- Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan
- Department of Pathology, Juntendo University Urayasu Hospital, Urayasu, Japan
Correspondence Address:
Satoshi Tsutsumi, Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan.
DOI:10.25259/SNI_782_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Keisuke Murofushi1, Satoshi Tsutsumi2, Shigeki Tomita1, Motoki Yamataka1, Natsuki Sugiyama1, Hideaki Ueno1, Hisato Ishii1. Frontal nerve schwannoma in a 16-year-old girl presenting with a rapid growth for 2 years. 01-Nov-2024;15:400
How to cite this URL: Keisuke Murofushi1, Satoshi Tsutsumi2, Shigeki Tomita1, Motoki Yamataka1, Natsuki Sugiyama1, Hideaki Ueno1, Hisato Ishii1. Frontal nerve schwannoma in a 16-year-old girl presenting with a rapid growth for 2 years. 01-Nov-2024;15:400. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13192
Abstract
Background: Orbital schwannomas arising from the frontal nerve are a rare but distinct entity.
Case Description: A 16-year-old girl presented to our hospital with gradually progressive proptosis. Computed tomography (CT) performed 2 years ago incidentally detected a retrobulbar mass in the left orbit measuring 13 mm × 14 mm × 10 mm, which was not identified on CT performed at the age of 4 years. CT taken at presentation revealed marked tumor growth over 2 years, measuring 24 mm × 20 mm × 17 mm. On magnetic resonance imaging (MRI), the tumor appeared homogeneously isointense both on the T1- and T2-weighted sequences. The patient underwent transcranial tumor resection. Following unilateral frontal craniotomy, an osteotomy was made to the left anterior fossa floor. On reflecting, the periorbita revealed the frontal nerve with the proximal segment intermingled with the tumor. The levator and superior rectus muscles were flattened and located immediately beneath the tumor. A gross total resection was performed. Microscopic findings of the resected tumor were consistent with schwannoma.
