- Department of Surgery, Federal Medical Center Owo, Owo, Ondo state, Nigeria,
- Department of Neurological Surgery, University College Hospital, University of Ibadan, Ibadan, Oyo state, Nigeria.
Correspondence Address:
Toyin Ayofe Oyemolade
Department of Surgery, Federal Medical Center Owo, Owo, Ondo state, Nigeria,
DOI:10.25259/SNI_559_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toyin Ayofe Oyemolade1, Amos Olufemi Adeleye2, Oluwakemi C. Ogunyileka1, Folawemimo M. Arogundade1, Ayodele J. Olusola1, Oluwadamilola O. Aribisala1. Determinants of discharge against medical advice from a rural neurosurgical service in a developing country: A prospective observational study. 12-Sep-2020;11:290
How to cite this URL: Toyin Ayofe Oyemolade1, Amos Olufemi Adeleye2, Oluwakemi C. Ogunyileka1, Folawemimo M. Arogundade1, Ayodele J. Olusola1, Oluwadamilola O. Aribisala1. Determinants of discharge against medical advice from a rural neurosurgical service in a developing country: A prospective observational study. 12-Sep-2020;11:290. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10250
Abstract
Background: In low-resource regions of the world, discharge against medical advice (DAMA) is one empiric contributory factor to poor in-hospital outcome that is not often mentioned. This study aims to investigate the determinants of DAMA from a rural neurosurgical service in a developing country.
