- Institute of Neuroscience, El Bosque University, Bogota, Colombia
- Department of Neurosurgery, Shaio Clinic, Bogota, Colombia
Correspondence Address:
Javier A. Jacobo Vasquez
Department of Neurosurgery, Shaio Clinic, Bogota, Colombia
DOI:10.4103/2152-7806.176132
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jacobo Vasquez JA, Fonnegra JR, Diez JC, Fonnegra A. Treatment of epidermoid tumors with gamma knife radiosurgery: Case series. Surg Neurol Int 10-Feb-2016;7:
How to cite this URL: Jacobo Vasquez JA, Fonnegra JR, Diez JC, Fonnegra A. Treatment of epidermoid tumors with gamma knife radiosurgery: Case series. Surg Neurol Int 10-Feb-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/treatment-of-epidermoid-tumors-with-gamma-knife-radiosurgery-case-series/
Abstract
Background:Epidermoid tumors (ETs) are benign lesions that are treated mainly by means of surgical resection, with overall good results. External beam radiotherapy is an alternative treatment for those recurrent tumors, in which a second surgery might not be the best choice for the patient. A little information exists about the effectiveness of gamma knife radiosurgery for the treatment of newly diagnosed and recurrent ETs. We present three cases of ETs treated with gamma knife radiosurgery.
Case Description:Case 1 is a 21-year-old female with an ET located in the left cerebellopontine angle (CPA) with symptoms related to VIII cranial nerve dysfunction. Symptom control was achieved and maintained after single session radiosurgery with gamma knife. Case 2 is a 59-year-old female patient with the history of trigeminal neuralgia secondary to a recurrent ET located in the left CPA. Significant pain improvement was achieved after treatment with gamma knife radiosurgery. Case 3 is a 29-year-old male patient with a CPA ET causing long lasting trigeminal neuralgia, pain relief was achieved in this patient after gamma knife radiosurgery.
Conclusion:Long-term symptom relief was achieved in all three cases proving that gamma knife radiosurgery is a good and safe alternative for patients with recurrent or nonsurgically treated ETs.
Keywords: Epidermoid cyst, epidermoid tumor, gamma knife, radiosurgery, trigeminal neuralgia
INTRODUCTION
Epidermoid tumors (ETs) are rare benign lesions of embryonic origin; they represent nearly 0.5% of all intracranial lesions.[
It is believed that the origin of these tumors results from the inclusion of ectoderm cells at the time of the closure of the neural tube between the 3rd and 5th week of embryonic life.[
ETs are most commonly located intracranially in the cerebellopontine angle (CPA),[
Surgical resection with the preservation of neurological function is the standard of care for intracranial ET. However, complete resection of the lesion is not always possible, adherence to the lesion walls to important neurovascular structures makes achieving this goal, nearly impossible in some instances.[
Radiotherapy has not been used extensively to treat ET, but several reports of its efficacy have been published.[
We show a series of three cases of ET presenting with cranial nerve dysfunction treated with gamma knife radiosurgery (GKS), and the results obtained by the patients.
CASE REPORTS
Case 1
A 21-year-old female patient presented with a headache, vertigo, tinnitus, and gait ataxia. Magnetic resonance imaging (MRI) revealed a heterogeneous lesion located in the left CPA, which was compatible with an ET. The lesion was in close relationship with the fifth, sixth, and seventh cranial nerves, and was displacing the brainstem contralaterally.
The patient was offered surgery but refused treatment, and so GKS was offered as an alternative.
