- Department of Neurological Surgery, Loyola University Medical Center, Maywood, Illinois, USA
Correspondence Address:
O. Howard Reichman
Department of Neurological Surgery, Loyola University Medical Center, Maywood, Illinois, USA
DOI:10.4103/2152-7806.156635
Copyright: © 2015 Reichman OH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Reichman OH. The Dumbest Mistake I Ever Made. Surg Neurol Int 14-May-2015;6:78
How to cite this URL: Reichman OH. The Dumbest Mistake I Ever Made. Surg Neurol Int 14-May-2015;6:78. Available from: http://surgicalneurologyint.com/surgicalint_articles/dumbest-mistake-ever-made/
Abstract
Life as a Neurological Surgeon is a foreboding responsibility and a gratifying opportunity. Having the confidence and trust of individuals faced with a life or death situation requires extensive training and experience. Curiosity provides the motivation to continuously seek better understanding of complex disease problems, better technology, improved diagnostic capability, and surgical skills. Solution of these challenges has been a constant process for several decades and continues to pose opportunities for progress. Early observation of results provides important information, but in many circumstances it may require long-term evaluation to fully document the benefit, or lack of benefit, for any treatment procedure. The focus of attention by the Neurological Surgeon must be on the proper immediate management of each given situation, but it is also important, and a responsibility to consider the long-term consequences or results. This presents a difficult challenge because patients move into distant places and Neurological Surgeons frequently move to accept new opportunities. It is expensive and cumbersome to retain records for many years. It is also unpredictable which patient's information will become particularly significant. It is an opportunity to describe experience with four patients to illustrate this dilemma.
Keywords: Arteri ovenous malformation, curiosity, cervical intramedullary ependymoma, hydrocephalus, hereditary hemorrhagic telangiectasia, long-term follow-up, microneurosurgery, treasure trove
Having enjoyed the opportunity to experience more than eight decades of life, I feel extremely grateful for the many enormous opportunities to directly participate in numerous unexpected advances.
Following the Great Depression (1928-1933), World War II (1941-1945), and the Korean War (1959-1953), an enormous environment of patriotism surrounded the United States. The price for World War II was reported as the loss of 405,399 brave American Military Servicemen and for the Korean War 54,246 lives. During his Inaugural Address (January 20, 1961) President John F. Kennedy expressed “Ask not what your country can do for you - ask what you can do for your country.” This attitude led to the Space Program and on July 21, 1969 when Astronaut Neil Armstrong stepped on the moon and said “That's one small step for man, one giant leap for mankind.”
This same attitude also spread throughout the medical profession with many physicians motivated by “curiosity” the word expressed by Astronaut Eugene Cernan during an Interview on television. This attitude was clearly illustrated by the life of Thomas E. Starzl, M.D. He had Joined the Navy in March 1944 and served until the war ended. He then graduated from Westminster College of Fulton, Missouri in May 1947 and attended Northwestern University Medical School (1947-1952). His subsequent medical training led to his arrival in December 1951 at the University of Colorado to become Chief of Surgery at the Denver VA Hospital and for the purpose of developing an Organ Transplant Program. His offices were on the fourth floor of the VA Hospital adjacent to the operating room and recovery room. During my third year of training in Neurological Surgery (July 1962 to June 1963) it became my opportunity to become quite well acquainted with Dr. Starzl and since the donor for first technically successful liver transplant was an individual approaching death because of an intracranial glioblastoma (his survival to this point had been several years and I confirmed the diagnosis by reviewing the pathology with our Neuropathologist). I was in attendance and clearly remember the operation performed on May 5, 1953. The patient was clearly alert and doing very well the next day, but unfortunately, died suddenly because of rejection 22 days later.
Three patients were operated (June, July, and October) with the same result, hence the program was delayed for 3 years to evaluate prednisone, imuran, cyclosporin, and other considerations for prevention of the rejection problem. Dr. Starzl work tirelessly and with determination to solve all of the issues concerning organ transplantation until after his retirement in 1990 following coronary bypass surgery.
During the fall of 1954 the first clinical rotation of my third year at the University of Utah College of Medicine was on Pediatrics. My first patient was a child diagnosed as “Failure to Thrive.” At 4-6 weeks, he weighed less than at birth. He was found to have a coarctation of the aorta. Doctors William Ray Rumel and Thomas F. Keyes performed surgery to remove the coarctation. This was the youngest and smallest patient to undergo this procedure in the State of Utah.
Following surgery, he immediately gained weight, became more alert, and made rapid progress. The experience of observing surgery and seeing his remarkable progress had a profound effect upon my future career. I felt that my aptitude matched the skills required for this type of surgery and that the satisfaction derived from this type of service would exceed any other experience for me.
During the following summer it became my opportunity to serve as an Extern at the L. D. S. Hospital in Salt Lake City. This provided an opportunity for experiences with several surgical specialties, but my greatest interest was to become better acquainted with Dr. Rumel and Robert J. Beveridge, who were then completing his Fellowship.
Coincidentally, we learned that the Beveridges lived in housing near ours and this established life-long friendship. Dr. Beveridge was born in Denver and graduated from the University of Colorado with B.A. and M.D. degrees. This later had a big influence on my later decision to move to Denver for training with Dr. Henry Swan and Dr. Robert Vertue.