Methods: This was a prospective observational study of all patients who discharged against medical advice in our service between November 2018 and October 2019.
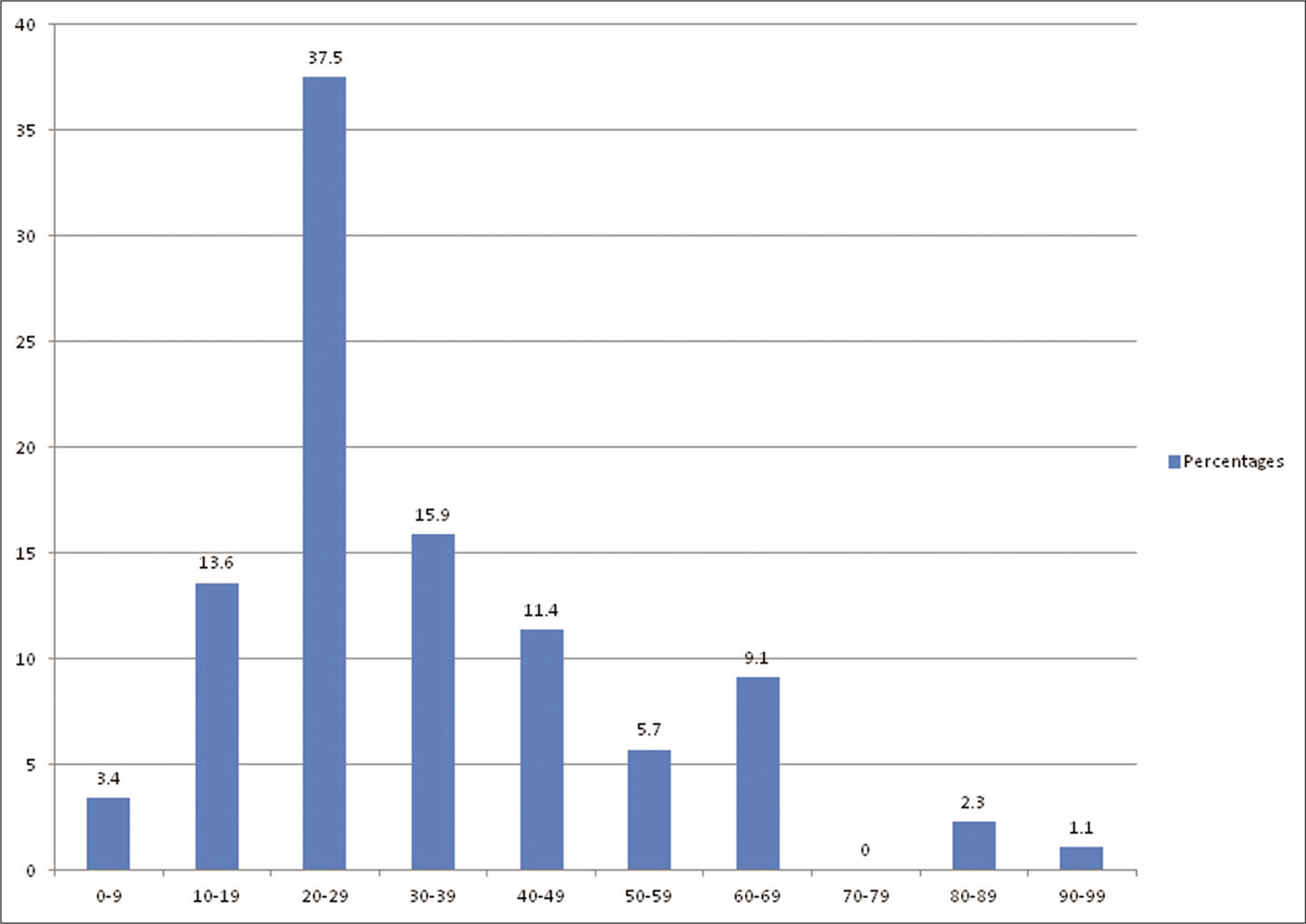
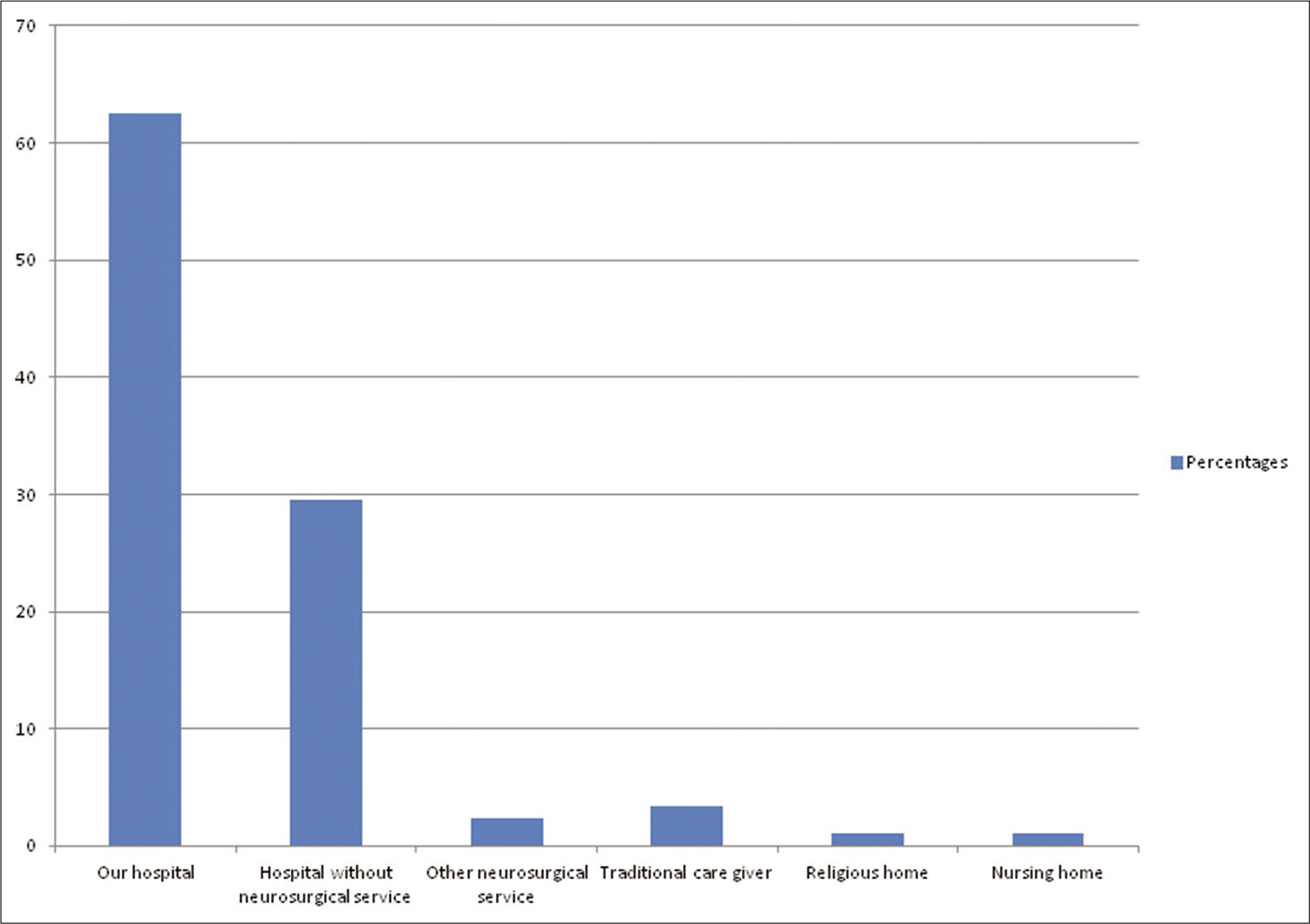
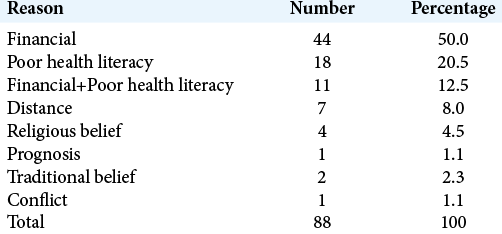
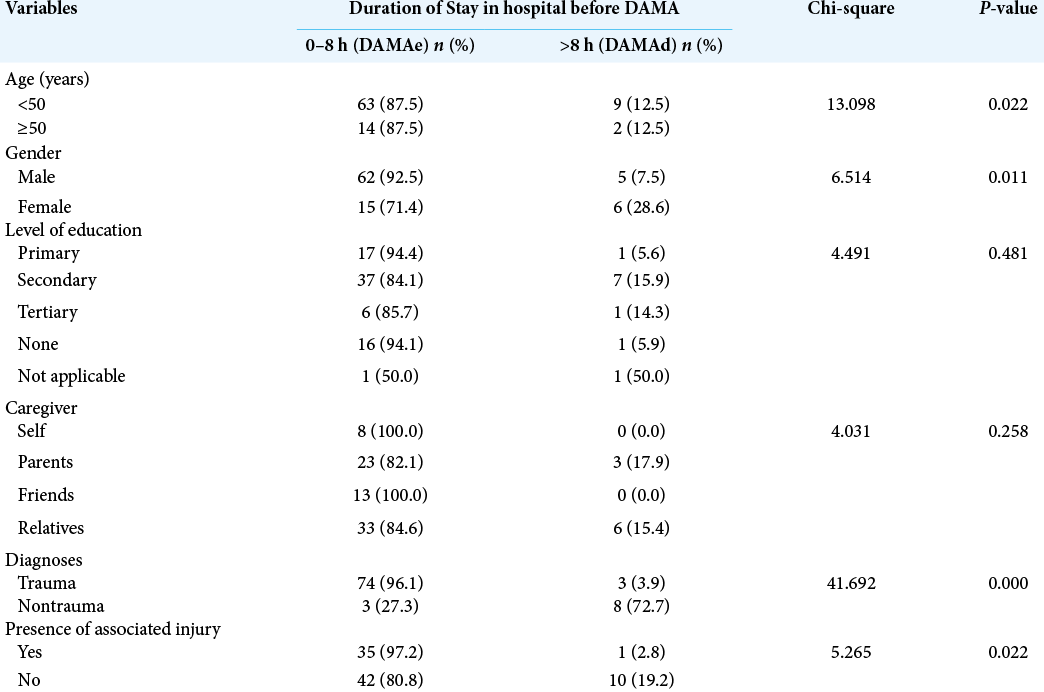
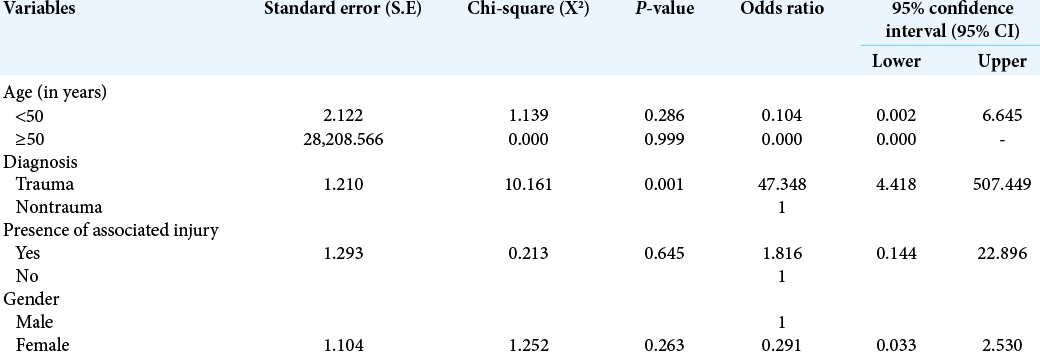
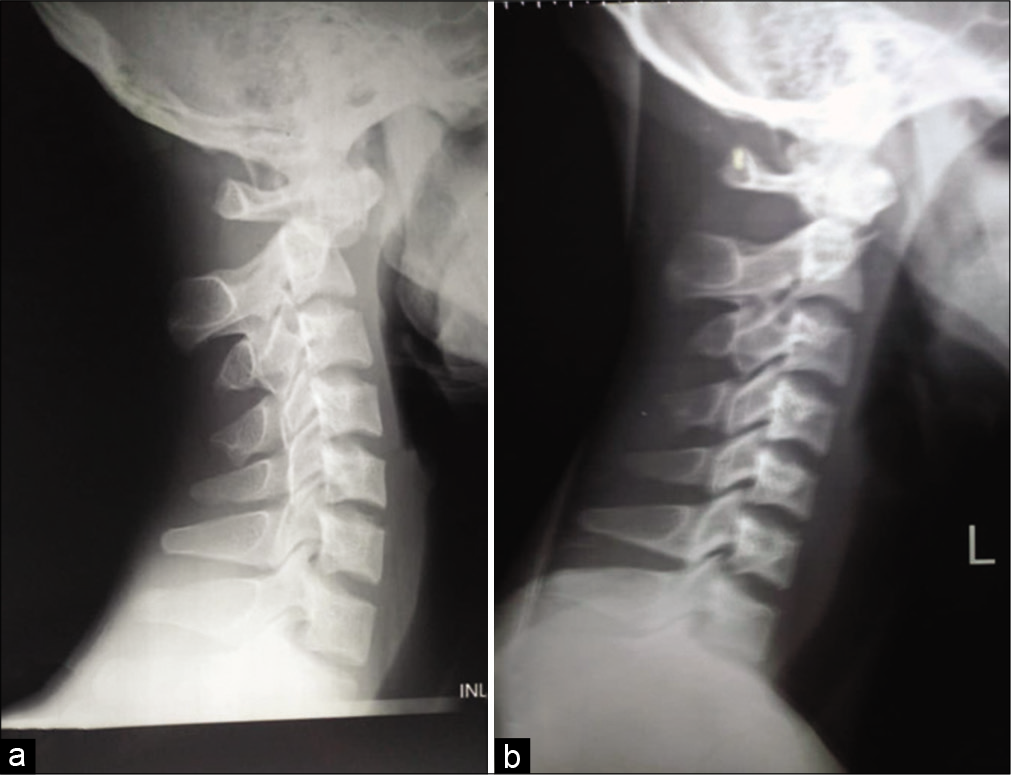
Results: There were 88 patients, 67 (76.1%) males, in the study, (M:F = 3.2:1), representing 17.4% of our patient population in the study period. The peak incidence was in the 20–29 years age group which accounted for 37.5% of the cases. About 55% of the patients presented directly to our center; 31.8% were referred from other hospitals, while 3.4% came from traditional caregivers and 1.1% from religious homes. Head injury was the most common indication for presentation (76.1% of the cases). The duration of hospital stay ranged from 2 h to 14 days. Majority of the patients (87.5%) left the hospital within 8 h of presentation. The reason for DAMA was financial constraints in 50% of cases, inadequate health literacy in 20.5%, financial constraints and poor health literacy together in 12.5%, religious misgivings in 4.5%, and traditional belief in 2.3%. Neurotrauma was predictive of early DAMA (P = 0.001).