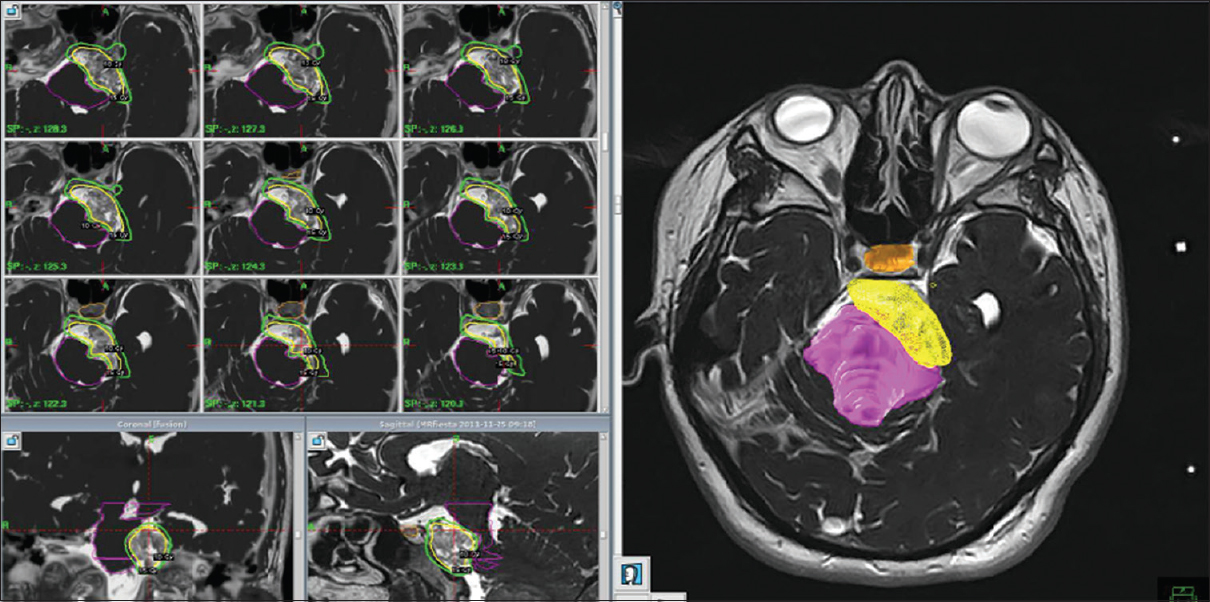
The tumor had a total volume of 7.1cc and was treated in a single session with a dose of 15 Gy at 55% margin isodose, maximum dose of 27.3 Gy [
At the follow-up period of 46 months, the patient had significant improvement of vertigo and tinnitus, with a headache remaining with similar characteristics. MRI at 6 months after surgery showed no significant changes.
Case 2
A 59-year-old female patient with 10 years history of trigeminal neuralgia secondary to a documented ET that was surgically treated at that time. The patient showed improvement of her pain symptoms but recurred after 6 years, she was then taken to surgery once more, but because of scar tissue in the CPA removal of the lesion was not possible; she had a VII and VIII nerve injury during the second procedure.
Neuropathic pain in the third branch of the trigeminal nerve was persistent and refractory to multiple medical therapies. The patient was referred to our institution for GKS treatment.
On MRI, residual lesion in the left CPA in close relationship with the trigeminal nerve.
