- Department of Spine Service, Indian Spinal Injuries Center, New Delhi, India.
DOI:10.25259/SNI_350_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jeevan Kumar Sharma, Kalyan Kumar Varma Kalidindi, Gururaj Sangondimath, Abhinandan Reddy Mallepally, Nandan Marathe, Harvinder Singh Chhabra. Clinicoradiological outcomes of Goel and Harms fixation for atlantoaxial instability: An institutional experience. 11-Jul-2020;11:189
How to cite this URL: Jeevan Kumar Sharma, Kalyan Kumar Varma Kalidindi, Gururaj Sangondimath, Abhinandan Reddy Mallepally, Nandan Marathe, Harvinder Singh Chhabra. Clinicoradiological outcomes of Goel and Harms fixation for atlantoaxial instability: An institutional experience. 11-Jul-2020;11:189. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10131
Abstract
Background: Few studies have reported on the long-term outcomes of Goel and Harms C1-C2 fusions in the Asian population.
Methods: This was a retrospective analysis of 53 patients undergoing Goel and Harms fixation (2010 –2018). Clinical outcomes were assessed utilizing the neck disability index (NDI), Japanese Orthopedic Association (JOA) score, and visual analog scale (VAS). Outcomes were then correlated with fusion rates (using dynamic X-rays), atlanto-dens interval (ADI), and space available for cord (SAC) data.
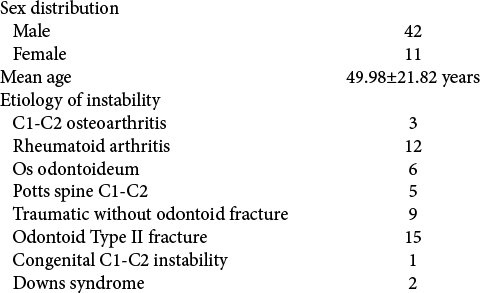
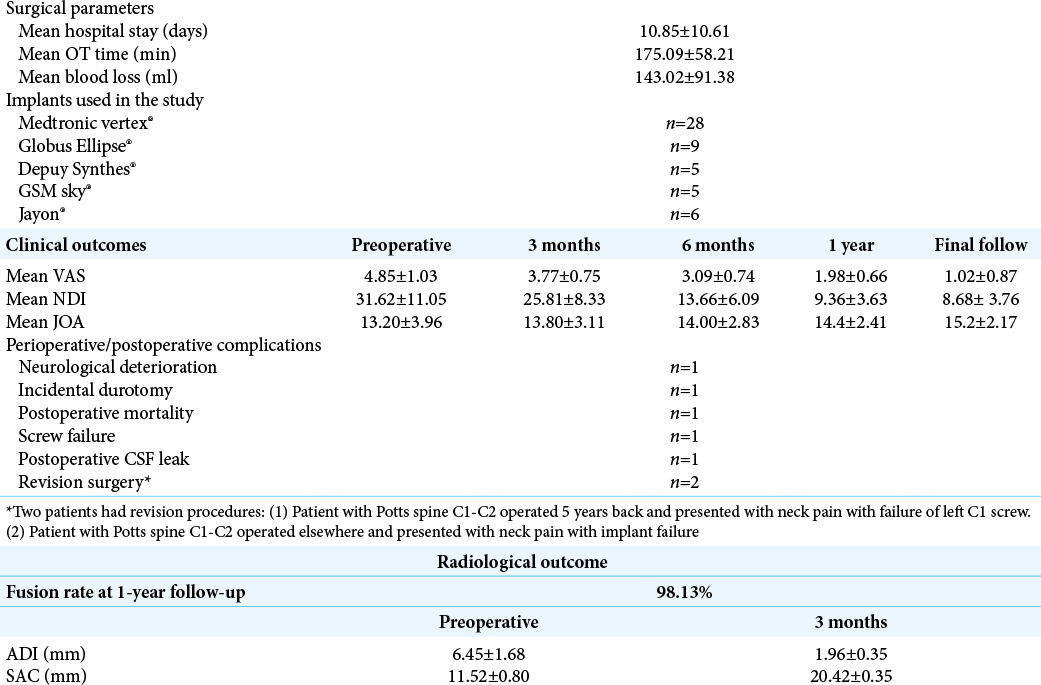
Results: The study’s 53 patients averaged 49.98 years of age and included 42 males and 11 females. The mean preoperative versus postoperative scores on multiple outcome measures showed NDI 31.62 ± 11.05 versus decreased to 8.68 ± 3.76 post, mean JOA score (e.g., in 41 patients with myelopathy) improved from 13.20 ± 3.96 to 15.2 ± 2.17, and the mean VAS decreased from 4.85 ± 1.03 to 1.02 ± 0.87 and showed restoration of the ADI (1.96 ± 0.35 mm) and SAC (20.42 ± 0.35 mm). A 98.13% rate of C1-C2 fusion was achieved at 12 postoperative months.
