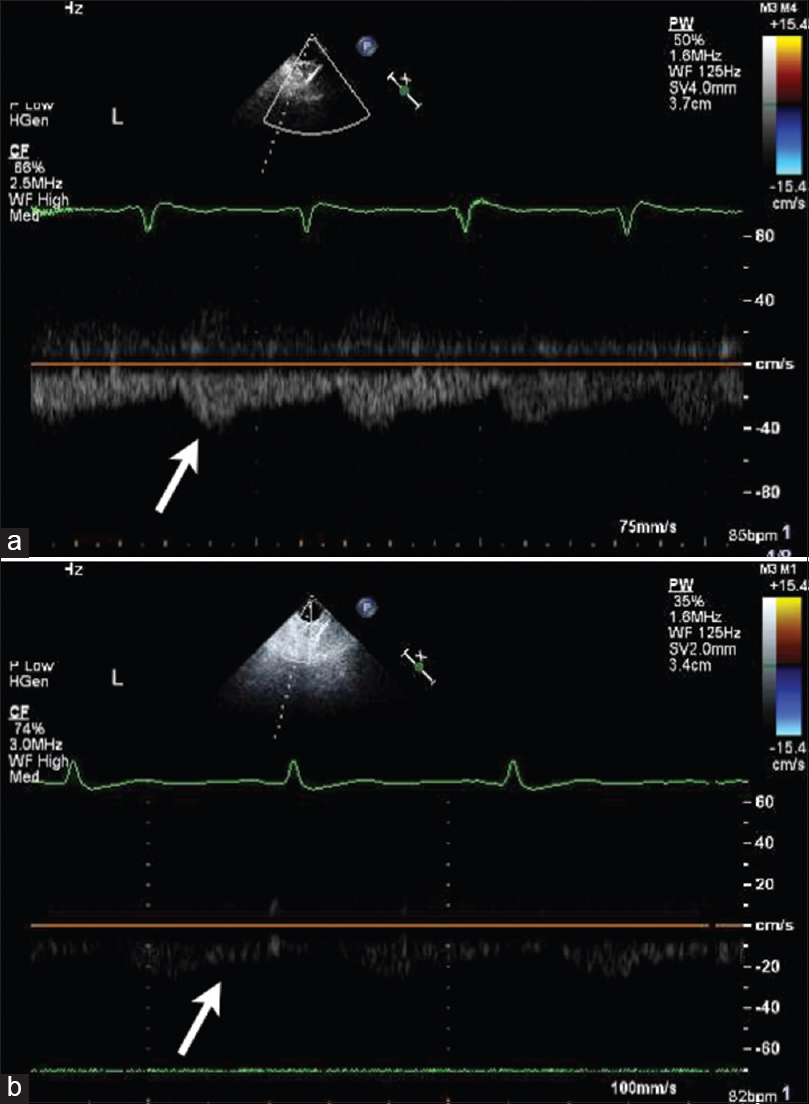
A 61-year-old male complained of left visual disturbance and was admitted to our hospital. He underwent carotid endarterectomy for left internal carotid artery (ICA) stenosis in previous hospital 1-year before, but he experienced left visual disturbance after surgery. Postoperative examinations revealed that the operated CCA was completely occluded. Additional surgery was not performed. His visual disturbance gradually progressed, and he was diagnosed as neovascular glaucoma. None of ophthalmological therapy could improve his symptoms. Neurological examination on admission revealed anisocoria. The size of pupils was 3.5 mm and 5.5 mm in the right and left side, respectively. Light reflex was absent in the left side. Left visual disturbance was severe (20/400 vision). Intraocular pressure was elevated up to 38 mmHg in the left side. No parenchymal lesion was observed on brain magnetic resonance (MR) imaging. However, MR angiography demonstrated that the left CCA and left vertebral artery were completely occluded. 123I-IMP single photon emission computed tomography (SPECT) showed an impaired reactivity to acetazolamide in the territory of the left ICA [
Figure 1
Preoperative single photon emission computed tomography findings of cerebral blood flow before (a) and after intravenous injection of acetazolamide. (b) Cerebral blood flow was kept within normal, but the reactivity to acetazolamide was impaired in the left middle cerebral artery territory (arrows)
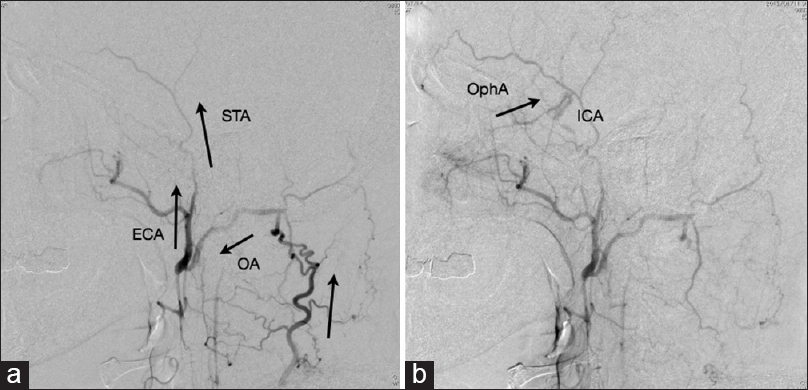
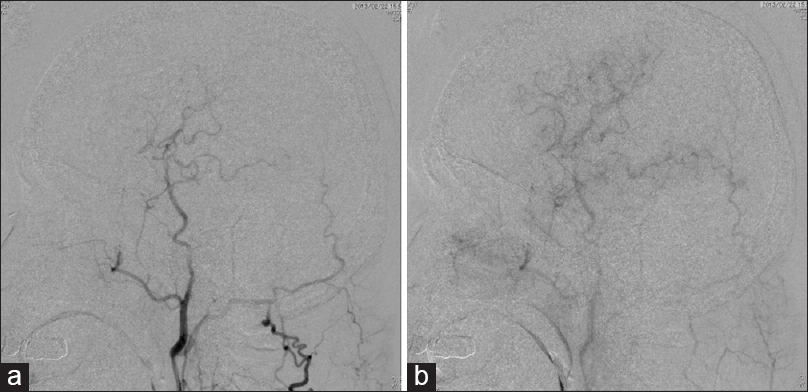
Figure 2
Preoperative cerebral angiography. (a) Early arterial phase of left subclavian angiogram. Lateral view: The occipital artery (OA) was opacified through the deep cervical artery. Then the retrograde blood flow of the OA opacified the main trunk of the external carotid artery and then superficial temporal artery. (b) Late arterial phase of left subclavian angiogram. Lateral view: Note that the internal carotid artery was opacified through the retrograde blood flow of the ophthalmic artery (OphA, arrow)