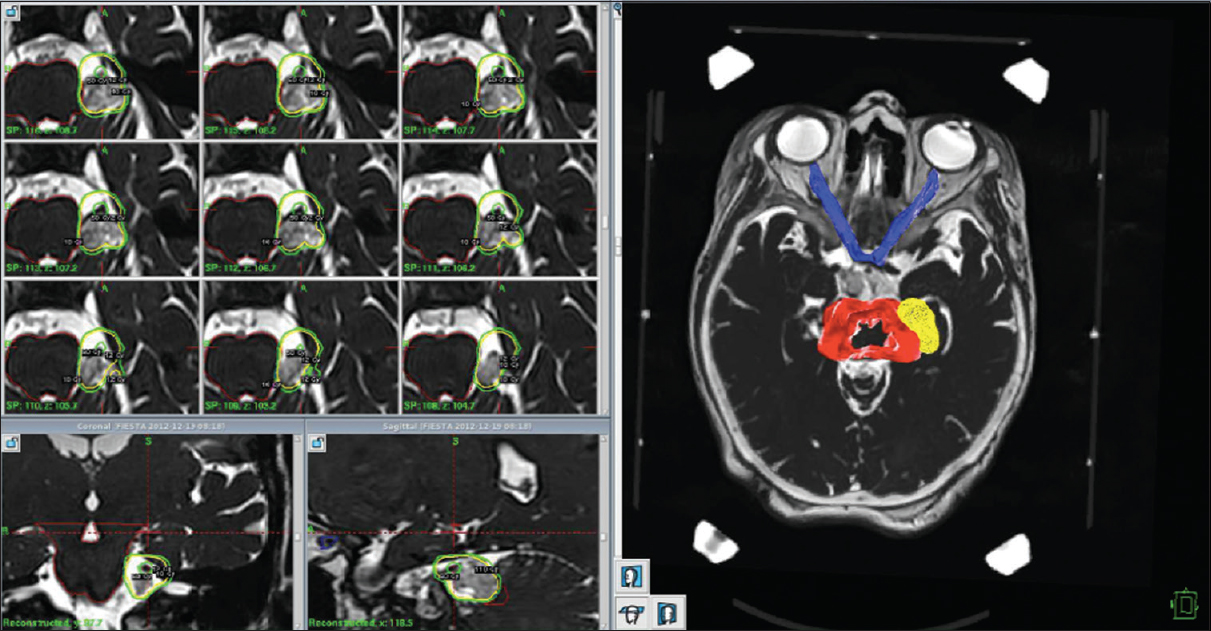
The patient was treated for trigeminal neuralgia with 80 Gy hotspot on the nerve while the tumor received 12 Gy margin dose [
Figure 2
Treatment plan for a patient with an epidermoid tumor and associated trigeminal neuralgia. 80 Gy hotspot was placed on the nerve while modeling 12 Gy isodose around the tumor. The optic pathway received 1.5 Gy on 1% of its volume; brainstem received 9 Gy on 1% of its total volume, and the pineal gland received a total of 1.7 Gy
Follow-up period of 33 moths showed that the patient had significant improvement of the pain; she developed paresthesia in the territory of V3 and continued medical therapy with carbamazepine achieving acceptable symptom control.
Tumor volume remained unchanged in control images.
Case 3
A 29-year-old male patient, with a 6-year long case of trigeminal neuralgia, was treated medically with poor results; the pain was persistent and incapacitating.
An MRI study showed a lesion located in the CPA that was in close relationship with the V, VI, VII, and VII nerves.
Surgery was considered in this patient, but because of the low morbidity associated with GKS, a trial treatment was done with the intent of pain resolution and tumor growth control.
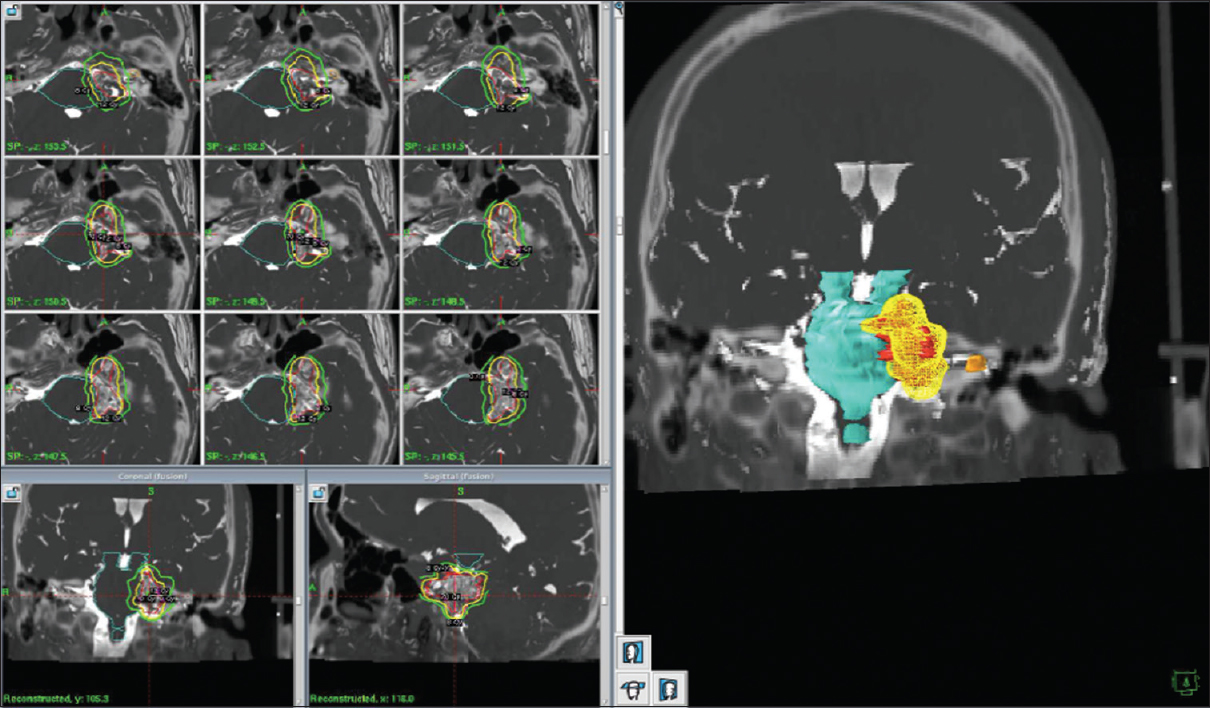
For this patient, treatment was addressed to improve pain as well, so a hotspot of 80 Gy was placed on the trigeminal nerve, meanwhile, the tumor margin received a dose of 12 Gy. The tumor had a total volume of 5.8cc [