As I approached graduation from medical school, I thought about several friends who had joined the reserves in military service and when activated, entered at a higher rank than as a “buck private” and enjoyed a very beneficial experience. I then joined the army reserve and rose from First Lieutenant to Major and also enjoyed a very beneficial experience.
Because of my experience as an Extern at L. D. S. Hospital, I had become acquainted with many of the attending physicians and rotations on Surgery, Internal Medicine, Pediatrics, OB-GYN, and Orthopedics.
While a career in Pathology was never a serious plan, my good friend, pathologist Homer H. Clark, M.D., suggested that active duty with only one year of surgery would likely be less beneficial than a year of pathology and he helped arrange for me to spend a year with his former director, J. Arnold deVeer, M.D. at the Brooklyn Hospital. This proved a very beneficial opportunity in many ways, but particularly since the President of the New York Heart Association was on the staff and assisted me in the acquisition of a New York Heart Association Fellowship to Nork with Ralph Deterling, M.D. at Columbia-Presbyterian Medical Center in New York City. This experience was presented before the New York Heart Association, May 18, 1959.
Because of my familiarity with staff and procedures at L. D. S. Hospital in Salt Lake City, I decided to return for my first year of Residency in General Surgery. Once again it was a very beneficial experience to associate with the Cardi othoracic Surgeons, but in retrospect, the most significant experience proved to be in Neurological Surgery with J. Louis Schricker, M.D. when I became aware and involved with the wide variety of conditions in this specialty, although my goal remained in cardiac surgery.
It became my good fortune to fill a vacancy as Second Year in General Surgery at the University of Colorado in Denver. Interestingly, my First rotation was in Neurological Surgery at Denver General Hospital. By then I had already had considerable experience with Neurological Surgery and throughout the year frequently interacted with the staff of Dr. Keasley Welch. It then became necessary to make the most difficult, but best professional decision of my life, to change course and pursue a career in Neurological Surgery.
At that time, preparation for surgical treatment of intracranial aneurysm consisted of 5:00 AM induction of anesthesia, immersion into a tub of ice water (to lower body temperature to 28-30°C), and bilateral exposure in the neck by vascular surgeons of external and internal carotid and vertebral arteries. The patient was then positioned and prepared for craniotomy to expose and clip the aneurysm.
Tragically, a brilliant and talented 60-year-old friend and neighbor completed her usual day when she suddenly collapsed and was pronounced dead 48 h later (September 26, 1961) because of hemorrhage from an intracranial aneurysm.
The annual meeting of the Congress of Neurological Surgery was conducted (October 11–13, 1961) in New York City. It became my opportunity to attend and, interestingly, subarachnoid hemorrhage and intracranial aneurysm were major topics of discussion. I remember interesting remarks by Hendrik Julius Svien, M.D.
Dr. Welch had a keen interest in the physiology of cerebrospinal fluid and clarified the anatomy and physiology of arachnoid villi as valves (Surgical Forum 10:767-769, 1960).
He also studied the secretion of cerebrospinal fluid by choroid plexus of the rabbit (Am. J. Physiol 205:617-624, 1963). It was my opportunity to participate in this study and the methods were later applied to evaluate flow through the EC-IC Bypass Graft (Fein and Reichman: Microvascular Anastomosis for Cerebral Ischemia. Springer-Verlag: P 220-240, 1974).
The University of Colorado had an excellent and very active Department of Pediatrics under the outstanding leadership of C. Henry Kempe, M.D. We were frequently consulted because of an infant with an enlarging head and a large and tense anterior fontanel. A need le was inserted for removal of a small amount of cerebrospinal fluid, insertion of a small amount of air, and X-ray ventriculogram. Treatment with the relatively new Holter valve or Pudenz valve usually provided a satisfactory result. Unfortunately, the large fontanel was occasionally the result of bilateral subdural hematomas, which required bilateral craniotomies for removal of the mass of blood with the surrounding membranes. Fractures of extremity bones were frequent and confirmed abuse. This resulted in the landmark review “The Battered -Child Syndrome” JAMA 181:17-24, 1962. We were also frequently consulted for infants with craniosynostosis, which required linear craniectomy for restoration of normal configuration of the head.
One morning I, a nonartist, was sent on an errand to locate in the city of Denver an artist's air brush. I had no idea what an artist's air brush was, let alone, where to find one. During surgery for an anterior communicating artery aneurysm, Dr. Welch had concluded that the arterial branches were so complex that the usual clipping would pose an excessive risk and the operative exposure was closed. He then contacted Dr. Bertram Selverstone of Boston who provided some polyvinal-polyvinylidene chloride latex and epoxy-polyamide resin for re-exposing and re-enforcing the aneurysm (Clinical Neurosurgery 9:201-213, 1963).
Since Richard A. Lende was experienced and particularly interested in cerebral physiology and localization, he initiated the program for stereotaxic treatment of patients with movement disorders. The stereotaxic apparatus designed by Professor Lars Leksell of the Karolinska Institute in Stockholm, Sweden was acquired.
Upon completion of my training in Neurological Surgery at the University of Colorado (June 30, 1964), I returned to Salt Lake City, Utah for establishment of my practice of Neurological Surgery. It became my opportunity to become deeply involved in the new Birth Defects Program sponsored by the March of Dimes and directed by Garth Myers, M.D. at Primary Children's Hospital. I acquired a Leksell system which was placed at Holy Cross Hospital and a Todd -Wells system, which was placed at L. D. S. Hospital for the treatment of movement disorders. My preliminary results were presented in September 11, 1968 at the annual meeting of the Utah State Medical Society. This led to a visit with George Constantin Cotzias at Brookhaven National Laboratory and the acquisition of an enormous amount of L-DOPA. A presentation before the Utah Medical Association on September 11, 1970 summarized the experience with the first 75 of 100 patients utilizing this new treatment.