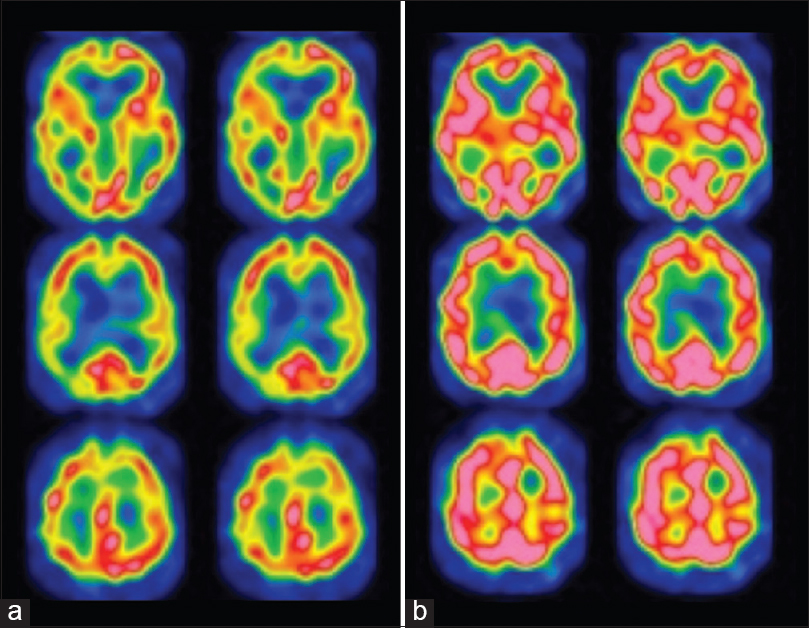
Based on these findings, he underwent left STA-MCA double anastomosis to resolve the reversed blood flow in the left ophthalmic artery and improve his glaucoma-related symptoms. The frontal and parietal branches of the STA were carefully dissected under a surgical microscope. We could confirm that the blood flow from the distal end of the ipsilateral STA had enough high-pressure during surgery. The branches of STA were anastomosed to the frontal and temporal branches of the MCA with an end-to-side fashion, respectively. The patency was confirmed during surgery, using indocyanine green videoangiography. Postoperative course was uneventful. Postoperative SPECT study performed 2 weeks after surgery demonstrated that the reactivity to acetazolamide completely recovered in the territory of the left MCA [
DISCUSSION
Common carotid artery occlusion is rarely recognized in 0.5–5% of total population, which is much less frequent than ICA occlusion.[
Riles et al. (1984) classified CCA occlusion into four types from surgical viewpoints.[
Common carotid artery occlusion does not always cause visual disturbance. However, the symptom is the only clinical sign in some patients with CCA occlusion.[
CONCLUSION
The authors present a case with neovascular glaucoma due to CCA occlusion. Extensive formation of collateral circulation enabled us to perform standard STA-MCA anastomosis safely and less invasively. Enough blood flow through bypass graft ceased the deterioration of visual acuity and resolve abnormal blood vessels around the iris. Less invasive STA-MCA anastomosis should be considered as one of the surgical options for the certain patients with CCA occlusion.