The patient was followed after 34 months; the pain had completely gone away and received no medical treatment. Control images showed no tumor growth.
DISCUSSION
ETs are most frequently found in the CPA, and cranial nerve dysfunction is a common presenting symptom. Trigeminal neuralgia in patients with CPA ETs has been reported to vary from 0% to 76.9% depending on the series.[
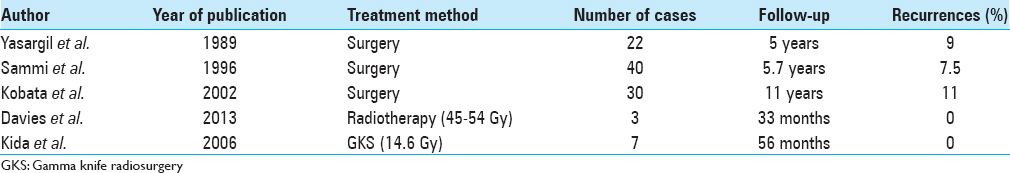
Surgical resection is the main treatment for symptomatic tumors, and many active trials have been reported.[
Samii et al. presented his experience with surgical resection of posterior fossa ET, achieving complete resection in 30 of the 40 cases presented.[
For patients who have failed surgical treatment or recurrence is documented, radiotherapy has been used as an alternative with fairly good results. The effects of radiotherapy on ET have been assessed in a few case reports,[
Davies et al. presented a series of three cases of ET that recurred after surgery; they treated these patients with conventional radiotherapy with doses varying from 45 Gy to 54 Gy given at 1.8 Gy per daily fraction. Patients achieved tumor and symptom control with a mean follow-up period of 33 months.
We believe that the option of radiosurgery should be given to the patients and should be considered for patients in whose surgery is not the best options or patients who refuse surgical treatment.