At that time there existed more of an atmosphere of cooperation and collaboration rather than competition. It was a common practice to visit other neurological surgeons and learn from individuals with different experiences. A symposium on Microneurosurgery was held April 14-15, 1967 at the University of California in Los Angeles.
The annual meeting of the American Association of Neurological Surgeons followed in San Francisco April 17-20, 1967 when it was possible to purchase a Zeiss binocular surgical microscope for preliminary experience in the research laboratory. Clifford C. Sny der, M.D. joined the faculty at the University of Utah September 1, 1967 to found the Division of Plastic and Reconstructive Surgery. He also became the Chief of Surgery at the VA Hospital and developed a research laboratory. This provided the opportunity for me to develop skills in microsurgery, including canine lingual-basilar anastomosis.
Leonard I. Malis, M.D. sponsored a course entitled Microneurosurgery (June 15-19, 1970) at the Mount Sinai school of Medicine in New York City. At this time I learned how to properly use the Malis bipolar coagulator by approximating the tips of the forceps under saline solution. During this meeting, I had the opportunity to develop a friend ship with Dr. M. Gazi Yasargil after he described his early experience with removal of spinal cord arteriovenous malformations and aneurysm surgery. Dr. Yasargil invited me to visit him in Zurich, Switzerland. During the next 2 weeks it was a great opportunity to observe Dr. Yasargil perform a variety of microsurgical operations, including his 16 patient for anastomosis between the superficial temporal artery and a cortical branch of the midd le cerebral artery.
I greatly appreciate the word “curiosity” as mentioned by Astronaut Eugene Cernan. This has been the motivation for many of us in Neurological Surgery to increase our understanding of many serious disease problems and to increase equipment and surgical methods for more satisfactory results.
In retrospect, I enjoyed a remarkable opportunity to serve as Neurological Surgeon in Salt Lake City between 1964 and 1973 when I moved to Loyola University Medical Center in the Chicagoland area for practice until 1997.
During the years at Loyola, I kept all the medical records from my practice in Salt Lake City. Since they had never been used during this time, they were shredded before moving back to Utah. This was “The Dumbest Mistake I Ever Made”. A treasure-trove of information was lost! It is very expensive and difficult to retain all records for a long time, but it is not possible to predict which cases will provide information because of long-term follow-up. Fortunately, I have sufficient information from four patients to illustrate the value of long-term follow-up.
CASE I
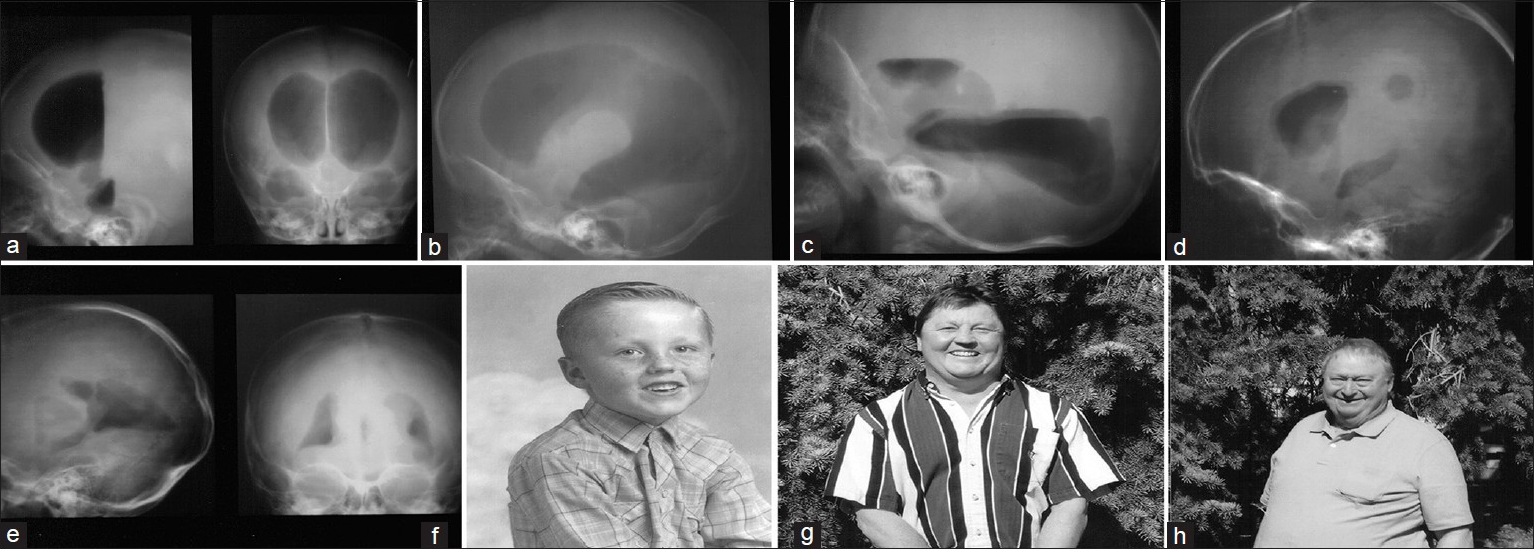
This 50-year-old male was born January 3, 1964 at Rock Springs, Wyoming. At age 6 months he was noted to have an enlarging head. He was referred to the Birth Defects Program (sponsored by the National Foundation March of Dimes) at Primary Children's Hospital in Salt Lake City, Utah. A ventriculogram demonstrated severe hydrocephalus with obstruction of the Acqueduct of Sylvius and no fluid beyond [Figure
Figure 1
(a) Initial ventriculogram with patient in supine position. Air demonstrates large lateral venticles. Left: lateral view. Right: frontal view. (b) Patient in lateral position demonstrates very large lateral ventricle. (c) Patient in prone position demonstrates large third ventricle with posterior filling of large lateral ventricle, but no filling of aqued uct or fourth ventricle. (d) Ventriculogram performed May 22, 1969. Patient in supine position shows normalization of lateral ventricle size. (e) Ventriculogram performed May 22, 1969. Patient in prone position shows normalization of lateral ventricle size. The third ventricle is normal in size, but there is no filling of the aqueduct or fourth ventricle. (f) Patient at age 5 years. (g) Patient at age 48 years adjacent to his office. (h) Neurological Surgeon O. Howard Reichman, M.D., adjacent to patient's office March 22, 2012