Conclusion: Frontal nerve schwannomas may grow rapidly under certain conditions. Periodic follow-up using MRI and timely resection is recommended when an asymptomatic orbital tumor, possibly a frontal nerve schwannoma, is detected in young patients.
Keywords: Frontal nerve, Orbital tumor, Schwannoma, Transcranial approach
INTRODUCTION
Peripheral nerve sheath tumors of the orbit and ocular adnexa are a distinct group of neoplasms characterized by nonspecific clinical presentations, variable tumor locations, challenging therapeutic efforts, and occasional diagnostic dilemmas.[
The frontal nerve is an orbital branch of the first trigeminal division.[
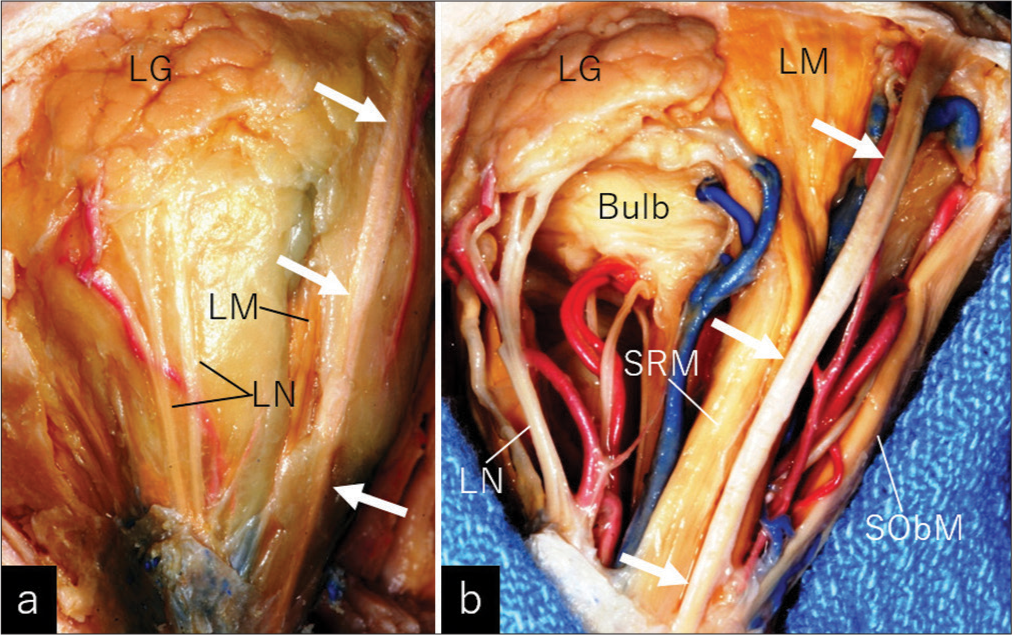
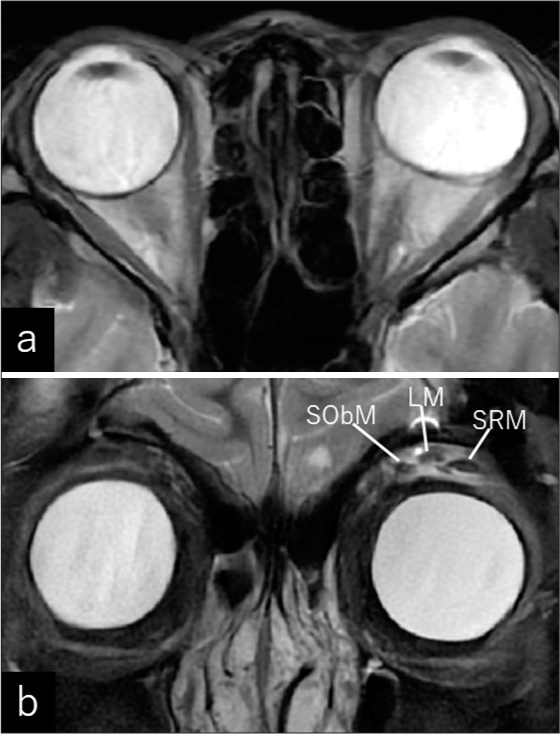
Figure 1:
Superolateral and posterior view of a dissected left orbit, after removing the (a) superior and lateral walls and (b) fat tisue, show the frontal nerve consistently coursing on the upper surface of the levator muscle, just beneath the periorbita (arrows). LG: Lacrimal gland, LM: Levator palpebral superioris muscle, LN: Lacrimal nerve, SObM: Superior oblique muscle, SRM: Superior rectus muscle. The dissection was performed by one of the authors (S.T.).
Herein, we report a case of frontal nerve schwannoma in an adolescent girl that rapidly grew over 2 years and was resected through the transcranial route.
CASE PRESENTATION
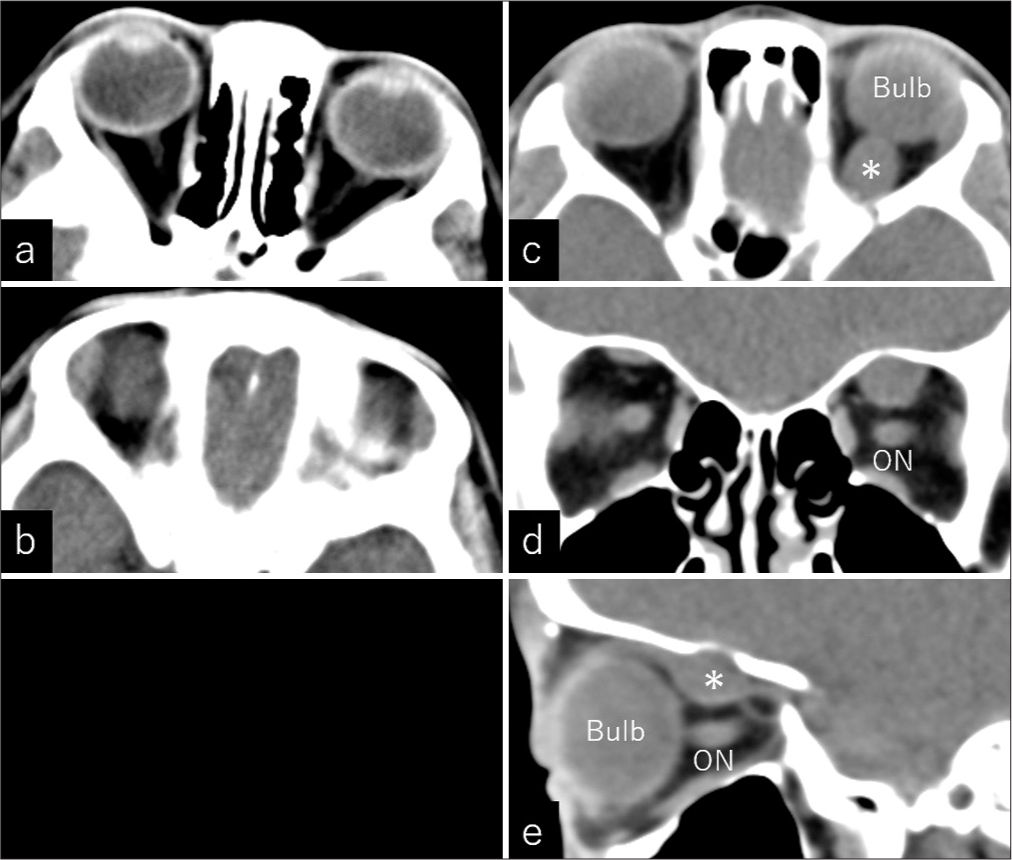
