- Department of Neurosurgery, Otsu City hospital, Otsu, Shiga, Japan.
- Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan.
Correspondence Address:
Motohiro Takayama, Department of Neurosurgery, Otsu City hospital, Otsu, Shiga, Japan.
DOI:10.25259/SNI_157_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Motohiro Takayama1, Yoshinori Maki2, Toshinari Kawasaki1. Cauda equina syndrome after L5-S1 posterior decompression surgery showing a “convexity sign” caused by engorgement of the ventral epidural venous plexus: A case series. 04-Mar-2022;13:82
How to cite this URL: Motohiro Takayama1, Yoshinori Maki2, Toshinari Kawasaki1. Cauda equina syndrome after L5-S1 posterior decompression surgery showing a “convexity sign” caused by engorgement of the ventral epidural venous plexus: A case series. 04-Mar-2022;13:82. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11442
Abstract
Background: Cauda equina syndrome (CES) following posterior lumbar decompression is rare. Here, we present four postoperative cases of L5S1 surgery resulting in CES attributed to engorged ventral epidural veins that decreased spontaneously in three cases, while the fourth warranted a laminoplasty.
Case Description: Four patients underwent posterior lumbar decompressions at the L5-S1 level, but developed postoperative symptoms/signs of CES. Interestingly, in all four cases, cauda equina compression was attributed to engorgement of the ventral epidural venous plexus documented on magnetic resonance images (MRI) by the “convexity sign.” Postoperatively, three patients’ CES compression decreased spontaneously, but one required a laminoplasty.
Conclusion: Postoperative CES occurred in four patients undergoing L5-S1 lumbar surgery. This deficit was attributed to marked engorgement of the ventral epidural plexus (i.e., yielding the “convexity sign” on MRI) that resolved spontaneously in three patients, but warranted a laminoplasty in the fourth.
Keywords: Cauda equina syndrome, Dysuria, Epidural venous plexus, L5-S1, Posterior lumbar decompression
INTRODUCTION
Cauda equina syndrome (CES) is rarely seen in patients following lumbar surgery.[
CASE PRESENTATION
Four patients, ranging in age from 54 to 70, underwent lumbar decompressive procedures (three patients), and/or lumbar fusions [
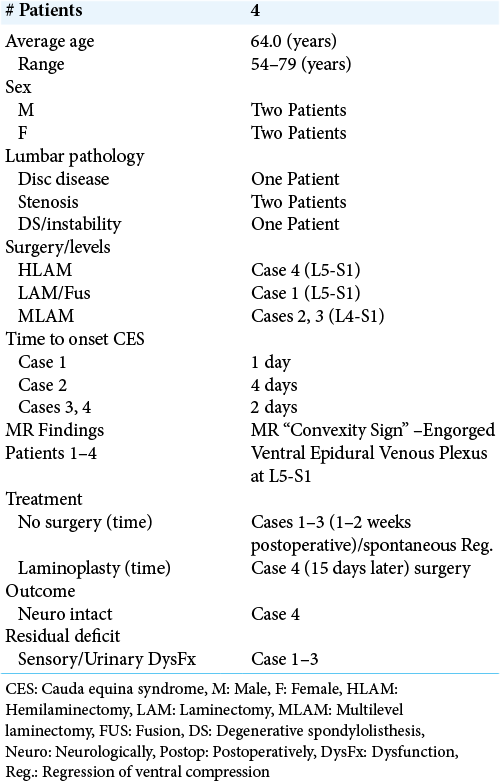
Figure 1:
Magnetic resonance images of Case 1 (a) spondylolisthesis was present at the L5-S1 level, and the dural sac terminated at S1. (b and c) The postoperative MR showed the dorsal shift of the thecal sac (white arrow heads) attributed to the ventrally engorged epidural venous plexus (a white arrow and dotted line; i.e., the “convexity sign”). (d) Seven years postoperatively, the ventrally engorged epidural venous plexus could still be seen.