Because of the distance involved and my intense new responsibilities, I lost contact with patients from my practice in Salt Lake City. Therefore, I had no insight into the subsequent life of this person. Fortunately, it became a wonderful opportunity to re-establish contact and meet him in his office at Laramie, Wyoming on March 22, 2012 [Figure
In his community there was no kindergarten, so he began first grade in 1970 at age 6. Because of his father's interest in the sport of boxing, he also became interested and began at age 12 to participate in the sport under his father's direction and later under the instruction of other highly skilled and professional leaders. He attended Mountain View High School (south of Fort Bridger) and graduated in 1982. He then entered the United States Army and was very active on the military boxing team. While stationed at a base in Germany, he went with the group to Finland for a special event in preparation to participate with the 1984 Olympics in Los Angeles. Tragically, the bus attempted to pass under a low bridge and the roof of the bus was torn off. He sustained several injuries and was in coma for several hours. He was taken to a hospital and a ventriculo-peritoneal shunt was inserted. He experienced no further problems with hydrocephalus, but was d ischarged from the army in 1984.
After discharge from the army, he returned to Rock Springs and became employed in hard hat’’ construction projects. He was married on April 15, 1985 and has become the father of three wonderful and accomplished children.
Approximately 7 years after discharge from the army, he decided to consider college and with some financial assistance resulting from his prior military service, attended Western Wyoming Community College at Rock Springs (1991-1993). He then entered the College of Business at the University of Wyoming in Laramie, graduating in 1995. He has since been employed as a Benefit Specialist at the Family Services Center in Laramie, Wyoming. This has been, and continues to be, an enjoyable and rewarding opportunity.
His parents retired in the community of Pahrump, Nevada and have greatly enjoyed this location. On April 13, 2012 the patient and his father were enjoying golf when he suddenly passed-out and was taken to a hospital at Las Vegas where a shunt revision was performed and he continues to do very well as he expressed during a telephone conversation with me on September 18, 2014.
CASE II
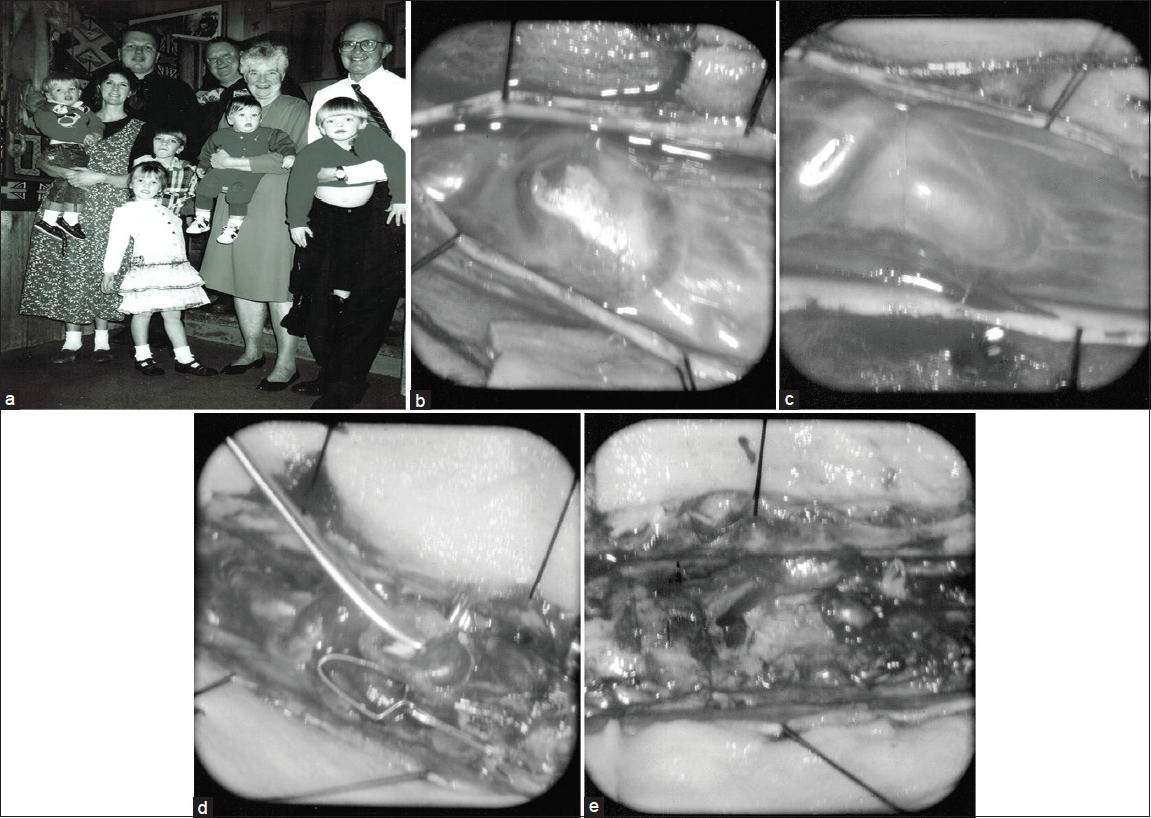
This charming 52-year-old female continues to enjoy a very enthusiastic, active, and productive life. She has become the mother of five wonderful children [
Figure 2
(a) The patient's family (February 3, 1996). Back row (left to right): patient’ s husband, neurological surgeon (OHR). Middle row (left to right): patient with child, patient's mother with child, patient’ s father with child. Front row: two older children standing. (b) View through surgical microscope (July 20, 1970). Large tense aneurysm at T-1. (c) View through surgical microscope (July 20, 1970). Large tense draining vein at T-2. (d) View through surgical microscope (July 22, 1970). Large aneurysm still rather tense. (e) View through surgical microscope (July 22, 1970). Total removal of spinal arteriovenous malformation has been accomplished
At age 3, she had a minor head injury that caused unconsciousness for nearly a week and was associated with nuchal rigidity and blood y cerebrospinal fluid. At age 4, she developed low back pain. As she approached her 8th birthday, she began limping on her left foot with increasing weakness of the leg and inversion deformity. Examination demonstrated weakness of hip flexion (left greater than right) with weakness of left hip extension and paralysis of dorsiflexion and eversion of her left foot. A myelogram demonstrated a large serpiginous filling defect between T-1 2 and L-4. An aortogram demonstrated a very large and complex arteriovenous malformation between T-9 and L-4.
