- Department of Neurosurgery, SUNY Upstate Medical University Hospital, Syracuse, New York, United States.
- Department of General Surgery, Lalezari Surgical, Los Angeles, California, United States.
Correspondence Address:
Shawn Singh Rai
Department of Neurosurgery, SUNY Upstate Medical University Hospital, Syracuse, New York, United States.
DOI:10.25259/SNI_197_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shawn Singh Rai, Carlos Rodrigo Goulart, Sepehr Lalezari, Michael Anthony Galgano, Satish Krishnamurthy. Dorsal migration of lumbar disc fragments causing cauda equina syndromes: A three case series and literature review. 04-Jul-2020;11:175
How to cite this URL: Shawn Singh Rai, Carlos Rodrigo Goulart, Sepehr Lalezari, Michael Anthony Galgano, Satish Krishnamurthy. Dorsal migration of lumbar disc fragments causing cauda equina syndromes: A three case series and literature review. 04-Jul-2020;11:175. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10115
Abstract
Background: Dorsal migration of an intervertebral lumbar disc fragment is exceedingly rare and may result in spinal cord or cauda equina compression. Radiologically, these lesions may be misdiagnosed as extradural masses or epidural hematomas.
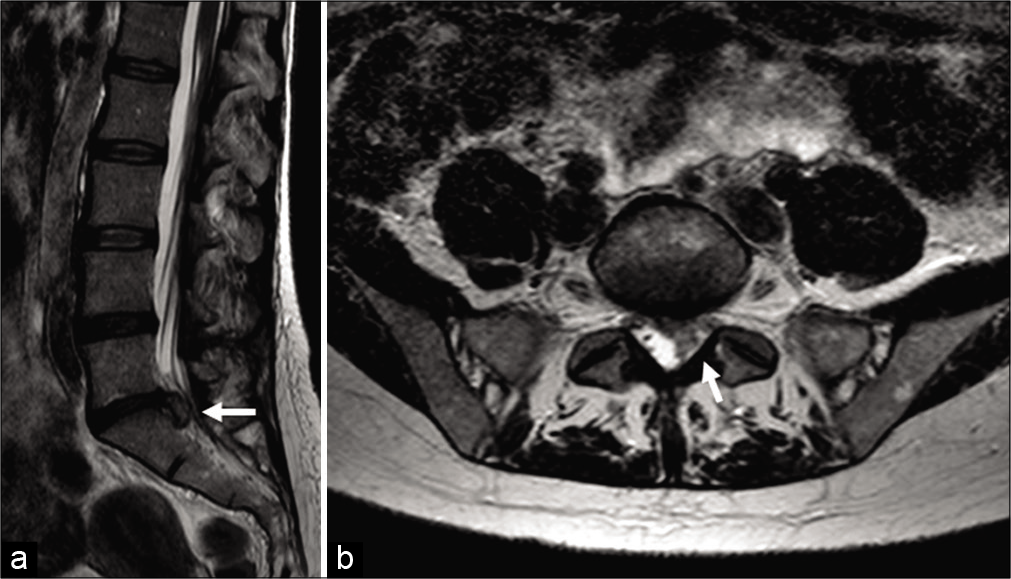
Case Description: We present three cases involving dorsal migration of sequestered lumbar disc fragments resulting in cauda equina syndromes. A 31-year-old male, 79-year-old female, and 47-year-old female presented with cauda equina syndromes attributed to the migration of dorsal sequestered lumbar disc fragments. Prompt surgical decompression resulted in adequate outcomes. Here, we review the three cases and the current literature for such lesions.
Conclusion: Dorsal migration of sequestered lumbar disc fragments is exceedingly rare, and these lesions are frequently misdiagnosed as extradural masses of other origin or epidural hematomas. Here and in the literature, prompt epidural decompression both confirmed the correct diagnosis and resulted in excellent outcomes.