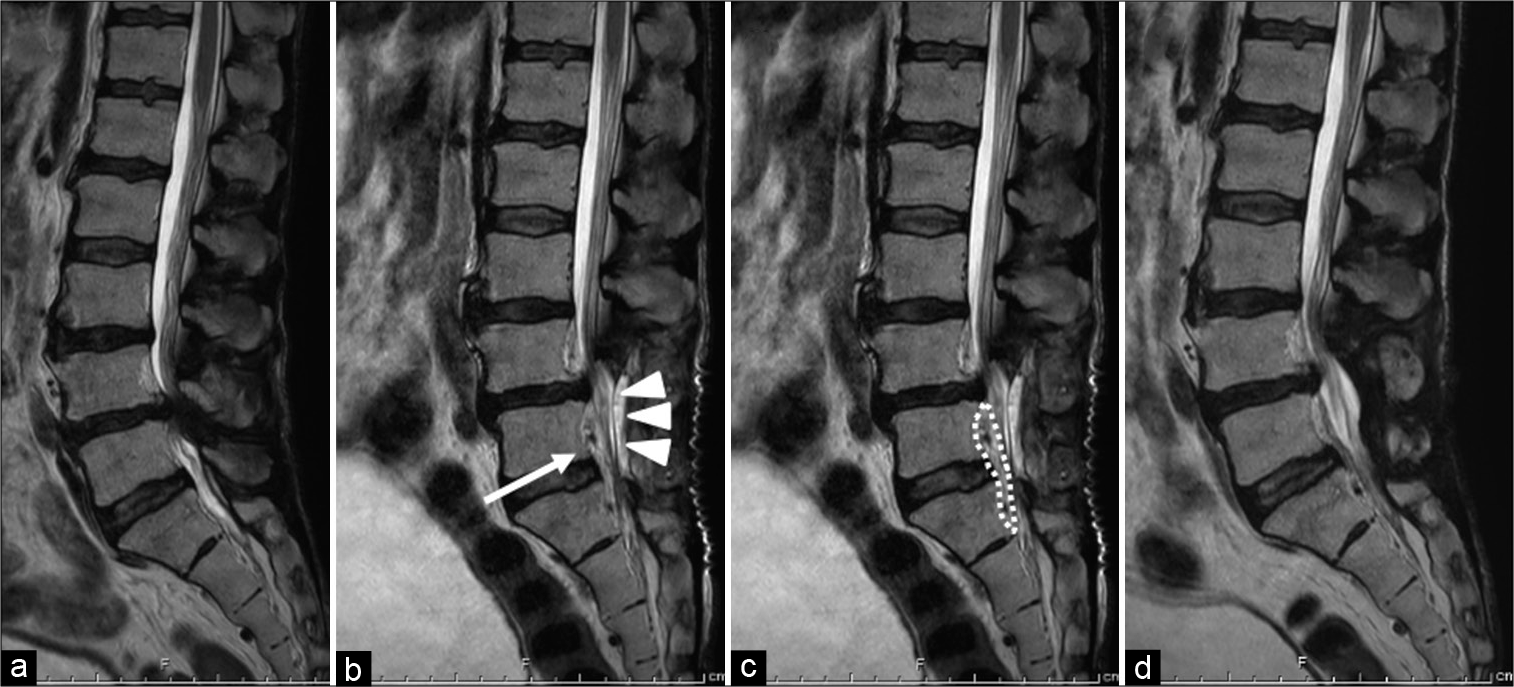
Figure 2:
Magnetic resonance images of Case 2 (a) lumbar spinal canal stenosis was observed at the L4-L5 level. (b and c) The postoperative MR revealed ventral dural sac compression (white arrow heads) attributed to the engorged ventral epidural venous plexus (a white arrow and dotted line; that is, the “convexity sign.” (d) Six months later, the MR demonstrated a reduction in ventral compression, but not full resolution.