Because of her rapidly threatening situation, the possibility of surgical removal raised many questions. After extensive thought and numerous discussions, it was decided to proceed with surgery. On July 20, 1970, a laminectomy was performed extending from T-9 to L-3. An enormous number of sepentine vessels were coagulated and removed. However, a large aneurysm [
While attending Union High School at Roosevelt, Utah she became actively involved in the Drill Team, which required very active dance steps. A problem with elevation of the left foot created a challenge for her, but she was able to compensate for this sufficiently that others were unaware and the team won First Place in the State Competition.
After graduation from high school she attended R icks College at Rexburg, Idaho for 2 years. She then completed a mission at Quito, Ecuador (October 1984 to March 1986) for the Church of Jesus Christ of Latter-day Saints. She was married on August 8, 1986. Her husband had completed a mission to Pittsburgh, Pennsylvania. They have become parents of five outstanding children [
The patient's father had suffered nosebleed s for many years for which numerous procedures were performed without much relief. He had also observed dark stools on occasion. He finally underwent the procedure of Nasal Cavity Closure, which provided much relief. This made it possible for him to serve in the Temple Presidency of the Montcello, Utah Temple for the Church of Jesus Christ of Latter-day Saints and to fulfill missions in Downers Grove, Illinois and Bangkok, Thailand.
The father had become aware that he had suffered from a rare familial problem, but at the time very little was known of this disease. His mother had experienced severe difficulties, but lived to the age of 72 years. His grandfather had also experienced difficulties, but lived to the age of 80 years and his death certificate listed hypertensive card iovascular renal disease and atherosclerosis.
The patient's father became aware that progress was becoming available in understanding the genetics of this problem and in 1989 he became one of the Board of Directors of the hereditary hemorrhagic telangiectasia (HHT) Foundation, Inc. that was being established. He also became acquainted with Jamie McDonald, M.S., LGC who also became a member of the Board of Directors and established the HHT Clinic at the University of Utah Medical Center in 1995.
Of interest, the great-grandfather of the patient's father was a member of the Willia West Lane Company of the Mormon Overland Travel Company to Salt Lake City in 1852 and traveled with his wife and his older brother. He later had a total of four wives and descendents of three of these were later proven to have HHT, proving that he carried the genetic abnormality. He became the first Mayor of Springville, Utah, but died of pneumonia at age 77. None of his brother's descendents have demonstrated any evidence of HHT.
Illustration of the patients family was performed February 3, 1996 at the Sundance Resort in Provo Canyon prior to her participation on February 7, 1996 during the 22nd Annual Richard Lende Conference at Snowbird Utah. This preceded the Fifth Annual Conference of the International Hereditary Hemorrhagic Foundation, Inc. in Salt Lake City, Utah (July 19–21, 1996). During this meeting was discussed that Chromosome 9 and Chromosome 12 contain the genetic abnormalities causing HHT.
Genetic mutations have since been clearly documented so that genetic testing is now widely available. Doctor Jamie McDonald has greatly contributed to this research and has published very informative guidelines to increase our understanding. Depending upon the size and location of the telangiectasia and the age of a patient, HHT may present with a wide range of manifestations. Some are relatively minor and rather insignificant. Some are annoying to a variable degree. Others are potentially very serious and even fatal!
