- Department of Neurosurgery, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki City, Japan.
Correspondence Address:
Yoichi Morofuji, Department of Neurosurgery, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki City, Japan.
DOI:10.25259/SNI_816_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kazuaki Okamura, Yoichi Morofuji, Nobutaka Horie, Tsuyoshi Izumo, Kei Sato, Takashi Fujimoto, Takayuki Matsuo. Hematoma expansion unrelated to rebleeding in ruptured anterior cerebral artery aneurysms treated by early endovascular embolization. 23-Nov-2021;12:571
How to cite this URL: Kazuaki Okamura, Yoichi Morofuji, Nobutaka Horie, Tsuyoshi Izumo, Kei Sato, Takashi Fujimoto, Takayuki Matsuo. Hematoma expansion unrelated to rebleeding in ruptured anterior cerebral artery aneurysms treated by early endovascular embolization. 23-Nov-2021;12:571. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11244
Abstract
Background: Whether hematoma expansion after aneurysmal rupture is always a sign of rerupture remains unclear. Hence, the present study aimed to assess the incidence and risk factors of hematoma expansion unrelated to aneurysmal rerupture after endovascular embolization for ruptured cerebral aneurysms.
Methods: We included patients who underwent endovascular embolization for ruptured cerebral aneurysms within 48 h after onset at our institution between January 2009 and February 2014. The medical records of 70 consecutive patients were reviewed and analyzed retrospectively.
Results: Hematoma expansion unrelated to aneurysmal rerupture occurred in 7 (10%) of 70 patients. Interestingly, four of seven patients had distal anterior cerebral artery (ACA) aneurysms. The interval from onset to aneurysm coiling was shorter in patients with hematoma expansion than in those without (P = 0.040).
Conclusion: Early embolization of ruptured ACA aneurysms might increase the risk of hematoma expansion unrelated to aneurysmal rerupture because the procedures were conducted under systemic anticoagulation. It would be better to refer the patient for direct clipping if the patient has a distal ACA aneurysm with parenchymal hematoma at interhemispheric fissure. Delayed coil embolization, which means around 12–18 h delayed, might be another option for ruptured distal ACA aneurysms to prevent hematoma expansion.
Keywords: Anticoagulation, Endovascular embolization, Hematoma expansion, Ruptured aneurysm, Subarachnoid hemorrhage
INTRODUCTION
In aneurysmal subarachnoid hemorrhage (aSAH), the major causes of mortality and morbidity include initial hemorrhage, rerupture, and vasospasm. In patients with aSAH, rerupture is associated with poor outcome. The mortality rate is as high as 80% in patients who experience aneurysm rerupture.[
However, whether hematoma expansion after aneurysmal rupture is always a sign of rerupture remains unclear. Since the publication of the International Subarachnoid Aneurysm Trial (ISAT), endovascular embolization has been widely used as an alternative to surgical clip placement for aSAH, and the treatment strategy for the condition was changed from clipping to coiling.[
We have experienced a few complications including hematoma expansion after successful endovascular coiling. Hence, the present study aimed to assess the incidence and risk factors of this complication. Moreover, data on cases involving hematoma expansion unrelated to aneurysmal rerupture after endovascular embolization for ruptured cerebral aneurysms were discussed.
MATERIALS AND METHODS
Patient population
We included patients who underwent endovascular embolization for ruptured cerebral aneurysms within 72 h after onset at our institution between January 2009 and August 2014. The medical records of 70 consecutive patients were reviewed and analyzed retrospectively. The following data were obtained from each patient: age, sex, World Federation of Neurosurgical Societies and Fisher grades, aneurysm location, size of aneurysm, time from onset to aneurysm coiling, and modified Rankin scale score at discharge. The clinical study protocol was reviewed and approved by the Institutional Review Board of Nagasaki University Hospital, and all patients provided a written informed consent.
Radiological evaluation
All patients underwent computed tomography (CT) scan 72 h after symptom onset. A second CT scan was required within 24 h after endovascular embolization. The presence of aneurysm was confirmed through CT angiography (CTA) or digital subtraction angiography. Initial CT scan images were classified according to the Fisher grading system. Hematoma expansion was defined as subarachnoid hemorrhage or intraparenchymal hematoma growth observed between the first and second follow-up CT scans without clinical signs of aneurysmal rebleeding, such as neurological deterioration and changes in vital signs.