Conclusion: Goel and Harms technique for C1-C2 fusion resulted in both good clinical and radiological outcomes.
Keywords: Atlantoaxial, Cervical spine, Goel’s technique, Harms, Instability
INTRODUCTION
There are various techniques available for atlantoaxial (A-A) arthrodesis.[
MATERIALS AND METHODS
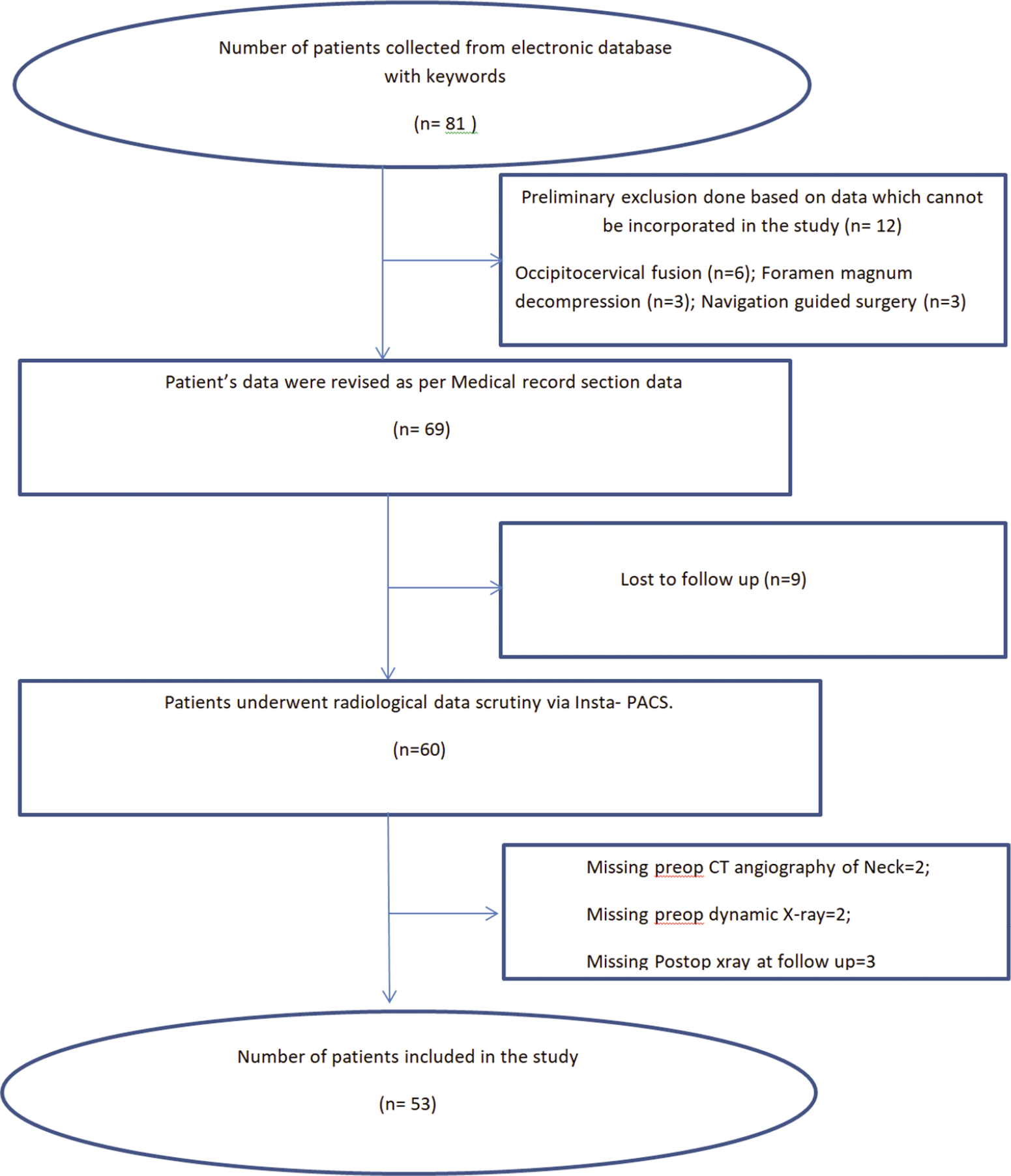
We performed a retrospective analysis of clinical and radiological data for 57 patients who underwent Goel and Harms C1-C2 fusions for various pathologies (2010–2018) [
Surgical protocol followed in our institute
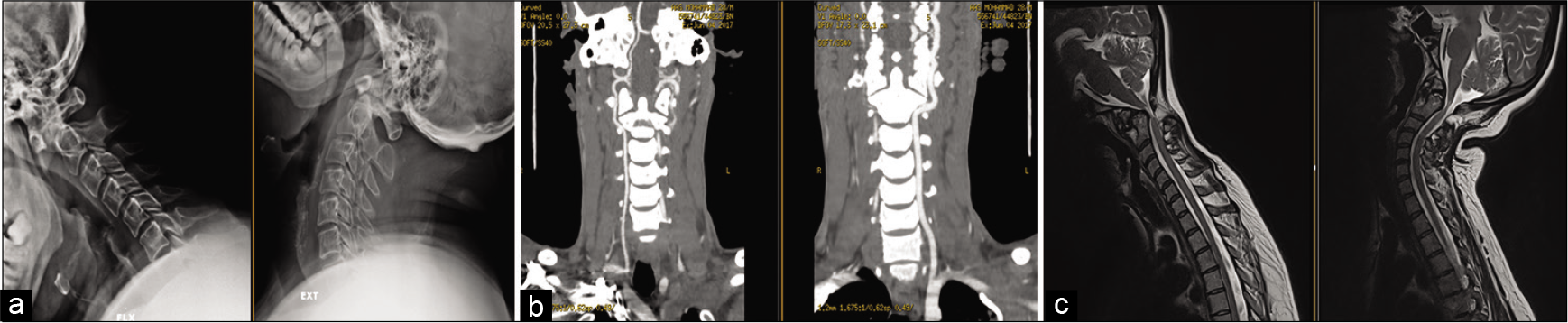
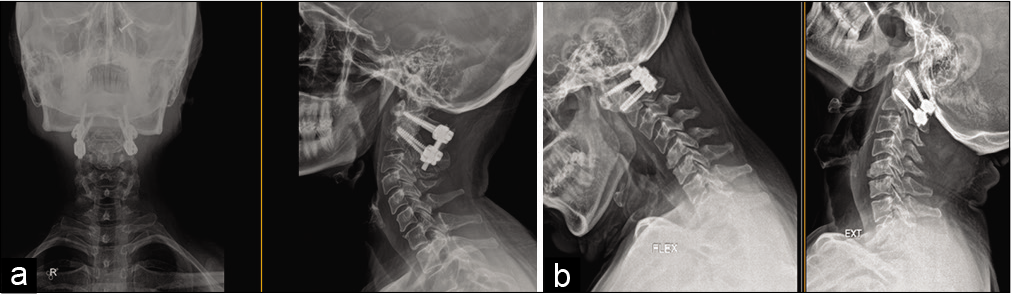
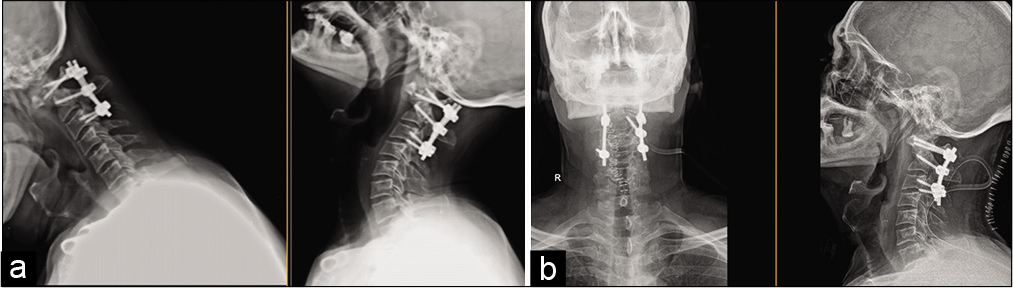
Dynamic X-rays were used to assess the instability of C1-C2. The diameter of the C2 pedicle was assessed on preoperative CT scan and the CTA documented whether or not there was a high riding vertebral artery. C2 pedicle/pars screws and C1 lateral mass screws were used for fixation, and rods were connected to the screws. Clinical outcomes and dynamic X-rays were performed at 3rd months, 6th months, and then yearly.