With all the progress that has, and is currently being made, I have become amazed and concerned in talking to several experienced medical colleagues by how little is generally known regarding HHT. It has become my wonderful opportunity to become better informed by my patient, her family, and particularly by Jamie McDonald, M.S., LGC.
CASE III
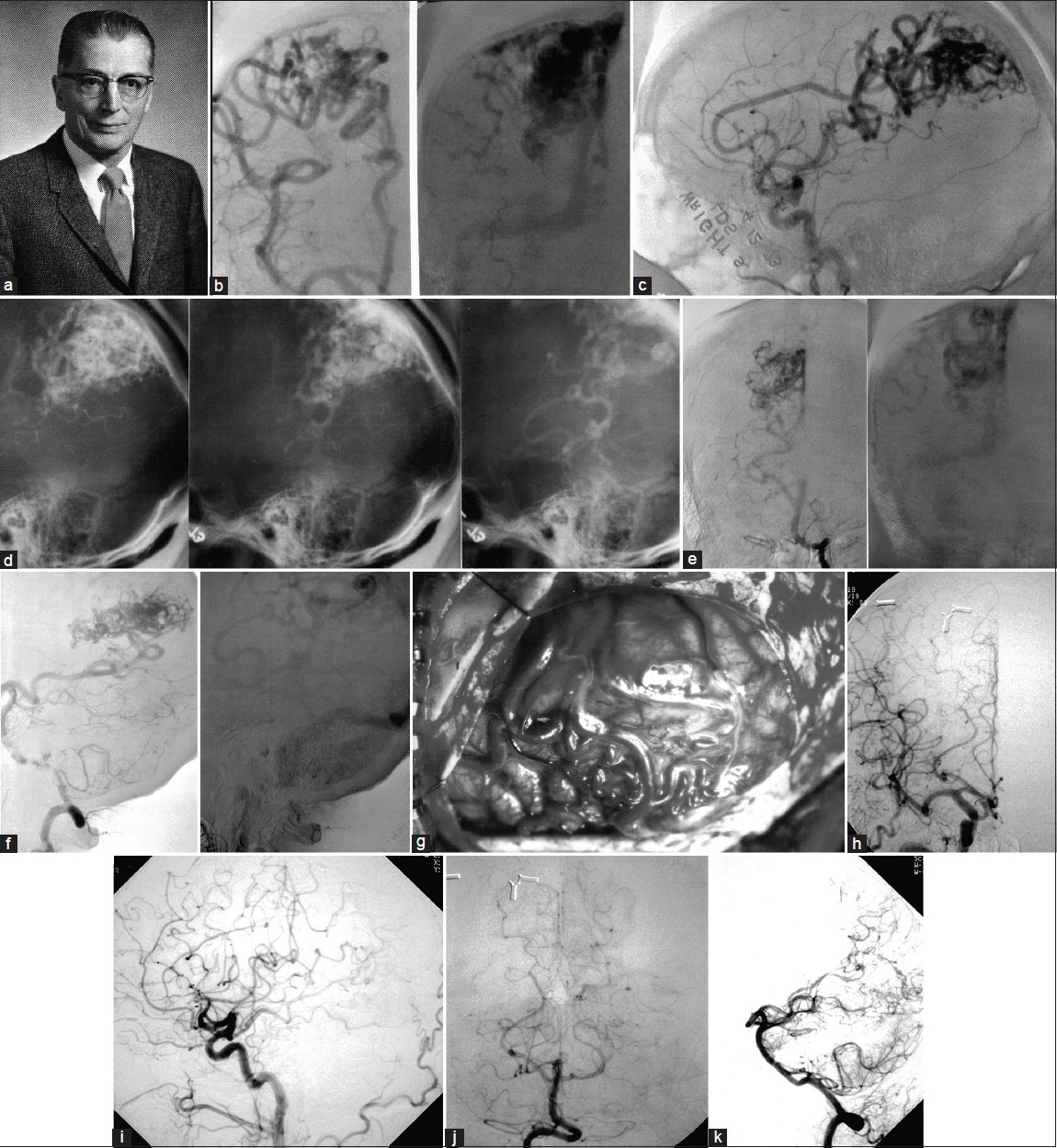
This 68-year-old male was showering while at junior high school (age 11 years), when suddenly everything went blank and he passed-out. He awakened while the school principal was driving him home. Later that year he experienced another episode and his father contacted his uncle Stewart A. Wright, M.D. [
Figure 3
(a) Stewart A. Wright, M.D., Neurological Surgeon. (b. April 13, 1973. Right carotid arteriogram. Left: Early arterial phase demonstrates very large middle and anterior cerebral branches with early filling of arteriovenous malformation (AVM). Right: Later phase demonstrates large AVM with early venous drainage. (c) Lateral view demonstrates early filling of right posterior parietal AVM. (d) Three stages of lateral view of the enormous right posterior parietal AVM. (e) Frontal view of left vertebral injection. Left: Early filling of AVM from right posterior cerebral artery. Right: Later phase demonstrates early filling of AVM with early venous drainage. (f) Lateral view of left vertebral injection. Left: Left vertebral artery fills right posterior cerebral artery leading to AVM. Right: Later phase demonstrates venous drainage of AVM. (g) Operative exposure demonstrates surface visualization of AVM extending to midline into sagittal sinus. (h) May 22, 1998. Right carotid arteriogram demonstrates return of middle and anterior cerebral arteries to normal size with no evidence of residual AVM. Metal clips remain from original operation. (i) Lateral view of right carotid arteriogram demonstrates no evidence of original AVM. (j) Frontal view of left vertebral injection shows normal filling of basilar and both posterior cerebral arteries with no evidence of original AVM. Metal clips remain from original operation. (k) Lateral view of left vertebral arteriogram demonstrates normal intracranial filling and no evidence of original AVM
In April, 1973 he developed severe headache and passed-out. He was ad mitted to the hospital where he awakened. He had slight nuchal rigidity, but his neurological examination was otherwise basically normal. A spinal tap demonstrated xanthchromic fluid with a pressure of 370 mm, 177 RBC, and 49 mg protein. An arteriogram performed on April 13, 1973 demonstrated a huge arteriovenous malformation located in the right occipital region [Figure
Considering all of the complex circumstances involved, it was decided to proceed with surgery on April 19, 1973 [
The asymptomatic patient married an outstanding wife on May 2, 1974 and together they have become the parents of seven very talented and accomplished, now adult, children.
