- Department of Neurology, Medical College of Wisconsin, West Allis, WI 53227, USA
- Department of Neurosurgery, Springfield Neurological and Spine Institute, Springfield, MO 65804, USA
- Department of Neurosurgery, Medical College of Wisconsin, Froedtert Hospital, Milwaukee, WI 53226, USA
Correspondence Address:
Jack M. Leschke
Department of Neurosurgery, Medical College of Wisconsin, Froedtert Hospital, Milwaukee, WI 53226, USA
DOI:10.4103/2152-7806.173559
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Leschke JM, Mumert ML, Kurpad SN. Syringosubarachnoid shunting using a myringotomy tube. Surg Neurol Int 07-Jan-2016;7:
How to cite this URL: Leschke JM, Mumert ML, Kurpad SN. Syringosubarachnoid shunting using a myringotomy tube. Surg Neurol Int 07-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/syringosubarachnoid-shunting-using-a-myringotomy-tube/
Abstract
Background:Syringomyelia results from obstruction of cerebrospinal fluid (CSF) flow due to a multitude of causes. Often symptoms of pain, weakness, and sensory disturbance are progressive and require surgical treatment. We present here a rare technique for syringosubarachnoid shunting.
Case Description:We present the case of a 38-year-old male who suffered a traumatic cervical spinal cord injury due to a motor vehicle accident. With progressive pain and motor decline, a magnetic resonance imaging was obtained and showed a new syrinx extending cervical multiple segments. A unique surgical procedure using a myringotomy tube to shunt CSF into the subarachnoid space was employed in this case. The patient's examination stabilized postoperatively, and at 2 months and 6 months follow-up visits, his strength and sensation continued to improve.
Conclusion:We used a myringotomy tube for syringosubarachnoid shunting for the surgical management of a posttraumatic syrinx with good results. This technique minimizes suturing and may minimize shunt-related complications.
Keywords: Cerebrospinal fluid, shunt, spinal cord injury, syringomyelia, syrinx
BACKGROUND
Syringomyelia is caused by the pathologic obstruction of pulsatile cerebrospinal fluid (CSF) flow that occurs at any point caudal to the foramen magnum. The result is a fluid filled, gliosis lined cavity. The cavity itself can manifest as central canal dilation or can lie within spinal cord parenchyma.[
Clinically relevant syringomyelia will often present with intractable pain and central cord deficits that can be progressive.[
Surgery is the preferred treatment for syringomyelia regardless of the operative technique.[
Given the variability of clinical presentation, diverse pathophysiology, and provider preference, surgical treatment of syringomyelia is highly individualized. Historically, laminectomy, intradural exploration, lysis of adhesions, and duraplasty has been a favored option offering the most complete exposure.[
In the pediatric population, some have performed simple aspiration, and others have decompressed the posterior fossa to approximate normal CSF dynamics both with and without plugging of the obex.[
Shunting syrinx fluid to the subarachnoid space, peritoneal cavity, or pleural space using a fluid diversion catheter is a less invasive surgical alternative that has gained favor.[
Less invasive techniques such as endoscopic strategies and key-hole laminectomy with syringosubarachnoid shunt using a microscope boast limited removal of bone structures and ligamentum flavum. They argue preservation of normal anatomical structures and fewer complications.[
Unfortunately, in many patients, the benefits of surgery are not sustained, and repeat surgery is common due to cavity expansion and shunt failure–in particular with extraspinal shunts.[
In this study, we will describe a case in which we employed a rare technique for syringosubarachnoid shunting using a myringotomy tube in place of a flow diverting catheter. To our knowledge, only a single publication has reported a similar technique.[
CASE DESCRIPTION
A 38-year-old male was involved in an all-terrain vehicle crash and sustained a C6–C7 spinal cord injury with locked facets and underwent anterior/posterior cervical decompression and fusion. At the time of his initial injury, he had complete loss of motor function in his lower extremities as well as distal upper extremities. Strength was preserved in his biceps and deltoids, and a high thoracic sensory level was present.
Six months postinjury, the patient reported neck pain and loss of strength and sensation in the right arm for 3 weeks in duration. There was new right-sided weakness involving most notably his biceps and triceps muscles. Sensory function was diminished in the right arm with a C6 level on the left.