Conclusion: The rate of DAMA was high in our study. Financial constraints with other socioeconomic limitations were the most common causes of DAMA in our environment.
Keywords: Determinants, Developing country, Discharge against medical advice, Rural neurosurgery
INTRODUCTION
Discharge against medical advice (DAMA) is an issue generating some significant concerns in health systems globally.[
Several causes of DAMA have been reported, including financial difficulties/lack of health insurance; dissatisfaction with the care received, and/or, the hospital environment; lack of access to skilled and qualified physicians, lack of advanced medical services; and presumed unsatisfactory results from treatment, and presumed unduly prolonged in-hospital stay of patients.[
The previous studies on DAMA in our country as well as most studies from other parts of the world were in mixed patients’ populations in the medical, psychiatric, or surgical/ orthopedic wards.[
MATERIALS AND METHODS
This was a cross-sectional study of all prospective patients who discharged against medical advice in our neurosurgical service over a 12-month period from November 2018 to October 2019. Our neurosurgical practice is a newly inaugurated one in a tertiary level hospital in a rural part of Nigeria, a large country in sub-Saharan Africa. We collected data on the demographic characteristics of the patients, the diagnosis, duration of symptoms, duration of stay in our service before the DAMA, reasons for the DAMA, plus representation in the hospital after the DAMA, as well as the reasons for the representation and the interval between the DAMA and the repeat presentation. Early DAMA (DAMAe) was defined as DAMA within 8 h of admission and late DAMA (DAMAd) as DAMA after 8 h.[
RESULTS
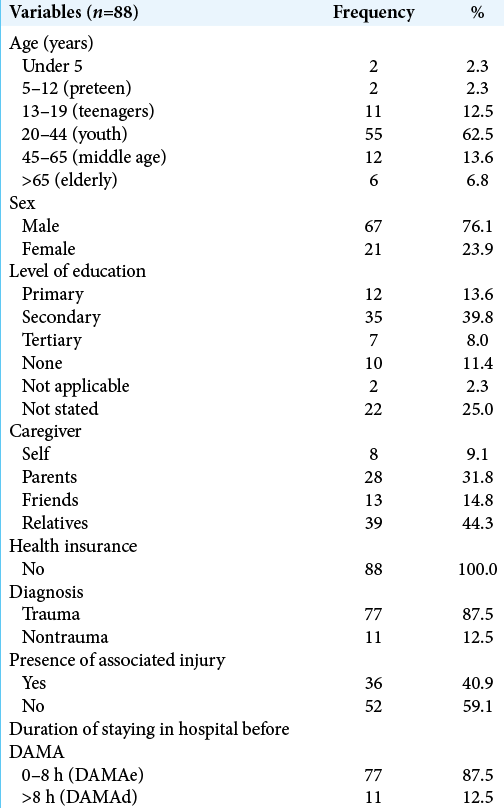
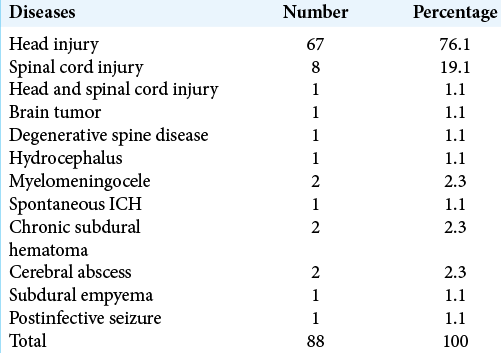
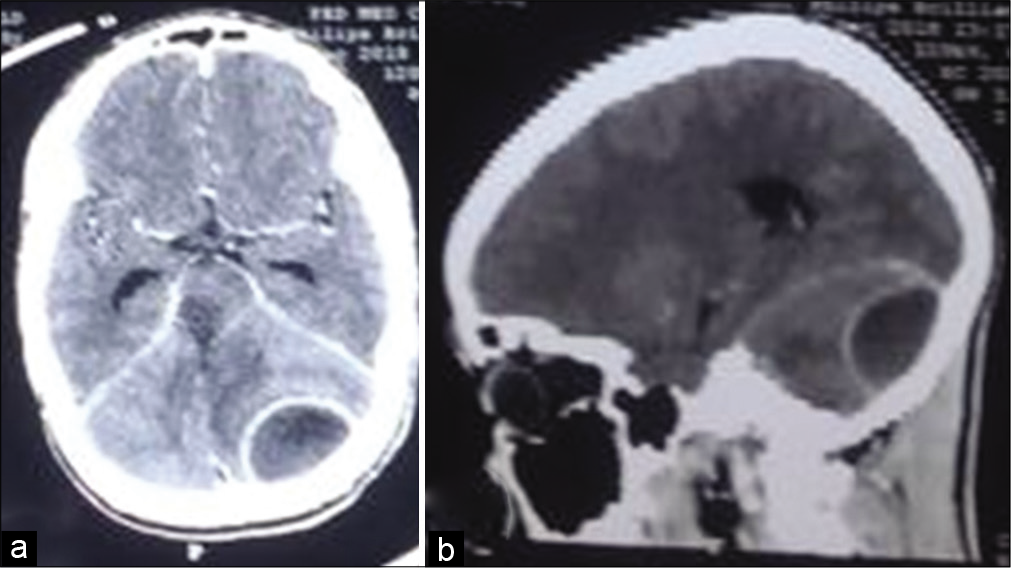
There were 88 patients in the study, 67 (76.1%) males and 21 females (M:F = 3.2:1), representing 17.4% of the 506 cases seen in our neurosurgical practice during the study period [
The median duration of hospital stay in this cohort of patients that discharged AMA was 6.5 h (range = 2 h–14 days). The DAMA was early, within 8 h of admission (DAMAe) in 87.5%, and late, after 8 h (DAMAd) in 12.5%. The reason for DAMA was low income in 50% of cases, low health literacy in 20.5%, low income and health literacy together in 12.5%, long distance in 8.0%, and conflicting religious and traditional beliefs in 4.5% and 2.3%, respectively [
DISCUSSION
DAMA is a well-recognized concern in in-patient health care globally with significant attendant negative economic and health consequences.[
The predominance of male gender in this study is in agreement with trends in other studies locally and abroad.[
Other reasons for DAMA identified in this study were poor medical insight and the need for proximity to relatives/ caregivers in some of the patients. About 33% of the patients discharged against medical advice because they felt that they were well while 8% left because of their felt need for proximity to relatives/caregivers despite no access to neurosurgical service at these destinations. These factors have all been documented in the literature.[
Notably in this study, none of the patients discharged against medical advice because of dissatisfaction with the care received, or the medical staff, or the hospital environment. This finding is contrary to those of other reports which found a proportion of their patients leaving the hospital against medical advice because of dissatisfaction with the medical staff or the hospital environment.[
DAMA because of religious and traditional beliefs was a rather interesting finding in this study. Although the percentage was low in this study (6.8%) despite the prevalence of these two factors in our environment, this finding highlights the challenge these beliefs pose to health care in poor societies with high level of poor health literacy, particularly in the developing world.