Unfortunately, the patient immediately became acquainted with the employment challenges resulting from complex intracranial surgery and treatment with Dilan tin. His first employment as Medical Assistant for the Utah Medical Examiner was terminated after only 6 months. While I know nothing of the detailed issues, the result seems highly inappropriate.
He became a Purchasing Agent for the United States Federal Government (1984-1999) and this became a very reliable financial support for him and his family. He was at Hill Field Air Force Base (1984-1987), then at Dugway Proving Ground (1987-1999). He was at Dugway when the arteriogram was performed in Provo, Utah on May 22, 1998.
It became my (OHR) opportunity to meet again with this individual on July 13 and 19, 2011 and again on April 25, 2012. I was deeply impressed by his energy, superb memory, and obvious intellectual capability. He has also developed a reputation among friends and other employees of integrity, dependability, cooperation, and diligence. While he continues to receive some benefits resulting from government employment (1984-1999), a change in government priorities led to his retirement from the position last held. I feel deeply disturbed by the difficulties he has since experienced in his effort to obtain reliable employment because of his age and history of major intracranial surgery with continued anticonvulsant medication. He did have a brief episode of transient amnesia for which he was taken to the Emergency Department of the Intermountain Medical Center (November 21, 2007), but an extensive evaluation did not demonstrate any major problem and his memory returned promptly. He was discharged with arrangements made for follow-up evaluation by his Neurologist. A similar episode occurred on July 6, 2010 and he was hospitalized for one day at ST. Marks Hospital.
Again, an extensive evaluation was completed, but the conclusion was that this episode was a result of dehydration. An electroencephalogram was performed by his Neurologist July 19, 2010. This was normal in the awake state, but demonstrated minor abnormalities while asleep.
He continues to benefit from some employment, but not to the level of his desire and capability.
On September 16, 2014 during a telephone conversation, his situation continues with important activities, but not with employment consistent with his level of talent.
CASE IV
This remarkable 84-year-old female and her talented husband (a highly regarded building contractor) enjoyed a pleasant and rewarding life, particularly in becoming the parents of five outstanding children. Between July 1963 and August 1965 the family with five small children moved to Hawaii so the father could direct a very extensive project. This is still remembered as a wonderful experience.
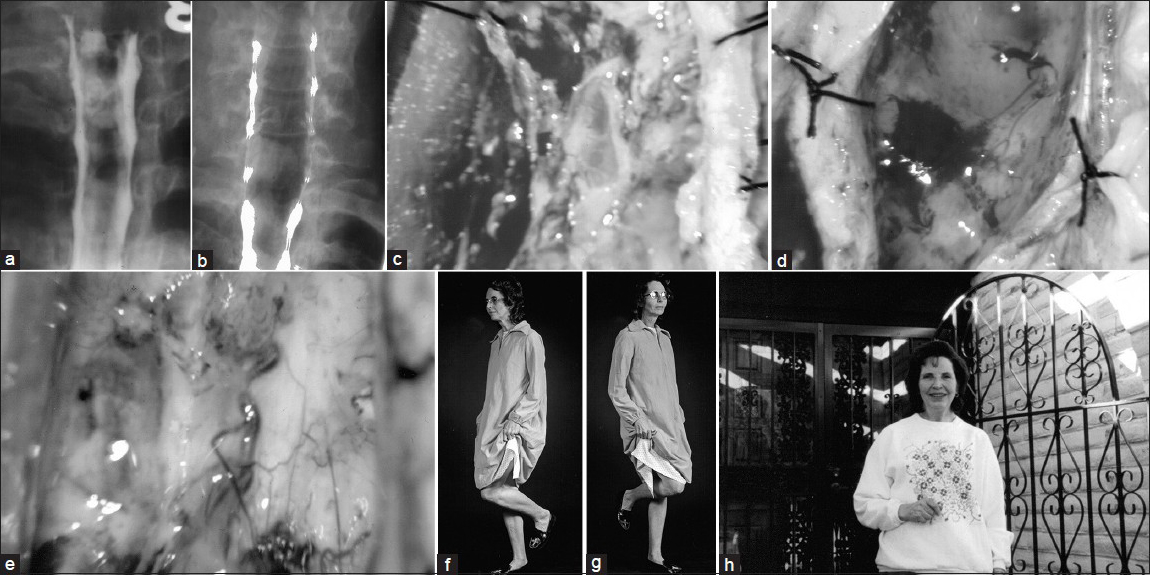
During August of 1969 their life made a sudden change, when she began to notice tingling in her left third, fourth, and fifth fingers with extension up to the elbow. She then developed intermittent burning (left greater than right), which involved hands, elbows, and shoulders. A myelogram was performed on July 28, 1971. This demonstrated a complete block at C-7 to T-1 [
Figure 4
(a) Myelogram (July 28, 1971) shows complete block at C-7 to T-1. (b) Myelogram (November 16, 1971) shows that complete block has been relieved, but that cervical spinal cord is extremely enlarged by the tumor. (c) Operative exposure through microscope shows small mid line cystic exposure of tumor. (d) Midline exposure has been increased for exposure and removal of tumor. Upper: tumor. Lower: small drop of blood. (e) Tumor completely removed. Anterior spinal artery and branches easily visualized from behind and fully protected. (f) Early in postoperative period patient able to stand with stability on right foot, which was impossible prior to surgical removal of tumor. (g) Early in postoperative period patient able to stand with stability on left foot, which was impossible prior to surgical removal of tumor. (h) Patient at her home as she eagerly plans to participate at the 22nd Annual Richard Lende Conference at Snowbird, Utah on February 7, 1995
Her condition remained sufficiently stable that additional surgery was delayed until December 10, 1976 when she came to Chicago for surgery at Loyola University Medical Center.