References
1. Archie JP Jr. Axillary-to-carotid artery bypass grafting for symptomatic severe common carotid artery occlusive disease. J Vasc Surg. 1999. 30: 1106-12
2. Aso K, Ogasawara K, Kobayashi M, Yoshida K. Arterial bypass surgery using a spontaneously formed “bonnet” superficial temporal artery in a patient with symptomatic common carotid artery occlusion: Case report. Neurosurgery. 2010. 67: onsE316-7
3. Collice M, D’Angelo V, Arena O. Surgical treatment of common carotid artery occlusion. Neurosurgery. 1983. 12: 515-24
4. Crocker M, Walsh D, Epaliyanage P, Tolias CM. Excimer laser-assisted non-occlusive cerebral vascular anastomosis (ELANA): Review of the first UK experience. Br J Neurosurg. 2010. 24: 148-55
5. Cull DL, Hansen JC, Taylor SM, Langan EM, Snyder BA, Coffey CB. Internal carotid artery patency following common carotid artery occlusion: Management of the asymptomatic patient. Ann Vasc Surg. 1999. 13: 73-6
6. Hashimoto Y, Kin S, Haraguchi K, Niwa J. Two symptomatic cases of common carotid artery occlusion. Jpn J Neurosurg. 2005. 14: 347-351
7. Kawaguchi S, Sakaki T, Kamada K, Iwanaga H, Nishikawa N. Effects of superficial temporal to middle cerebral artery bypass for ischaemic retinopathy due to internal carotid artery occlusion/stenosis. Acta Neurochir (Wien). 1994. 129: 166-70
8. Kawaguchi S, Sakaki T, Uranishi R, Ida Y. Effect of carotid endarterectomy on the ophthalmic artery. Acta Neurochir (Wien). 2002. 144: 427-32
9. Kazumata K, Asaoka K, Yokoyama Y, Sugiyama T, Kaneko S, Itamoto K. “Isolated carotid bifurcation” and vertebral-carotid artery bypass for common carotid artery occlusion. Neurol Med Chir (Tokyo). 2013. 53: 179-82
10. Kearns TP, Siekert RG, Sundt TM Jr. The ocular aspects of bypass surgery of the carotid artery. Mayo Clin Proc. 1979. 54: 3-11
11. Kobayashi T, Houkin K, Kuroda S, Saito H, Iwasaki Y. Internal carotid artery occlusive disease presected with visual disturbance: A retrospective study. Surg Cereb Stroke (JPN). 2002. 30: 15-8
12. Levine SR, Welch KM. Common carotid artery occlusion. Neurology. 1989. 39: 178-86
13. Martin RS, Edwards WH, Mulherin RS, Edwards WH. Surgical treatment of common carotid artery occlusion. Am J Surg. 1993. 165: 302-6
14. McGuiness CL, Short DH, Kerstein MD. Subclavian-external carotid bypass for symptomatic severe cerebral ischemia from common and internal carotid artery occlusion. Am J Surg. 1988. 155: 546-50
15. Melgar MA, Weinand ME. Thyrocervical trunk-external carotid artery bypass for positional cerebral ischemia due to common carotid artery occlusion. Report of three cases. Neurosurg Focus. 2003. 14: e7-
16. Nagasawa S, Tanaka H, Kawanishi M, Ohta T. Contralateral external carotid-to-external carotid artery (half-collar) saphenous vein graft for common carotid artery occlusion. Surg Neurol. 1996. 45: 138-41
17. Podore PC, Rob CG, DeWeese JA, Green RM. Chronic common carotid occlusion. Stroke. 1981. 12: 98-100
18. Riles TS, Imparato AM, Posner MP, Eikelboom BC. Common carotid occlusion. Assessment of the distal vessels. Ann Surg. 1984. 199: 363-6
19. Shibuya M, Suzuki Y, Takayasu M, Sugita K. Effects of STA-MCA anastomosis for ischaemic oculopathy due to occlusion of the internal carotid artery. Acta Neurochir (Wien). 1990. 103: 71-5
20. Sivalingam A, Brown GC, Magargal LE. The ocular ischemic syndrome. III. Visual prognosis and the effect of treatment. Int Ophthalmol. 1991. 15: 15-20
21. Spetzler RF, Rhodes RS, Roski RA, Likavec MJ. Subclavian to middle cerebral artery saphenous vein bypass graft. J Neurosurg. 1980. 53: 465-9
22. Spetzler RF, Roski RA, Rhodes RS, Modic MT. The “bonnet bypass”. Case report. J Neurosurg. 1980. 53: 707-9
23. Standefer M, Little JR, Tomsak R, Furlan AJ, Zegarra H, Williams G. Improvement in the retinal circulation after superficial temporal to middle cerebral artery bypass. Neurosurgery. 1985. 16: 525-9
24. Sullivan TM. Subclavian-carotid bypass to an “isolated” carotid bifurcation: A retrospective analysis. Ann Vasc Surg. 1996. 10: 283-9
25. Young LH, Appen RE. Ischemic oculopathy. A manifestation of carotid artery disease. Arch Neurol. 1981. 38: 358-6






Petr Galkin
Posted September 28, 2017, 9:13 am
Dear Shusuke Yamamoto!
Thank you for interesting clinical case.
On my opinion, in 1B CCA occlusion it is better to start with ECA bypass from proximal patent arterial trunks before STA-MCA anastomosis (for ex. subclavian artery) to provide enough (magistral) arterial flow in terminal branches of ECA.