Follow-up duration
The mean follow-up duration was 48.90 ± 24.78 months (12–96 months).
RESULTS
Clinical findings
For 53 patients undergoing various surgical procedures, 43 patients had signs of myelopathy. The mean operative time was 175.09 ± 58.21 min, the average blood loss was 143.02 ± 91.38 ml, and the average length of stay was10.85 ± 10.61 days [
Outcome scores
Postoperatively, the improvement was seen on the JOA, VAS, and NDI scores, while radiological improvement was noted (e.g., X-rays and/or MR) on the ADI and SAC measures [
Complications
There were six complications; a patient with Os- odontoideum deteriorated postoperatively from AIS-E to AIS-C but improved to AIS-D 3 months later, two sustained intraoperative or postoperative CSF leaks, two patients had to undergo revision surgery [
DISCUSSION
Gallie, Brooks, and Jenkins used bone grafts for C1-C2 fusion with sublaminar wires to provide A-A stability.[
CONCLUSION
The Goel and Harms technique was a safe and effective technique for treating A-A (C1-C2) instability in the Asian population.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978. 60: 279-84
2. Gallie WE. Skeletal traction in the treatment of fractures and dislocations of the cervical spine. Ann Surg. 1937. 106: 770-6
3. Goel A, Desai KI, Mazumdar DP. Atlantoaxial fixation using plate and screw method: A report of 160 treated patients. Neurosurgery. 2002. 51: 1351-7
4. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001. 26: 2467-71
5. Huang DG, Hao DJ, He BR, Wu QN, Liu TJ, Wang XD. Posterior atlantoaxial fixation: A review of all techniques. Spine J. 2015. 15: 2271-81
6. Isik HS, Sandal E, Cagli S. Clinical outcomes of posterior C1 and C2 screw-rod fixation for atlantoaxial instability. Turk Neurosurg. 2018. 28: 602-9
7. Rajinda P, Towiwat S, Chirappapha P. Comparison of outcomes after atlantoaxial fusion with C1 lateral mass-C2 pedicle screws and C1-C2 transarticular screws. Eur Spine J. 2017. 26: 1064-72
8. Zheng Y, Hao D, Wang B, He B, Hu H, Zhang H. Clinical outcome of posterior C1-C2 pedicle screw fixation and fusion for atlantoaxial instability: A retrospective study of 86 patients. J Clin Neurosci. 2016. 32: 47-50