Keywords: Cauda equina syndrome, Disc, Dorsal, Extruded, Lumbar
INTRODUCTION
Dorsal migration of lumbar intervertebral disc herniations resulting in acute cauda equina syndrome is exceedingly rare. Magnetic resonance imaging (MRI) findings can often be misdiagnosed as extradural masses of other origin or epidural hematomas. Here, we present three cases of dorsal migration of sequestered lumbar discs with posterior migration in patients presenting with cauda equina syndromes (CESs) resolved with posterior decompressions [
CASE PRESENTATION
Case 1
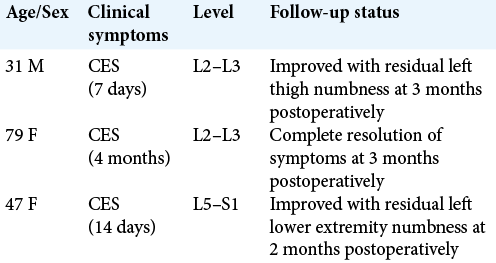
A 31-year-old male presented with 1 week of progressive low back pain, left lower extremity numbness, and weakness after lifting a heavy box. The neurological examination revealed an asymmetric CES, 3/5 weakness of the left lower extremity and numbness, and left more than right. The lumbar MRI revealed a posteriorly located extradural lesion at L2–L3 with compression of the thecal sac, thought to represent an extradural tumor [
Case 2
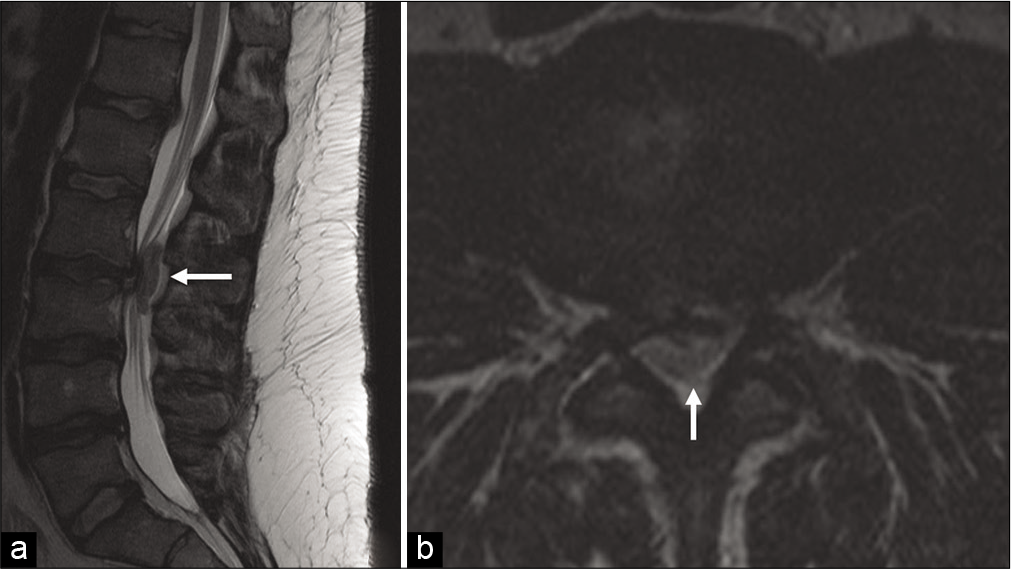
A 79-year-old female with a history of melanoma presented with the unsteady gait of 4 months duration with urinary urgency. Her only deficit was the weakness of the hip flexors and adductors bilaterally. The lumbar MRI scan demonstrated a dorsal epidural lesion at the L2–3 level with thecal sac compression [
Case 3
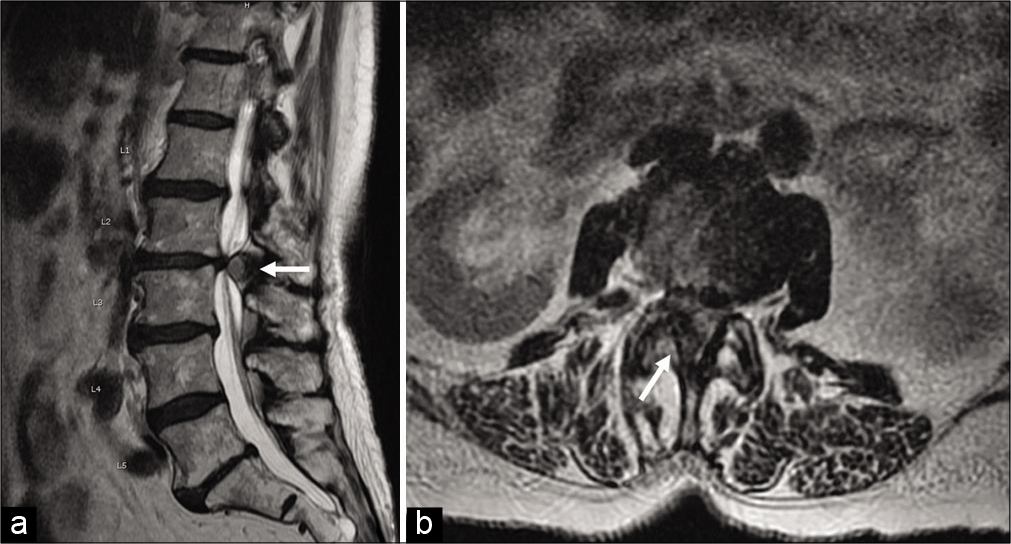
A 47-year-old female presented with low back pain and left lower extremity radiculopathy for 2 weeks duration. On examination, she had gastrocnemius weakness, left lower extremity numbness, urinary urgency, and an abnormal gait. The MRI demonstrated a left lateral epidural lesion dorsal to the S1 nerve root with compression of the thecal sac [