The spinal cord was exposed from C-3 to C-7 through the scar tissue from initial surgery. An opening was made through the dura, which was retracted and a small cystic area was visualized at the C-4 and C-5 level [
Postoperatively, she began immediately to experience neurological improvement, but because of previous radiation and scar tissue the wound developed some spinal fluid drainage and required wire closure of the dehiscence for longer healing. She made rapid improvement and could now stand with reliable stability on either foot [Figure
The patient was pleased to participate at the 22nd Annual Richard Lende Conference at Snowbird, Utah February 7, 1995. This photograph [
It became my (OHR) wonderful opportunity to visit the patient and her husband at their home on December 11, 2010 and learn of their enthusiasm about continuing activities. They have enjoyed extensive travel with their outstanding family. Many of these include visits to foreign countries to participate in their children's important responsibilities. These opportunities continue as discussed by telephone on June 18, 2012 and again March 30, 2013.
DISCUSSION
Myeolography, ventriculography, and angiography were always performed by the neurological surgeon. The first publication on DIAGNOSTIC NEURORADIOLOGY was authored by Juan M. Taveras, M.D. and Ernest H. Wood, M.D. and published by Williams and Wilkins Company in 1964. The prodigy of Dr. Taveras, David O. Davis, M.D., came to the University of Utah Medical Center in September 1970. He introduced selective “four vessel” cerebral arteriography using transfemoral catheterization. He also introduced high quality magnification and subtraction capability, which proved very important for me in the selection and evaluation of my first 28 patients for EC-IC bypass surgery, which were performed at the University of Utah Medical Center.
At Loyola University Medical Center, we were successful in the acquisition of one of the first five units introducing computed tomography (CT) for shipment to the United States in 1974. This new technology was published by The C. V. Mosby Company in 1981 and authored by Thomas H. Newton, M.D. and D. Gordon Potts, M.D.
Anne G. Osborn, M.D., F.A.C.R. authored DIAGNOSTIC NEURORADIOLOGY, which was published by Mosby in 1994. This described the new technology of magnetic resonance imaging (MRI). One of the first units was installed at the University of Utah Medical Center in June 1986.
These new technological advances have proven very successful in simplifying and improving outcomes for patients with very threatening problems. In my own experience, none of the new technologies existed during the first third of my practice. CT was very helpful during the next third of my practice. MRI was very helpful during the final third of my practice, surprisingly for clearly defining the margin around arteriovenous malformations and surrounding brain tissue.
While these new advances have proven so important, the responsible physician should not overlook the example described in Fisher's Rules (17) and should provide adequate time and attention for each patient. Also, the physician should not be overly influenced by statistics and “evidence-based medicine.” Statistics may be important and helpful; they can be very misleading. “Potential problems arise from involvement of private enterprises that have much to gain and much to lose depending upon trial results” (Louis R. Caplan, M.D.). “I have always believed that stroke is caused by a very heterogeneous array of different cardiac, extracranial vascular, and intracranial hemorrhagic conditions and that treatment depends on identifying the specific cause in the individual patient” (Louis R. Caplan, M.D.).
Statistical randomized trials are very expensive and difficult to complete. Therefore, numerous compromises are always accepted in the effort to complete them in a reasonable time period. Entrance criteria are always poorly defined. Several years may be required to adequately evaluate any benefit or lack of benefit from treatment.
CONCLUSION
The combinations of patriotism and curiosity have influenced many leaders in Neurological Surgery to make many very important advances during each of the past decades. It became my good fortune to make the best, but most difficult, professional decision in my life to enter the field of Neurological Surgery at this significant time. It became my opportunity to participate actively in most of these advances.
I enjoyed a very interesting and rewarding practice of Neurological Surgery in Salt Lake City between 1964 and 1973. The dumbest professional mistake that I ever made was to destroy the unused records of the period (1964-1973) when I left Chicagoland in 1997. A treasure-trove of information was lost!