More than four-fifth of our patients (87.5%) in this study were of the early DAMA status, leaving the hospital within 8 h of presentation. This figure is significantly higher than the 25.7% reported by Lakhotia et al.[
DAMA is one of the leading causes of hospital readmission.[
The negative impact of the privately funded model of payment for health care on the outcome of that care, especially as obtains in the low resource settings of many sub-Saharan Africa has been documented. The absence of health insurance covers in all our patients, and the finding of financial constraints as the most common reason for DAMA lends credence to the need to do away with this model of health-care financing. We advocate alternative health-care financing models particularly a functional and sustainable health insurance scheme in other to maximize the health resources available in these settings.[
CONCLUSION
The rate of DAMA was high in our study possibly due to the expensive nature of neurosurgical in-hospital evaluation and treatment in a resource-constrained developing country milieu of privately funded health-care financing. Low income and level of health literacy were the most common causes of DAMA in this neurosurgical patient population. A diagnosis of neurotrauma significantly predicts early DAMA in this study. Functional health insurance scheme with a wide coverage will go a long way in reducing the incidence of DAMA and improving overall health indices in developing countries like ours.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Commentary
This is a simple but elegant study. The authors show convincing evidence that financial constraints is the most important factor in refusal of continuation of treatment for DAMA in the developing nation under study, and that this can result in increased morbidity and mortality. But if one were to consider that ability to pay (financial constraints) was the most important factor, as indeed this paper attempts to prove and argue, then one would expect a more equal proportion of males and females, even taking into account that head injuries occur more frequently in men than in women. In fact, head injuries are more common in men than women because of men’s aggressiveness and more frequent belligerence. So I tend to believe that aggressiveness of males, especially in head injured patients, could still be an important fact to rival, or even surpass, financial reasons in these cases of DAMA. The author(s) did not find this to be the case.
Another interesting fact is that most of us in the US tend to believe that financial constraint is a problem that one only finds in America — and not the rest of the world — because most of the world, we are told, already has socialized medicine and wonderful “free” health care. In fact, in the US everyone that goes to an emergency facility (virtually every hospital) must be treated, regardless of ability to pay. Moreover, the poor have Medicaid; and those 65 or older (the elderly) have Medicare. No one goes without treatment. Hardest hit with catastrophic hospital bills are those of the middle class who have to buy their own medical insurance or chose not to have it because health insurance admittedly is expensive. But virtually no one, despite what one has been led to believe by the American mainstream or globalist media, goes without medical care.
So, I was particularly shocked a couple of years back when a group of our colleagues from China presented a study of patients who were treated with functional neurosurgery for seizure disorders and other maladies. They have had excellent results. Then it was mentioned in passing that it was a shame that the operations could not be performed more widespread because of inability to pay. “How can this be?” I wrote in a comment published in SNI. The authors wrote back in reply that free health care in China today is only for the cadre. Who is this cadre? The communist party intelligentsia, we must presume. The authors would not explain any further and the dialogue abruptly ended.
So, once again I am a bit perplexed that this is happening elsewhere in a developing country, presumably in sub- Saharan Africa because “a global lack of health insurance necessitating out-of-pocket payment for health-care expenses.” The authors do not explain why the DAMA rate in their patients was 17.4% but “previous reports from our country was .0002–5.7%.” Why this discrepancy? What national or regional policy can account for this significant difference? Let me play devil’s advocate for a moment to ask another question worth raising:
Was there any difference in outcome between similar patients who remained in the hospital and continued medical treatment in the hospital versus the DAMA patients in this study? This is a very important question because if there is no significant difference in outcome, informed DAMA patients were correct to exercise their personal autonomy, regardless of reason for leaving, and may have saved themselves and their families considerable out-of-pocket expenses as well as freed themselves from a heavy financial burden. In fact, “Thirty-three percent of the patients discharged against medical advice felt they were well.” It would have been interesting how many of these patients were found among those who later deteriorated because of DAMA.