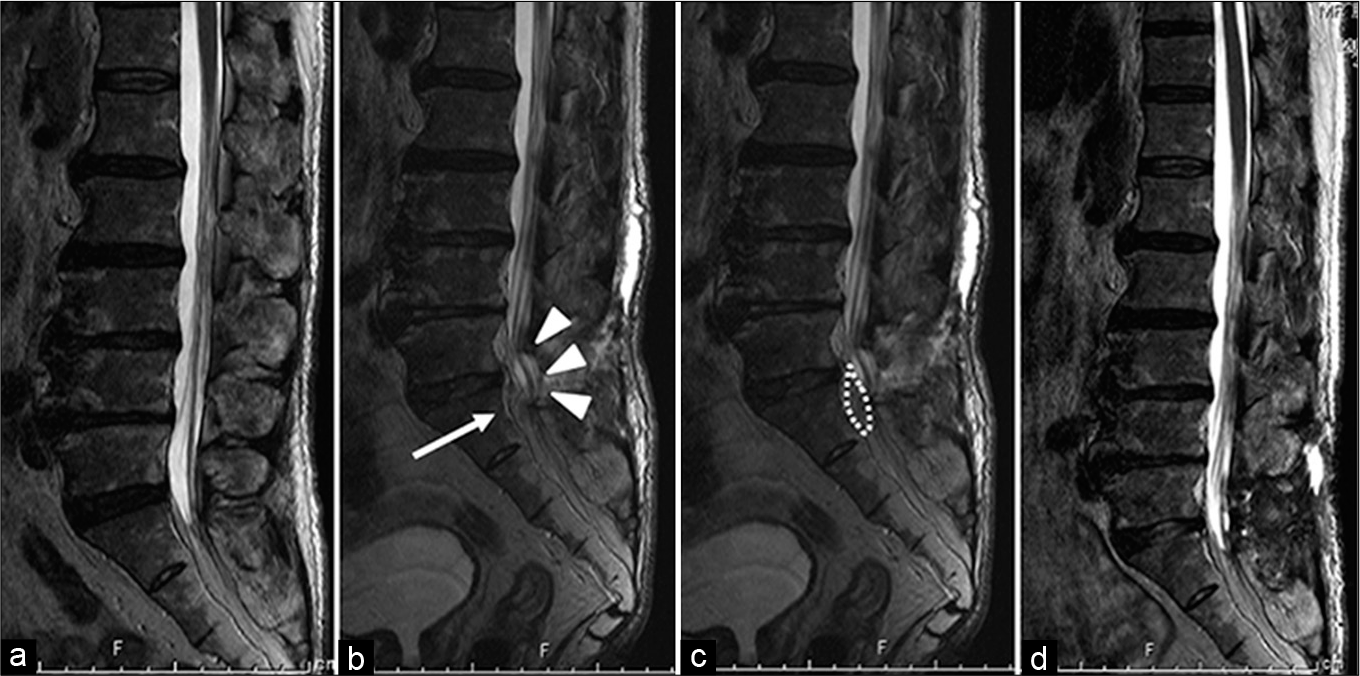
Figure 4:
Magnetic resonance images of Case 4 (a) the dural sac terminated at S1 level. (b and c) Postoperative MR images revealed ventral compression of dural sac (white arrow heads) due to the engorged ventral epidural venous plexus (a white arrow and dotted line). (d) After laminoplasty and coagulation of the ventral epidural venous plexus, the dural sac ventral compression was relieved.
DISCUSSION
We describe four cases of CES following posterior lumbar decompression surgery at the L5-S1 level. TCES in all cases was attributed to engorgement of the ventral epidural venous plexus diagnosed on MR by the “convexity sign.” We previously and again here reported a postoperative CES case attributed to an engorged ventral venous plexus (i.e., Case 4 in this study); this case was successfully treated with a laminoplasty that included coagulation of the engorged ventral venous plexus.[
CES following lumbar discectomy was described by McLaren and Bailey, and they elucidated that insufficient bony removal could result in postoperative CES.[
CONCLUSION
Neurosurgeons should be aware that postoperative CES may develop due to marked engorgement of the ventral epidural venous plexus after posterior decompression surgery at the L5-S1 level.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Henriques T, Olerud C, Petrén-Mallmin M, Ahl T. Cauda equina syndrome as a postoperative complication in five patients operated for lumbar disc herniation. Spine (Phila Pa 1976). 2001. 26: 293-7
2. Maki Y, Takayama M, Hayashi H, Yokoyama Y, Agawa Y. Cauda equina syndrome due to dural sac shift with engorgement of the epidural venous plexus: Rare complication after lumbar microdiscectomy. World Neurosurg. 2017. 104: 1048.e15-8
3. Mclaren AC, Bailey SI. Cauda equina syndrome: A complication of lumbar discectomy. Clin Orthop Relat Res. 1986. 204: 143-9
4. Podnar S. Cauda equina lesions as a complication of spinal surgery. Eur Spine J. 2010. 19: 451-7