Figure 3:
Preoperative sagittal T2-weighted magnetic resonance imaging (MRI) without contrast (a) and axial T2-weighted MRI scan without contrast (b) demonstrate an extradural T2 hypointense lesion in the left dorsal epidural space at the level of L5-S1 with compression of the thecal sac and left S1 nerve root (white arrow).
DISCUSSION
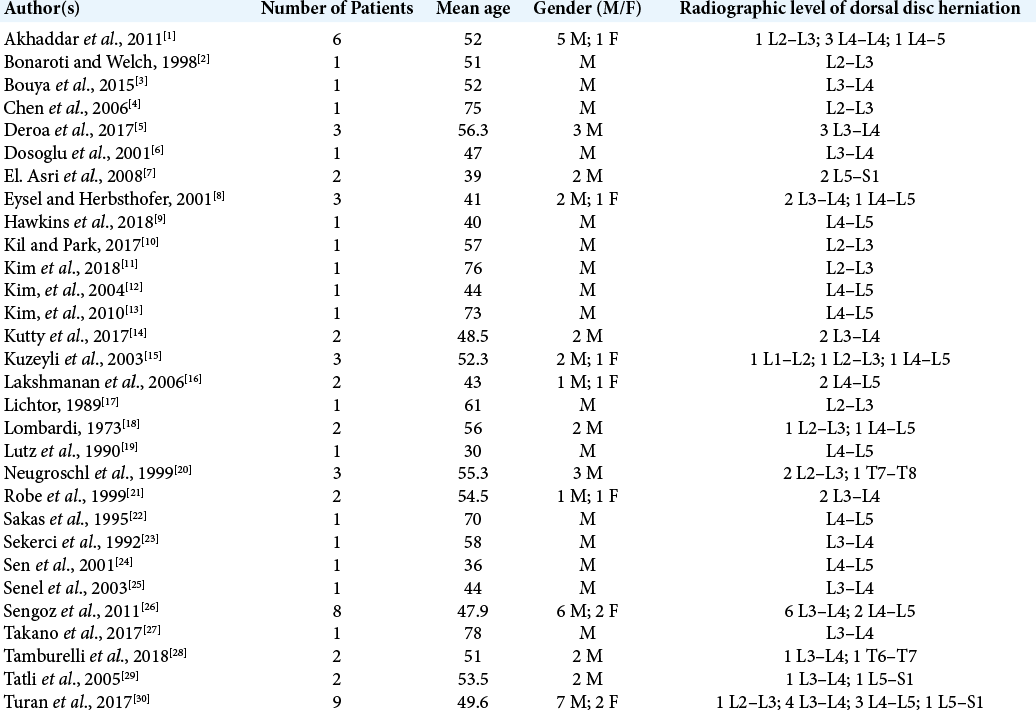
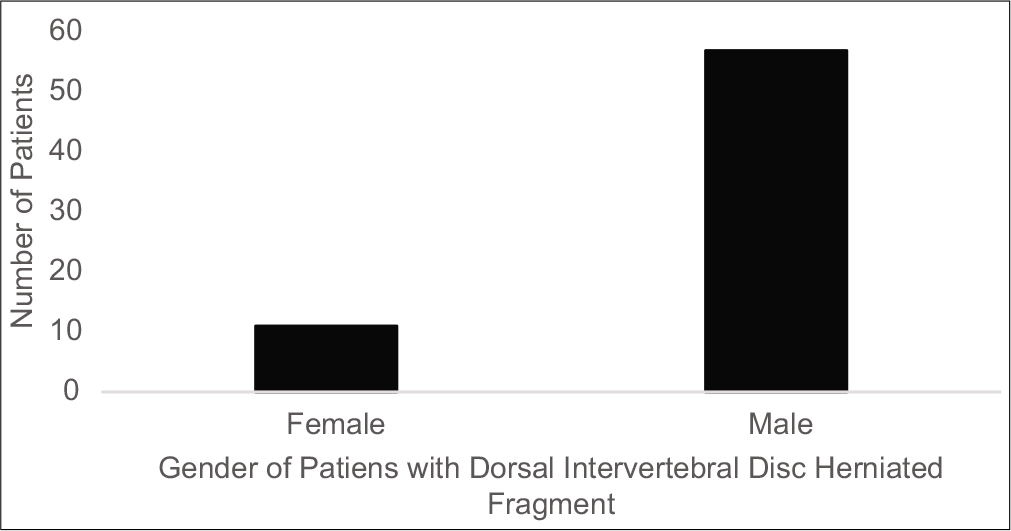
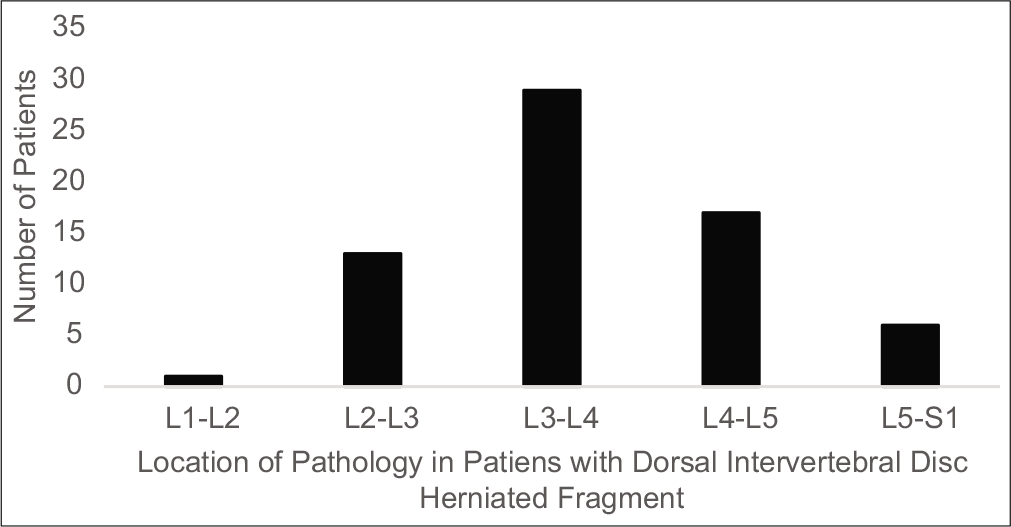
A review of the literature reveals 67 cases of dorsal disc fragment sequestrations, including our three cases.[
Our hypothesis is that a traumatic injury is responsible for the posterior migration of a herniated disc fragment in the lumbar spine. Patients with dorsally migrated lumbar disc fragments most commonly present with cauda equina syndrome (CES), paraparesis, or radiculopathy. The most important diagnostic study for assessing dorsally migrated lumbar discs is the MRI scan. The lack of continuity of the disc fragment with the intervertebral disc space and the unusual location of the migrated disc fragment can mislead the treating physician and favor the consideration of other differential diagnoses such as epidural tumor or hematoma. Establishing the correct diagnosis with surgical intervention is critical as it also simultaneously provides adequate neural decompression.
CONCLUSION
Dorsal sequestration of lumbar intervertebral discs is rare and may be readily confirmed on MRI studies. As these patients typically present with acute CES or paraparesis, timely decompression is warranted to both confirm the disc pathology and effect neurological recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akhaddar A, El-Asri A, Boucetta M. Posterior epidural migration of a lumbar disc fragment: A series of 6 Cases. J Neurosurg Spine. 2011. 15: 117-28