A 16-year-old previously healthy girl presented to the hospital with gradually progressing, painless proptosis for 1 year. Her medical history was unremarkable, and she had not undergone any prior orbital surgery. Computed tomography (CT) performed at the age of 4 years for an accidental simple head injury did not reveal any abnormal findings in the left orbit [
Figure 2:
(a and b) Non-contrast axial computed tomography scans taken at the age of 4 years do not show any lesion in the left superior orbit. (c-e) Non-contrast (c) axial, (d) coronal, and (e) sagittal computed tomography scans taken at the age of 14 years show a small retrobulbar mass in the left superior orbit, measuring 13 mm × 14 mm × 10 mm (asterisk) ON: Optic nerve.
Figure 3:
Non-contrast (a) axial, (b) coronal, and (c) sagittal computed tomography scans taken at the presentation show an oval-shaped tumor in the left superior orbit, measuring 24 mm × 20 mm × 17 mm, indicating a marked tumor growth for recent 2 years. Intralesional calcifications or hemorrhagic changes are not found. (d-f) Post-contrast coronal computed tomography performed at the presentation, at the levels of the (d) orbital apex, (e) maximal dimension of the tumor, and (f) anterior ethmoidal foramen, show the ophthalmic artery and its branches (arrows) coursing along the lower surface of the tumor (asterisk), in addition to slight enhancement of the lesion, ON: Optic nerve, Dashed arrow: Anterior ethmoidal artery.
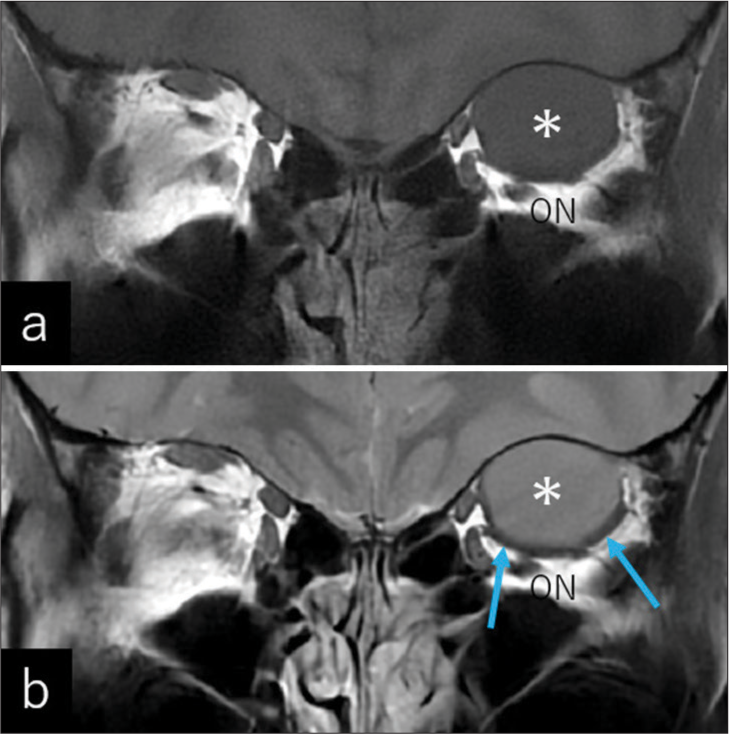
Figure 4:
Coronal (a) T1- and (b) T2-weighted magnetic resonance imaging show a well circumscribed tumor in the left orbit appearing homogeneously isointensity on both sequences (asterisk). On T2-weighted imaging, a hypointense, linear structure surrounding the inferior and medial surfaces of the tumor is noted (b, arrows). The left optic nerve shows a considerable downward displacement ON: Optic nerve.