Indeed, the authors did find several patients who did not do well and had catastrophic results presumably because of their refusing proper care because of DAMA. Nevertheless, a set of patient controls that could have been compared to the DAMA patients would have resulted in a better study, even without randomization, which of course would have been impossible in this study.
Personal autonomy, we as physicians must recognize, is an important aspect of medical care regardless of cause, as important as informed consent. Presumably, availability of social and economic assistance, as can be provided by the community, could help persuade some of these DAMA patients to accept medical in this study, but it would have been interesting if there had been a control group of patients for comparison of outcome among DAMA and non-DAMA patients.
Miguel A. Faria, MD
hfaria@windstream.net
References
1. Adefemi SA, Adeleke IT, Gara P, Ghaney OO, Omokanye SA, Yusuf AM. The rate, reasons and predictors of hospital discharge against medical advice among inpatients of a tertiary health facility in North-Central Nigeria. Am J Health Res. 2015. 3: 11-6
2. Adeleye AO, Fasunla JA, Young PH. Skull base surgery in a large, resource-poor, developing country with few neurosurgeons: Prospects, challenges, and needs. World Neurosurg. 2012. 78: 35-43
3. Adeleye AO, Jite IE, Smith OA. A tale of two acute extradural hematomas. Surg Neurol Int. 2016. 7: 54
4. Adeleye AO, Ogun MI. Clinical epidemiology of head injury from road-traffic trauma in a developing country in the current Era. Front Neurol. 2017. 8: 695
5. Adem A, Abebe A, Abduraham M. Pattern of surgical admissions to Tikur Anbessa Hospital, Addis Ababa, Ethiopia. East Cent Afr J Surg. 2001. 6: 31-4
6. Adeolu AA, Malomo AO, Shokunbi MT, Komolafe EO, Abiona TC. Etiology of head injuries in Southwestern Nigeria: A public health perspective. Internet J Epidemiol. 2004. 2: 1-4
7. Akiode O, Musa AA, Shonubi AM, Salami BA, Oyelekan AA. Trends of discharges against medical advice in a suburban surgical practice in Nigeria. Trop Doct. 2005. 35: 51-2
8. Al Ayed I. What makes patients leave against medical advice?. J Taibah Univ Med Sci. 2009. 4: 16-22
9. Alebiosu CO, Raimi TH. A study of hospital patients discharged against medical advice in the Olabisi Onabanjo University Teaching Hospital, Sagamu. Niger Med Pract. 2004. 40: 33-6
10. Alfandre DJ. I’m going home: Discharges against medical advice. Mayo Clin Proc. 2009. 84: 255-60
11. Aliyu ZY. Discharge against medical advice: Sociodemographic, clinical and financial perspectives. Int J Clin Pract. 2002. 56: 325-7
12. Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002. 167: 633-7
13. Ashrafi E, Nobakht S, Keykaleh MS, Kakemam E, Hasanpoor E, Sokhanvar M. Discharge against medical advice (DAMA): Causes and predictors. Electron Physician. 2017. 9: 4563-70
14. Berger JT. Discharge against medical advice: Ethical considerations and professional obligations. J Hosp Med. 2008. 3: 403-8
15. Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003. 118: 358-65
16. Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003. 139: 907-15
17. Ding R, Jung JJ, Kirsch TD, Levy F, McCarthy ML. Uncompleted emergency department care: Patients who leave against medical advice. Acad Emerg Med. 2007. 14: 870-6
18. Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000. 9: 1156-63
19. Duñó R, Pousa E, Sans J, Tolosa C, Ruiz A. Discharge against medical advice at a general hospital in Catalonia. Gen Hosp Psychiatry. 2003. 25: 46-50
20. El Malek VA, Alexander S, Al Anezi F. Discharge against medical advice among children admitted into pediatric wards at Al-Jahra Hospital, Kuwait. Kuwait Med J. 2014. 46: 28-31
21. Emejulu JK, Osuafor C, Ogbuagu CN. Audit of the demographic patterns of neurosurgical cases in a tertiary health institution: The need to relate service delivery to disease profile in dwindling resources and manpower shortage. Afr J Neurol Sci. 2009. 28: 11-21
22. Emejulu JK. Epidemiological patterns of head injury in a newly established neurosurgical service: One-year prospective study. Afr J Med Med Sci. 2008. 37: 383-8
23. Eze B, Agu K, Nwosu J. Discharge against medical advice at a tertiary center in southeastern Nigeria: Sociodemographic and clinical dimensions. Patient Int. 2010. 2: 27-31
