- Department of Neurosurgery, Hospital de Especialidades No. 71, Instituto Mexicano del Seguro Social, Torreón, Coahuila, México,
- Department of Pathology, Hospital de Especialidades No. 71, Instituto Mexicano del Seguro Social, Torreón, Coahuila, México,
- Graduate School of Neural and Behavioural Sciences, International Max Planck Research School, Tuebingen University, Tuebingen, Germany,
- Department of Neurosurgery, Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social, Ciudad de México, México.
Correspondence Address:
Bayron A. Sandoval-Bonilla
Department of Neurosurgery, Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social, Ciudad de México, México.
DOI:10.25259/SNI_684_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: María F. De la Cerda-Vargas1, José Antonio Candelas Rangel1, Elizabeth Meza Mata2, Araceli Ramírez-Cárdenas3, Bayron A. Sandoval-Bonilla4. 99mTc-UBI 29-41 bone SPECT/CT scan in craniofacial Actinomyces israelii: Misdiagnosis of cranial bone tumor – A case report. 16-Dec-2020;11:442
How to cite this URL: María F. De la Cerda-Vargas1, José Antonio Candelas Rangel1, Elizabeth Meza Mata2, Araceli Ramírez-Cárdenas3, Bayron A. Sandoval-Bonilla4. 99mTc-UBI 29-41 bone SPECT/CT scan in craniofacial Actinomyces israelii: Misdiagnosis of cranial bone tumor – A case report. 16-Dec-2020;11:442. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10459
Abstract
Background: Actinomycosis is a rare infection, frequently misdiagnosed as a neoplasia. This chronic and granulomatous disease is caused by Actinomyces israelii species. Cervicofacial actinomycosis occurs in 60% of cases and the diagnosis is commonly made by histopathology study.
Case Description: We report a case of fronto-orbital osteomyelitis initially misdiagnosed as a cranial bone meningioma, but later proved to be a case of actinomycosis. 99mTechnetium (99mTc) three-phase bone single-photon emission computed tomography/computed tomography (SPECT/CT) and 99mTc-ubiquicidin (UBI) 29-41 bone SPECT/CT scans were performed to corroborate the control of the infection.
Conclusion: Craniofacial actinomycosis is the most common presentation of actinomycosis. However, it continues to be a rare and difficult disease to diagnose and is often confused with a neoplastic process. The 99mTc-UBI 29-41 bone SPECT/CT scan could be an auxiliary noninvasive diagnostic alternative and a follow-up method for these patients.
Keywords: Actinomyces, Craniofacial, Osteomyelitis
INTRODUCTION
Actinomycosis is a rare invasive bacterial disease that causes a chronic, suppurative, granulomatous infection. Actinomyces israelii are Gram-positive, anaerobic, filamentous bacilli that have low pathogenicity and normally colonize the mouth and gastrointestinal tract.[
Given that actinomycosis is a purulent bacterial infection, radiotracers which detect bacteria colonization have diagnosis potential. Recent reports have showed that 99mtechnetium-ubiquicidin (99mTc-UBI) 29-41 bone single-photon emission computed tomography/computed tomography (SPECT/CT) scan can be a useful diagnostic study for pyogenic vertebral osteomyelitis.[
The diagnosis of actinomycosis is made by a positive culture or the visualization of necrosis with sulfur granules and Gram-positive filamentous bacteria in the histopathology study.[
CASE DESCRIPTION
A 57-year-old woman from Torreon Coahuila was referred in November 2015 for sudden increase in volume of the right fronto-orbital region. The patient reported a contusion in the right frontal region 1 month before and was underwent treatment with metronidazole but not improvement was observed [
Relevant antecedents included cardiothoracic surgery at 4 years old to treat an unspecified cyanotic heart condition and in 1992 plastic surgery established the diagnosis of “craniofacial dysostosis” and a fronto-orbital advancement, including osteotomies and bone cranial remodeling with methyl methacrylate.