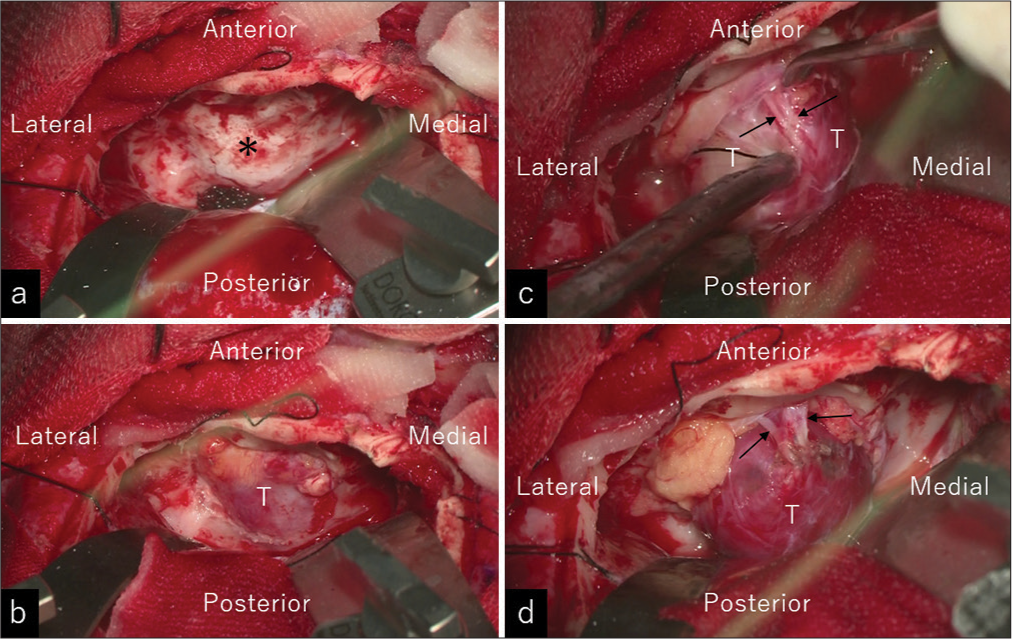
Figure 5:
Intraoperative photos showing the procedures in a step-by-step manner. (a) Epidural elevation of the frontal lobe exposed the left anterior fossa floor (asterisk). (b) Making a microsurgical osteotomy to the left floor revealed the offending tumor located immediately beneath the periorbita. (c) Reflection of the periorbita exposed the frontal nerve with the proximal segment intermingled with the tumor (arrows). (d) The tumor was circumferentially dissected from the surrounding tissues with the frontal nerve (arrows). T: Tumor.
Figure 6:
Photomicrographs of the resected specimens showing oval- or fusiform-shaped tumor cells arranged in palisading patterns (arrows) with fibrous interstitial tissues. The inset shows a magnified view. Cell atypia or mitotic figures are not found. Hematoxylin and eosin staining, ×40; inset, ×200.
Figure 7:
(a) Axial and (b) coronal T2-weighted magnetic resonance imaging performed on postoperative day 18 demonstrates restoration of the ocular position and distinguishable extraocular muscles on the left orbit. LM: Levator palpebral superioris muscle, SObM: Superior oblique muscle, SRM: Superior rectus muscle.