24. Fadare JO, Babatunde OA, Olanrewaju T, Busari O. Discharge against medical advice: Experience from a rural Nigerian hospital. Ann Niger Med. 2013. 7: 60-5
25. Hasan O, Samad MA, Khan H, Sarfraz M, Noordin S, Ahmad T. Leaving against medical advice from in-patients departments rate, reasons and predicting risk factors for re-visiting hospital retrospective cohort from a tertiary care hospital. Int J Health Policy Manag. 2019. 8: 474-9
26. Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice?. CMAJ. 2003. 168: 417-20
27. Ibekwe RC, Muoneke VU, Nnebe-Agumadu UH, Amadife MA. Factors influencincing discharge against medical advice among paediatric patients in Abakaliki, Southeastern Nigeria. J Trop Pediatr. 2009. 55: 39-41
28. Jeremiah J, O’Sullivan P, Stein MD. Who leaves against medical advice?. J Gen Intern Med. 1995. 10: 403-5
29. Jimoh BM, Anthonia OC, Chinwe I, Oluwafemi A, Ganiyu A, Haroun A. Prospective evaluation of cases of discharge against medical advice in Abuja, Nigeria. Sci World J. 2015. 2015: 314817
30. Kemp A, Sibert J. Childhood accidents: Epidemiology, trends, and prevention. J Accid Emerg Med. 1997. 14: 316-20
31. Lakhotia AN, Sodan A, Dube M, Telang K, Jain R, Athale S. Discharge against medical advice from neurology wards of a teaching hospital: A prospective observational study. Clin Epidemiol Glob Health. 2019. 7: 115-20
32. Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care?. J Health Soc Behav. 2002. 43: 296-306
33. Naderi S, Acerra JR, Bailey K, Mukherji P, Taraphdar T, Mukherjee T. Patients in a private hospital in India leave the emergency department against medical advice for financial reasons. Int J Emerg Med. 2014. 7: 13
34. Ohanaka EC. Discharge against medical advice. Trop Doct. 2002. 32: 149-51
35. Okoromah CN, Egri-Okwaji MT. Profile of and control measures for paediatric discharges against medical advice. Niger Postgrad Med J. 2004. 11: 21-5
36. Onyira EJ, Mgbekem M, Edet OB. Factors associated with discharge against medical advice among patients in University of Calabar Teaching Hospital Calabar (UCTH). Glob J Pure Appl Sci. 2016. 22: 91-100
37. Onyiriuka AN. Discharge of hospitalized under-fives against medical advice in Benin City, Nigeria. Niger J Clin Pract. 2007. 10: 200-4
38. Orimolade EA, Adegbehingbe OO, Oginni LM, Asuquo JE, Esan O. Reasons why trauma patients request for discharge against medical advice in Wesley Guild Hospital Ilesha. East Cent Afr J Surg. 2013. 18: 71-5
39. Querques J, Kontos N, Freudenreich O. Discharges against medical advice. JAMA. 2014. 311: 1807-8
40. Quinlan WC, Majoros N. Patients leaving against medical advice: Assessing the liability risk. J Healthc Risk Manag. 1993. 13: 19-22
41. Rabiu TB, Komolafe EO. Neurosurgery in rural Nigeria: A prospective study. J Neurosci Rural Pract. 2016. 7: 485-8
42. Roodpeyma S, Hoseyni SA. Discharge of children from hospital against medical advice. World J Pediatr. 2010. 6: 353-6
43. Saitz R, Ghali WA, Moskowitz MA. The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med. 2000. 15: 103-7
44. Seaborn MH, Osmun WE. Discharges against medical advice: A community hospital’s experience. Can J Rural Med. 2004. 9: 148-53
45. Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health. 1991. 81: 212-5
46. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012. 125: 594-602
47. Street RL, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: Why some patients are more involved than others. Med Care. 2005. 43: 960-9
48. Udosen AM, Glen E, Ogbudu S, Nkposong E. Incidence of leaving against medical advice (LAMA) among patients admitted at the accident and emergency unit of the University of Calabar Teaching Hospital, Calabar, Nigeria. Niger J Clin Pract. 2006. 9: 120-3
49. Valevski A, Zalsman G, Tsafrir S, Lipschitz-Elhawi R, Weizman A, Shohat T. Rate of readmission and mortality risks of schizophrenia patients who were discharged against medical advice. Eur Psychiatry. 2012. 27: 496-9
50. Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med. 1998. 13: 568-71
51. Withersty DJ. Patient responsibility and the AMA discharge: A one-year follow-up study. Am J Psychiatry. 1977. 134: 1442-4