2. Bonaroti EA, Welch WC. Posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. Clinical and magnetic resonance imaging evaluation. Spine (Phila Pa 1976). 1998. 23: 378-81
3. Bouya SM, Djoubairou BO, Okacha N, Gazzaz M, El Mostarchid B. Posterior epidural migration of lumbar intervertebral fragment: Case report. Pan Afr Med J. 2015. 21: 80-
4. Chen CY, Chuang YL, Yao MS, Chiu WT, Chen CL, Chan WP. Posterior epidural migration of a sequestrated lumbar disk fragment: MR imaging findings. AJNR Am J Neuroradiol. 2006. 27: 1592-4
5. Deora H, Prabhuraj AR, Pruthi N. Posterior epidural migration of lumbar disc: Will the real disc please stand up?. Surg Neurol Int. 2017. 8: 302-
6. Dosoglu M, Is M, Gezen F, Ziyal MI. Posterior epidural migration of a lumbar disc fragment causing cauda equina syndrome: Case report and review of the relevant literature. Eur Spine J. 2001. 10: 348-51
7. El Asri AC, Naama O, Akhaddar A, Gazzaz M, Belhachmi A, El Mostarchid B. Posterior epidural migration of lumbar disk fragments: Report of two cases and review of the literature. Surg Neurol. 2008. 70: 668-71
8. Eysel P, Herbsthofer B. Dorsal compression of the epidural cord due to free sequestral lumbar prolapse. Diagnostic problems in magnetic resonance imaging and computed tomography. Arch Orthop Trauma Surg. 2001. 121: 238-40
9. Hawkins JC, Natkha VP, Seibly J. Posterior epidural migration of a lumbar disc herniation causing cauda equina syndrome: A case report. Cureus. 2018. 10: e2739-