We present the three cases of ET causing cranial nerve dysfunction, two patients presented with trigeminal neuralgia, and one patient showed VIII nerve dysfunction with tinnitus and vertigo. All three patients were treated with GKS and showed significant improvement in their symptoms, and after 46 months of follow-up no recurrence has been reported [
Only one case series of ET treated with GKS could be found on this literature search. Kida et al.[
It should be noted that in this case series an additional boost was delivered to the trigeminal nerve, and pain control was achieved, while in the case series presented by Kida et al., no additional radiation was given to the nerve, and still pain control was achieved. This might indicate that pain control may be the result of nerve decompression without the need of nerve lesion by means of direct radiosurgery.
We hope that this case series encourages other gamma knife groups to treat patients with ET, and by doing this, sufficient evidence is obtained so that radiosurgery can be used as a viable alternative for patients with ET and secondary cranial nerve dysfunction.
CONCLUSION
We have shown three different cases of cranial nerve hyperactive dysfunction caused by CPA ETs. Long-term symptom relief was achieved in all three cases proving that GKS is a good and safe alternative for patients with recurrent or nonsurgically treated ET.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Altschuler EM, Jungreis CA, Sekhar LN, Jannetta PJ, Sheptak PE. Operative treatment of intracranial epidermoid cysts and cholesterol granulomas: Report of 21 cases. Neurosurgery. 1990. 26: 606-13
2. Berger MS, Wilson CB. Epidermoid cysts of the posterior fossa. J Neurosurg. 1985. 62: 214-9
3. Chen IH, Huang CI, Lee LS, Teng MH, Ho DM. Hemifacial spasm associated with double compression of facial nerve by benign tumor and tortuous cerebellar artery. J Surg Assoc ROC. 1989. 22: 64-8
4. Cheng TM, Cascino TL, Onofrio BM. Comprehensive study of diagnosis and treatment of trigeminal neuralgia secondary to tumors. Neurology. 1993. 43: 2298-302
5. Davies JM, Trinh VT, Sneed PK, McDermott MW. Radiotherapy for recurrent epidermoid cyst. J Neurooncol. 2013. 112: 307-13
6. deSouza CE, deSouza R, da Costa S, Sperling N, Yoon TH, Abdelhamid MM. Cerebellopontine angle epidermoid cysts: A report on 30 cases. J Neurol Neurosurg Psychiatry. 1989. 52: 986-90
7. Keville FJ, Wise BL. Intracranial epidermoid and dermoid tumors. J Neurosurg. 1959. 16: 564-9
8. Kida Y, Yoshimoto M, Hasegawa T, Fujitani S. Radiosurgery of epidermoid tumors with gamma knife: Possiblility of radiosurgical nerve decompression. No Shinkei Geka. 2006. 34: 375-81
9. Kobata H, Kondo A, Iwasaki K. Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: Pathogenesis and long-term surgical results in 30 patients. Neurosurgery. 2002. 50: 276-85
10. Lunardi P, Missori P, Innocenzi G, Gagliardi FM, Fortuna A. Long-term results of surgical treatment of cerebello-pontine angle epidermoids. Acta Neurochir (Wien). 1990. 103: 105-8
11. Lunardi P, Missori P. Supratentorial dermoid cysts. J Neurosurg. 1991. 75: 262-6
12. Parikh S, Milosevic M, Wong CS, Laperriere N. Recurrent intracranial epidermoid cyst treated with radiotherapy. J Neurooncol. 1995. 24: 293-7
13. Rubin G, Scienza R, Pasqualin A, Rosta L, Da Pian R. Craniocerebral epidermoids and dermoids.A review of 44 cases. Acta Neurochir (Wien). 1989. 97: 1-16
14. Samii M, Tatagiba M, Piquer J, Carvalho GA. Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg. 1996. 84: 14-9
15. Talacchi A, Sala F, Alessandrini F, Turazzi S, Bricolo A. Assessment and surgical management of posterior fossa epidermoid tumors: Report of 28 cases. Neurosurgery. 1998. 42: 242-51
16. Yasargil MG, Abernathey CD, Sarioglu AC. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989. 24: 561-7