DISCUSSION
Orbital schwannomas most frequently affect middle-aged individuals and arise from the frontal nerves.[
Frontal nerve schwannomas can be approached through a superior orbitotomy, lateral orbitotomy, craniotomy, or their combinations.[
Schwannomas are benign peripheral nerve sheath tumors with common indolent growth. However, the present tumor showed unusually rapid growth over 2 years. Vahdani et al. reported an atypical orbital schwannoma in a 12-year-old patient without neurofibromatosis who presented with unusually rapid growth for 5 months. The tumor did not show any evidence of cystic degeneration, hemorrhage, or sarcomatous features.[
CONCLUSION
Frontal nerve schwannomas may grow rapidly under certain conditions. Periodic follow-up using MRI and timely resection is recommended when an asymptomatic orbital tumor, possibly a frontal nerve schwannoma, is detected in young patients.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agosti E, Saraceno G, Rampinelli E, Veiceschi P, Buffoli B, Rezzani R. Quantitative anatomic comparison of endoscopic transnasal and microsurgical transcranial approaches to the anterior cranial fossa. Oper Neurosurg (Hagerstown). 2022. 23: e256-66
2. Boustred AM. Endoscopic excision of a supraorbital schwannoma. Ophthalmic Plast Reconstr Surg. 2007. 23: 66-8
3. De Jong L, Demaerel P, Sciot R, Van Calenbergh F. A patient with swelling of the eyelid: Ancient schwannoma of the supraorbital nerve (2010:6b). Eur Radiol. 2010. 20: 2301-4
4. Haładaj R, Polguj M, Topol M. Anatomical variations of the supraorbital and supratrochlear nerves: Their intraorbital course and relation to the supraorbital margin. Med Sci Monit. 2019. 25: 5201-10
5. Hassler W, Schick U. The supraorbital approach--a minimally invasive approach to the superior orbit. Acta Neurochir (Wien). 2009. 151: 605-12
6. Hayashi Y, Watanabe T, Kita D, Hayashi Y, Takahira M, Hamada JI. Orbital cystic schwannoma originating from the frontal nerve. Case Rep Ophthalmol Med. 2012. 2012: 604574
7. Izumo T, Otsuka M, Okunaga T, Yoshioka T, Yokoyama H, Nagata I. Intraorbital schwannoma arising from the supraorbital nerve. No Shinkei Geka. 2012. 40: 167-71 [Article in Japanese]
8. Margalit N, Ezer H, Fliss DM, Naftaliev E, Nossek E, Kesler A. Orbital tumors treated using transcranial approaches: Surgical technique and neuroophthalmogical results in 41 patients. Neurosurg Focus. 2007. 23: E11
9. Mourier KL, Cophignon J, D’Hermies F, Clay C, Lot G, George B. Superolateral approach to orbital tumors. Minim Invasive Neurosurg. 1994. 37: 9-11
10. Natori Y, Rhoton AL. Transcranial approach to the orbit: Microsurgical anatomy. J Neurosurgery. 1994. 81: 78-86
11. Rhoton AL. The orbit. Neurosurgery. 2002. 51: S303-34
12. Sweeney AR, Gupta D, Keene CD, Cimino PJ, Chambers CB, Chang SH. Orbital peripheral nerve sheath tumors. Surv Ophthalmol. 2017. 62: 43-57
13. Taubenslag KJ, Nickols HH, Chelnis JG, Mawn LA. Hybrid neurofibroma/schwannoma of the supraorbital nerve: Clinicopathologic correlation of a rare tumor. Ophthalmic Plast Reconstr Surg. 2017. 33: S104-6
14. Tokugawa J, Nakao Y, Mori K, Maeda M. Orbital cystic neurinoma. Acta Neurochir (Wien). 2003. 145: 605-6
15. Vahdani K, Luthert PJ, Rose GE. Atypical, extremely rapid growth of pediatric orbital neurilemmoma. Ophthalmic Plast Reconstr Surg. 2021. 37: e164-7
16. Young KL, Beckman TJ, Cranstoun M, Sullivan TJ. Orbital schwannoma-management and clinical outcomes. Ophthalmic Plast Reconstr Surg. 2020. 36: 590-5
17. Young SM, Kim YD, Jeon GS, Woo KI. Orbital frontal nerve schwannoma-distinctive radiological features. Am J Ophthalmol. 2018. 186: 41-6