10. Kil JS, Park JT. Posterior epidural herniation of a lumbar disk fragment at L2-3 that mimicked an epidural hematoma. Korean J Spine. 2017. 14: 115-7
11. Kim H, Kwon BS, Park JW, Lee HJ, Lee JW, Lee EK. Posterior epidural migration of a lumbar intervertebral disc fragment resembling a spinal tumor: A case report. Ann Rehabil Med. 2018. 42: 621-5
12. Kim JH, Kong MH, Lee SK, Song KY. A case of posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. J Korean Neurosurg Soc. 2004. 35: 442-4
13. Kim JS, Lee SH, Arbatti NJ. Dorsal extradural lumbar disc herniation causing cauda equina syndrome: A case report and review of literature. J Korean Neurosurg Soc. 2010. 47: 217-20
14. Kutty RK, Sunilkumar BS, Peethambaran A, Jain SK, Kumar S. PEMLIF-a tale of two stories. J Spine Surg. 2017. 3: 498-503
15. Kuzeyli K, Cakir E, Usul H, Baykal S, Yazar U, Karaarslan G. Posterior epidural migration of lumbar disc fragments: Report of three cases. Spine (Phila Pa 1976). 2003. 28: E64-7
16. Lakshmanan P, Ahuja S, Lyons K, Howes J, Davies PR. Sequestrated lumbar intervertebral disc in the posterior epidural space: A report on two cases and review of the literature. Spine J. 2006. 6: 583-6
17. Lichtor T. Posterior epidural migration of extruded lumbar disk. Surg Neurol. 1989. 32: 311-2
18. Lombardi V. Lumbar spinal block by posterior rotation of anulus fibrosus. Case report. J Neurosurg. 1973. 39: 642-7
19. Lutz JD, Smith RR, Jones HM. CT myelography of a fragment of a lumbar disk sequestered posterior to the thecal sac. AJNR Am J Neuroradiol. 1990. 11: 610-1
20. Neugroschl C, Kehrli P, Gigaud M, Ragragui O, Maitrot D, Manelfe C. Posterior extradural migration of extruded thoracic and lumbar disc fragments: Role of MRI. Neuroradiology. 1999. 41: 630-5