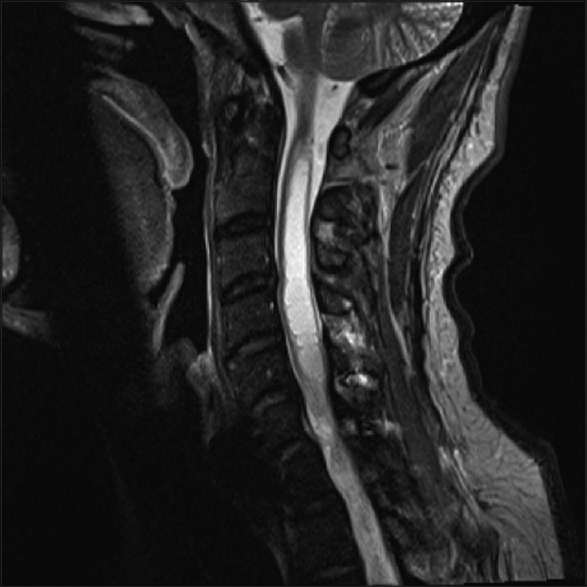
Magnetic resonance imaging of the cervical spine was performed and showed the appearance of a new large posttraumatic syrinx extending from C2 through the visualized upper thoracic spine [
Fluoroscopy was used to mark the planned incision site at the point where the syrinx was most prominent. Dissection was then carried down the midline to the inferior aspect of the targeted lamina. A small laminectomy was then performed, and the ligament was removed. The microscope was then brought into the operated field. Under high magnification, a midline durotomy was performed with the dura then tacked backward and retracted with 4-0 nylon sutures. With increasing magnification, we then identified an area of the spinal cord that was noted to be thinned out and white color and devoid of arteriovenous blood vessels. This was then opened with an 11 blade scalpel, and a gush of fluid suggested that the syrinx had been entered. A small spool-shaped myringotomy tube [
Postoperatively, the patient strength examination was stable compared to his preoperative exam. At 2 months and 6 months follow-up visits, his strength and sensation continued to improve progressively. Strength in his biceps, triceps, and wrists was full on the left with only small weakness comparatively on the right–which was much improved from his preoperative exam. Finger flexors had regained movement as well. At 1 year follow-up, symptoms were stable, and no imaging was indicated. He was instructed to follow-up as needed, and no repeat imaging was performed.
CONCLUSIONS
As we have described, various techniques are utilized for the surgical treatment of syringomyelia with varying success. No technique has demonstrated superior results when compared to the others; therefore, various shunting procedures such as syringoperitoneal, syringopleural, and syringosubarachnoid are practiced and can be used in different settings. In this study, we presented a rare technique for shunting CSF into the subarachnoid space using a myringotomy tube.
On review of literature, Ventureyra and Tekkök have reported the only other known report on a technique of this nature. Our technique broadly mirrors this one in terms of approach and concept. They report the use of a myringotomy tube through a small myelotomy for syrinx drainage without insertion of a catheter bulk into the syrinx. However, in contrast to our technique, the myringotomy tube used in their report employs perpendicular flanges that rest on the cord surface which are then secured to pia mater by 8-0 nylon sutures. At a mean follow-up of 11.5 months, 4/5 children (80%) had greater than or equal to a 30% decrease in maximum diameter of the syrinx.[
The advantage of using the spool-shaped myringotomy tube for shunting is that the hollow spool shape fixes the tube sturdily at the incision site. More importantly, without the perpendicular flanges, this shape avoids the need for suturing to the pial surface. We argue that this prevents a nidus for inflammation and resultant arachnoiditis, which may prove to offer higher success rates with further investigation.
In addition, as expected, the incision is small, and the surgeon will not have to tunnel a shunt catheter to a distant location. This allows for a significant degree of minimalism at and adjacent to the spinal cord itself, both periprocedurally and long-term.
One of the most important contributors to shunt malfunction is occlusion from arachnoiditis and adhesions around the catheter tip. We have mentioned that this is influenced by the integrity of the arachnoid membrane and the individual characteristics of the arachnoid space itself, ultimately determined by the underlying pathology. We suspect that our technique can further minimize scarring and prevent this feared complication. Furthermore, the use of the myringotomy tube by its nature avoids shunt-induced complications at distant body cavities.