Routine endovascular procedure
The treatment method was selected according to the CTA results, and endovascular embolization was the preferred strategy for the treatment of aSAH at our institution. However, craniotomy was commonly recommended to patients with extremely small, wide-neck, MCA, and anterior choroidal artery aneurysms. The patients normally underwent endovascular coiling under general anesthesia right after radiological evaluation or on the next morning. To maintain an activated clotting time of 250 s, all endovascular procedures were performed under systemic anticoagulation through the intra-arterial administration of heparin. Initial heparin was administrated just after arterial access. All patients were admitted to the intensive care unit or stroke care unit and were closely evaluated through continuous monitoring of arterial blood pressure and electrocardiography after the procedures.
Data analysis
Statistical analysis of categorical variables was performed using the Chi-square test or the t-test (GraphPad Inc., San Diego, CA, USA). P < 0.05 was considered statistically significant.
RESULTS
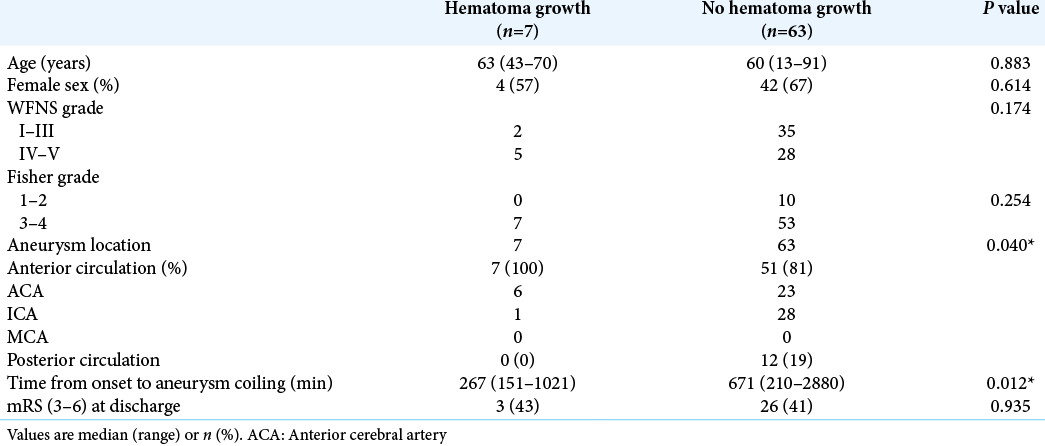
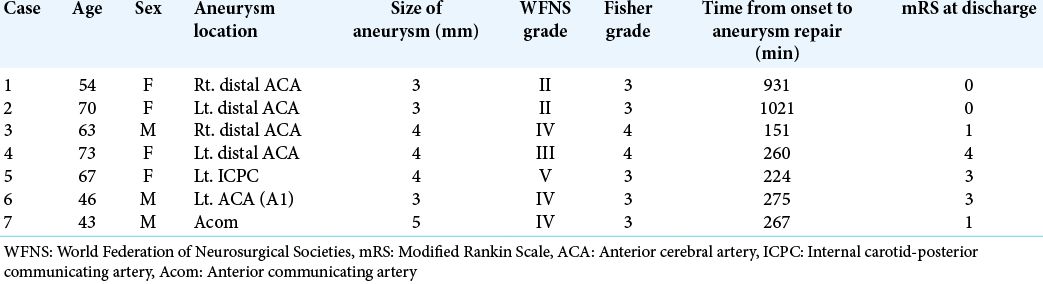
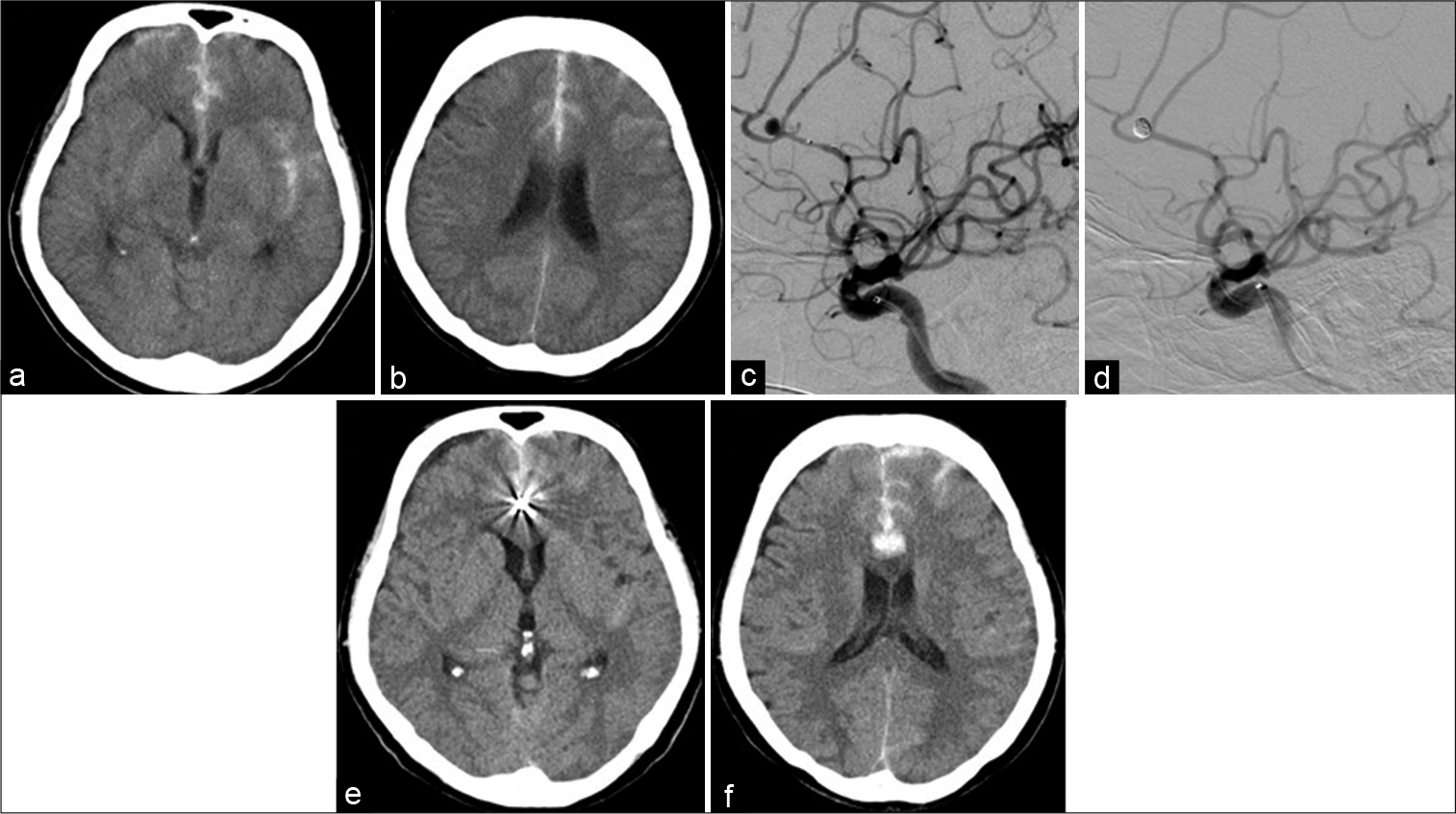
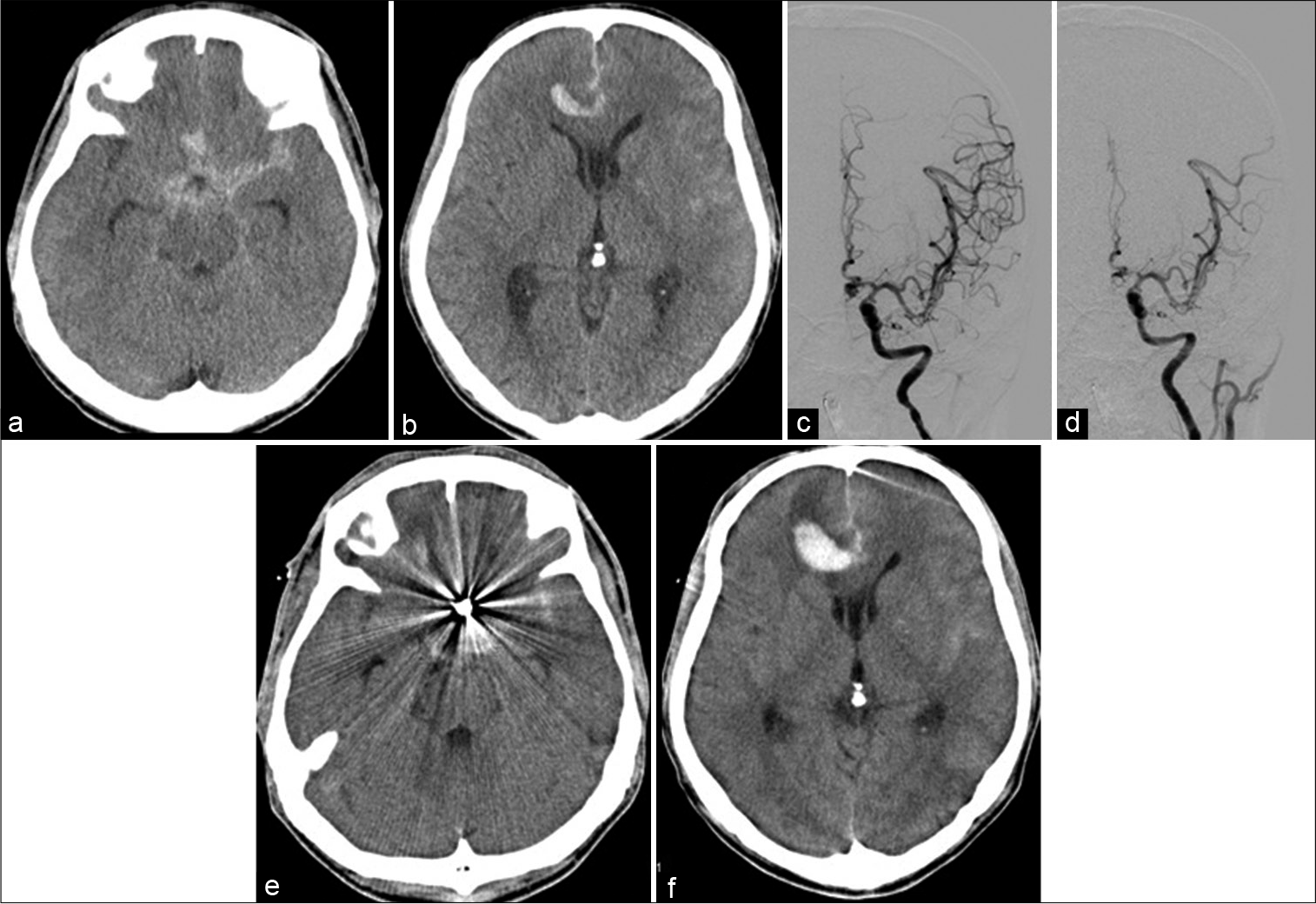
Hematoma expansion unrelated to aneurysmal rerupture occurred in 7 (10%) of 70 patients. The characteristics of patients and aneurysms are shown in [
Illustrative cases
Case 2
A 70-year-old woman presented with sudden and severe headache. She was then brought to our institution. CT scan showed a dense subarachnoid hemorrhage in the interhemispheric fissure. CTA revealed saccular aneurysm at the distal ACA, which was successfully coiled. Follow-up CT scan performed on the next day revealed hematoma formation in the interhemispheric fissure, which was distant from the embolized aneurysm. The hematoma was small, and the patient was treated conservatively [
Figure 1:
Images obtained from a 70-year-old woman with subarachnoid hemorrhage. (a and b) Computed tomography scan on admission revealed subarachnoid hemorrhage in the interhemispheric fissure. (c) Preoperative left carotid angiogram showed a saccular aneurysm at the distal anterior cerebral artery. (d) Postoperative left carotid angiogram after coiling revealed complete obliteration of the aneurysm. (e and f) Computed tomography obtained a day after coiling revealed hematoma formation in the interhemispheric fissure.