21. Robe P, Martin D, Lenelle J, Stevenaert A. Posterior epidural migration of sequestered lumbar disc fragments. Report of two cases. J Neurosurg. 1999. 90: 264-6
22. Sakas DE, Farrell MA, Young S, Toland J. Posterior thecal lumbar disc herniation mimicking synovial cyst. Neuroradiology. 1995. 37: 192-4
23. Sekerci Z, Ildan F, Yuksel M, Gul B, Kilic C. Cauda equina compression due to posterior epidural migration of extruded lumbar disk. Neurosurg Rev. 1992. 15: 311-3
24. Sen O, Aydm M, Erdogan B, Yildirim T, Caner H. Cauda equina syndrome caused by posterior epidural migration of an extruded lumbar disc fragment. Turk Neurosurg. 2001. 11: 108-10
25. Şenel A, Çokluk C, Çelik F. Posterior epidural migration of extruded lumbar disc mimicking epidural mass: Case report. Turk Neurosurg. 2003. 13: 115-7
26. Sengoz A, Kotil K, Tasdemiroglu E. Posterior epidural migration of herniated lumbar disc fragment. J Neurosurg Spine. 2011. 14: 313-7
27. Takano M, Hikata T, Nishimura S, Kamata M. Discography aids definitive diagnosis of posterior epidural migration of lumbar disc fragments: Case report and literature review. BMC Musculoskelet Disord. 2017. 18: 151-
28. Tamburrelli FC, Perna A, Oliva MS, Giannelli I, Genitiempo M. Unusual posterior epidural migration of intervertebral herniated disc: A report of two cases. Malays Orthop J. 2018. 12: 47-9
29. Tatli M, Guzel A, Ceviz A, Karadag O. Posterior epidural migration of sequestered lumbar disc fragment causing cauda equina syndrome. Br J Neurosurg. 2005. 19: 257-9
30. Turan Y, Yilmaz T, Gocmez C, Ozevren H, Kemaloglu S, Teke M. Posterior epidural migration of a sequestered lumbar intervertebral disc fragment. Turk Neurosurg. 2017. 27: 85-94