The treatment of syringomyelia remains a difficult endeavor due to a multitude of factors. This study presents a rare technique that we have increasingly utilized with success and reliability. In the future, we plan to present our complete patient series.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abel R, Gerner HJ, Smit C, Meiners T. Residual deformity of the spinal canal in patients with traumatic paraplegia and secondary changes of the spinal cord. Spinal Cord. 1999. 37: 14-9
2. Barbaro NM, Wilson CB, Gutin PH, Edwards MS. Surgical treatment of syringomyelia.Favorable results with syringoperitoneal shunting. J Neurosurg. 1984. 61: 531-8
3. Batzdorf U, Klekamp J, Johnson JP. A critical appraisal of syrinx cavity shunting procedures. J Neurosurg. 1998. 89: 382-8
4. Batzdorf U. Primary spinal syringomyelia.Invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2005. J Neurosurg Spine. 2005. 3: 429-35
5. Batzdorf U. Primary spinal syringomyelia: A personal perspective. Neurosurg Focus. 2000. 8: E7-
6. Carroll AM, Brackenridge P. Post-traumatic syringomyelia: A review of the cases presenting in a regional spinal injuries unit in the North East of England over a 5-year period. Spine (Phila Pa 1976). 2005. 30: 1206-10
7. Gamache FW, Ducker TB. Syringomyelia: A neurological and surgical spectrum. J Spinal Disord. 1990. 3: 293-8
8. Gardner WJ, Angel J. The mechanism of syringomyelia and its surgical correction. Clin Neurosurg. 1958. 6: 131-40
9. Gezen F, Kahraman S, Ziyal IM, Canakçi Z, Bakir A. Application of syringosubarachnoid shunt through key-hole laminectomy.Technical note. Neurosurg Focus. 2000. 8: E10-
10. Guest JD, Silbert L, Casas CE. Use of percutaneous endoscopy to place syringopleural or cystoperitoneal cerebrospinal fluid shunts: Technical note. J Neurosurg Spine. 2005. 2: 498-504
11. Guigui P, Benoist M, Deburge A. Spinal deformity and instability after multilevel cervical laminectomy for spondylotic myelopathy. Spine (Phila Pa 1976). 1998. 23: 440-7
12. Hida K, Iwasaki Y, Koyanagi I, Sawamura Y, Abe H. Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery. 1995. 37: 673-8
13. Holly LT, Johnson JP, Masciopinto JE, Batzdorf U. Treatment of posttraumatic syringomyelia with extradural decompressive surgery. Neurosurg Focus. 2000. 8: E8-
14. Isu T, Sasaki H, Takamura H, Kobayashi N. Foramen magnum decompression with removal of the outer layer of the dura as treatment for syringomyelia occurring with Chiari I malformation. Neurosurgery. 1993. 33: 845-9
15. Kramer KM, Levine AM. Posttraumatic syringomyelia: A review of 21 cases. Clin Orthop Relat Res. 1997. 334: 190-9
16. Larner AJ, Muqit MM, Glickman S. Concurrent syrinx and inflammatory central nervous system disease detected by magnetic resonance imaging: An illustrative case and review of the literature. Medicine (Baltimore). 2002. 81: 41-50
17. Laxton AW, Perrin RG. Cordectomy for the treatment of posttraumatic syringomyelia.Report of four cases and review of the literature. J Neurosurg Spine. 2006. 4: 174-8
18. Lee TT, Alameda GJ, Camilo E, Green BA. Surgical treatment of post-traumatic myelopathy associated with syringomyelia. Spine (Phila Pa 1976). 2001. 26: S119-27
19. Milhorat TH. Classification of syringomyelia. Neurosurg Focus. 2000. 8: E1-
20. Padovani R, Cavallo M, Gaist G. Surgical treatment of syringomyelia: Favorable results with syringosubarachnoid shunting. Surg Neurol. 1989. 32: 173-80
21. Perrouin-Verbe B, Lenne-Aurier K, Robert R, Auffray-Calvier E, Richard I, Mauduyt de la Grève I. Post-traumatic syringomyelia and post-traumatic spinal canal stenosis: A direct relationship: Review of 75 patients with a spinal cord injury. Spinal Cord. 1998. 36: 137-43
22. Samii M, Klekamp J. Surgical results of 100 intramedullary tumors in relation to accompanying syringomyelia. Neurosurgery. 1994. 35: 865-73
23. Schurch B, Wichmann W, Rossier AB. Post-traumatic syringomyelia (cystic myelopathy): A prospective study of 449 patients with spinal cord injury. J Neurol Neurosurg Psychiatry. 1996. 60: 61-7
24. Sgouros S, Williams B. Management and outcome of posttraumatic syringomyelia. J Neurosurg. 1996. 85: 197-205
25. Suzuki M, Davis C, Symon L, Gentili F. Syringoperitoneal shunt for treatment of cord cavitation. J Neurol Neurosurg Psychiatry. 1985. 48: 620-7
26. Tator CH, Meguro K, Rowed DW. Favorable results with syringosubarachnoid shunts for treatment of syringomyelia. J Neurosurg. 1982. 56: 517-23
27. Todor DR, Mu HT, Milhorat TH. Pain and syringomyelia: A review. Neurosurg Focus. 2000. 8: E11-
28. Vannemreddy SS, Rowed DW, Bharatwal N. Posttraumatic syringomyelia: Predisposing factors. Br J Neurosurg. 2002. 16: 276-83
29. Vaquero J, Martínez R, Arias A. Syringomyelia-Chiari complex: Magnetic resonance imaging and clinical evaluation of surgical treatment. J Neurosurg. 1990. 73: 64-8
30. Ventureyra EC, Tekkök IH. Syringostomy using myringostomy tube: Technical note. Neurosurgery. 1997. 41: 495-7
31. Williams B, Page N. Surgical treatment of syringomyelia with syringopleural shunting. Br J Neurosurg. 1987. 1: 63-80
32. Won DJ, Siddiqi J, Yamada S. A novel, simplified pediatric syringopleural shunt.Technical note. J Neurosurg. 2005. 102: 123-6
33. Yasuoka S, Peterson HA, MacCarty CS. Incidence of spinal column deformity after multilevel laminectomy in children and adults. J Neurosurg. 1982. 57: 441-5