Case 7
A 43-year-old man was transferred to our institution and was diagnosed with subarachnoid hemorrhage. CT scan showed a subarachnoid clot in the basal cistern and a small hematoma in the right medial frontal lobe facing the interhemispheric fissure. CTA revealed a saccular aneurysm at the anterior communicating artery, and the aneurysm was successfully coiled without any difficulties. Follow-up CT scan conducted on the next day showed hematoma enlargement, which was apparently distant from the embolized aneurysm [
Figure 2:
Images obtained from a 43-year-old man who was transferred to our institution and was diagnosed with subarachnoid hemorrhage. (a and b) Computed tomography scan on admission revealed subarachnoid hemorrhage in the basal cistern and a small hematoma in the right medial frontal lobe facing the interhemispheric fissure. (c) Preoperative left carotid angiogram showed a saccular aneurysm at the anterior communicating artery. (d) Postoperative left carotid angiogram after coiling revealed complete obliteration of the aneurysm. (e and f) Computed tomography scan performed a day after coiling revealed hematoma enlargement in the right frontal lobe. The hematoma was apparently distant from the embolized aneurysm.
DISCUSSION
The present study showed that there exist cases with hematoma expansion unrelated to aneurysmal rerupture after successful embolization of ruptured ACA aneurysms.
In a previous study, hemorrhage extended to the brain parenchyma in 20% of patients with aSAH.[
A previous study has shown that a thick or dense SAH can compress and further damage the pia mater or the small vessels surrounding the hematoma. This phenomenon causes intracerebral hematoma enlargement.[
The present study indicated that early coil embolization might be a risk factor for hematoma expansion. Early endovascular procedures with systemic anticoagulation may promote hematoma growth. Early intervention can definitely prevent rerupture. However, systemic heparinization is associated with hematoma growth in coil embolization, especially for SAH patients with parenchymal hematoma or with distal ACA aneurysms. The previous studies have shown that angiography increased the risk of rebleeding until 3 h after SAH.[
Since the publication of ISAT, endovascular embolization has been used as an alternative to surgical clip placement for aSAH. The treatment strategy for this condition was changed from clipping to coiling. However, direct clipping or delayed coil embolization might be recommended for SAH with a hematoma or dense/thick SAH in ruptured distal ACA aneurysms.
The present study had several limitations. It has a retrospective nature, and it was subject to selection bias and deviations. In addition, the sample size was small. Thus, a statistical analysis could not be performed.
CONCLUSION
The present study showed that there exist cases with hematoma expansion unrelated to aneurysmal rerupture after successful embolization of ruptured ACA aneurysms because the procedures were conducted under systemic anticoagulation. It might be better to refer the patient for direct clipping if the patient has a distal ACA aneurysm with parenchymal hematoma at interhemispheric fissure. Delayed coil embolization, which means around 12–18 h delayed, might be another option for ruptured distal ACA aneurysms to prevent hematoma expansion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. An H, Park J, Kang DH, Son W, Lee YS, Kwak Y. Should Cerebral Angiography Be Avoided within Three Hours after Subarachnoid Hemorrhage?. J Korean Neurosurg Soc. 2019. 62: 526-535
2. Chang SH, Shin HS, Lee SH, Koh HC, Koh JS. Rebleeding of Ruptured Intracranial Aneurysms in the Immediate Postoperative Period after Coil Embolization. J Cerebrovasc Endovasc Neurosurg. 2015. 17: 209-216
3. Egashira Y, Yoshimura S, Enomoto Y, Ishiguro M, Asano T, Iwama T. Ultra-early endovascular embolization of ruptured cerebral aneurysm and the increased risk of hematoma growth unrelated to aneurysmal rebleeding. J Neurosurg. 2013. 118: 1003-1008
4. Lim YC, Kim C-H, Kim YB, Joo J-Y, Shin YS, Chung J. Incidence and Risk Factors for Rebleeding during Cerebral Angiography for Ruptured Intracranial Aneurysms. Yonsei Med J. 2015. 56: 403-409
5. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002. 360: 1267-1274
6. Tanikawa R. [Less invasive cistemal approach and removal of subarachnoid hematoma for the treatment of ruptured cerebral aneurysms]. No Shinkei Geka. 2007. 35: 17-24
7. van Asch CJ, Oudendijk JF, Rinkel GJ, Klijn CJ. Early intracerebral hematoma expansion after aneurysmal rupture. Stroke. 2010. 41: 2592-2595