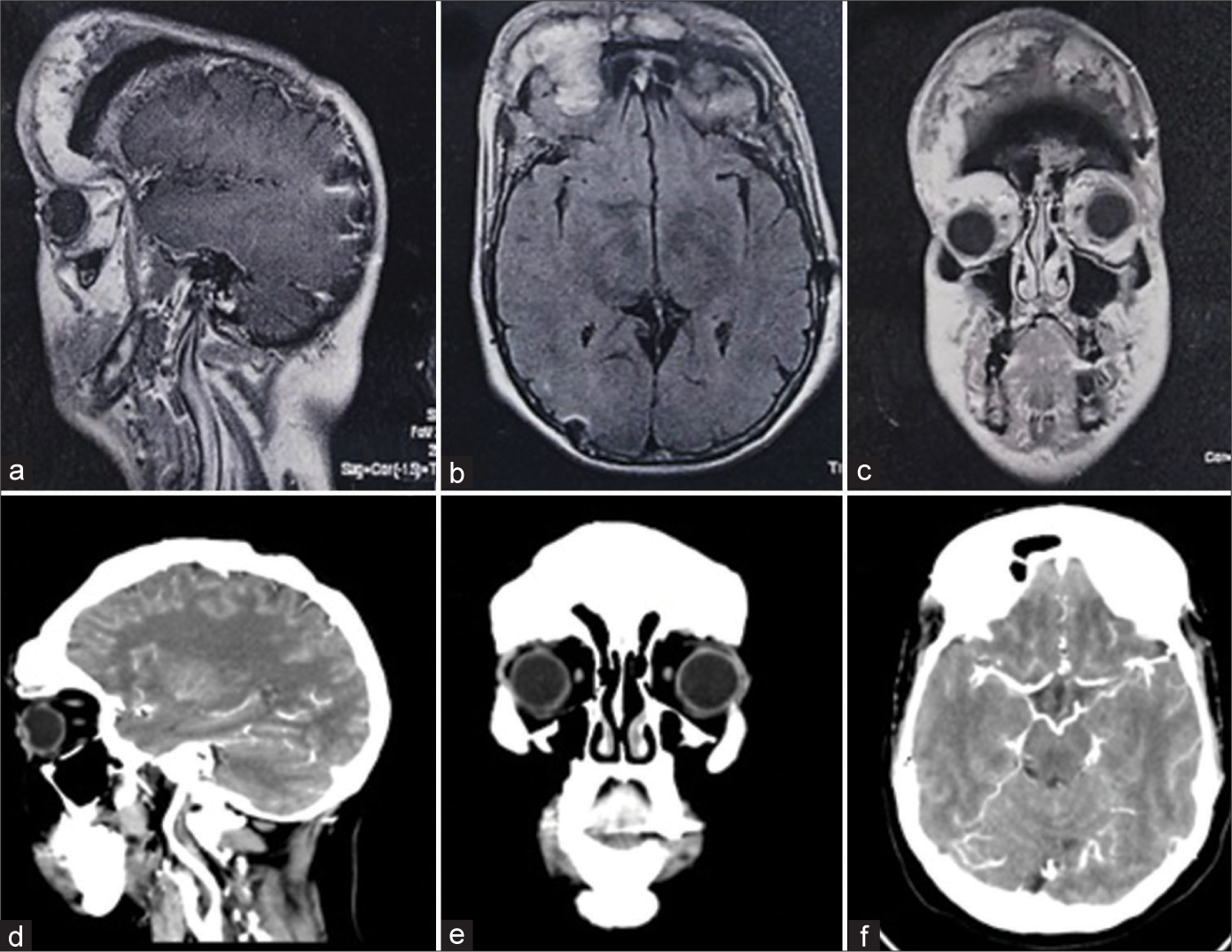
In January 2016, a magnetic resonance imaging study reported heterogeneous enhancement mass in the bilateral fronto-orbital region [
Figure 2:
(a-c) (Upper quadrants) Presurgical gadolinium-enhanced T1-weighted magnetic resonance imaging showing heterogeneous enhancement mass in the bilateral fronto-orbital region predominantly on the right side, we can see a hypodensity in relation to methyl methacrylate. (d-f) (Lower quadrants) Computed tomography scan control 6 months after the medical treatment with resolution of the deformity.
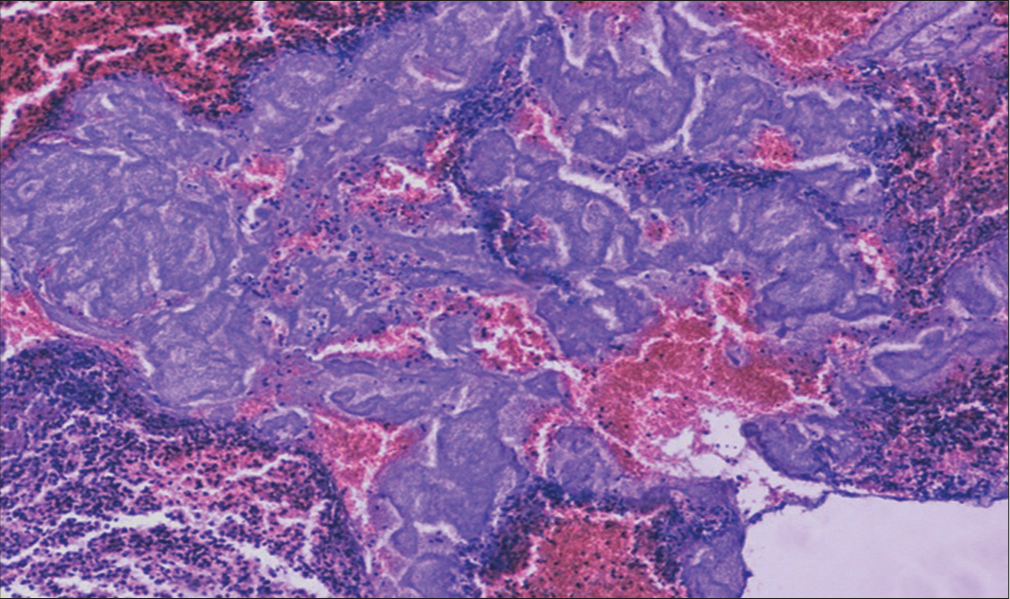
The culture was reported negative, but tissue staining with hematoxylin and eosin revealed bacilli compatible with A.israelii was isolated in the tumor tissue by histopathological study by staining for hematoxylin and eosin [
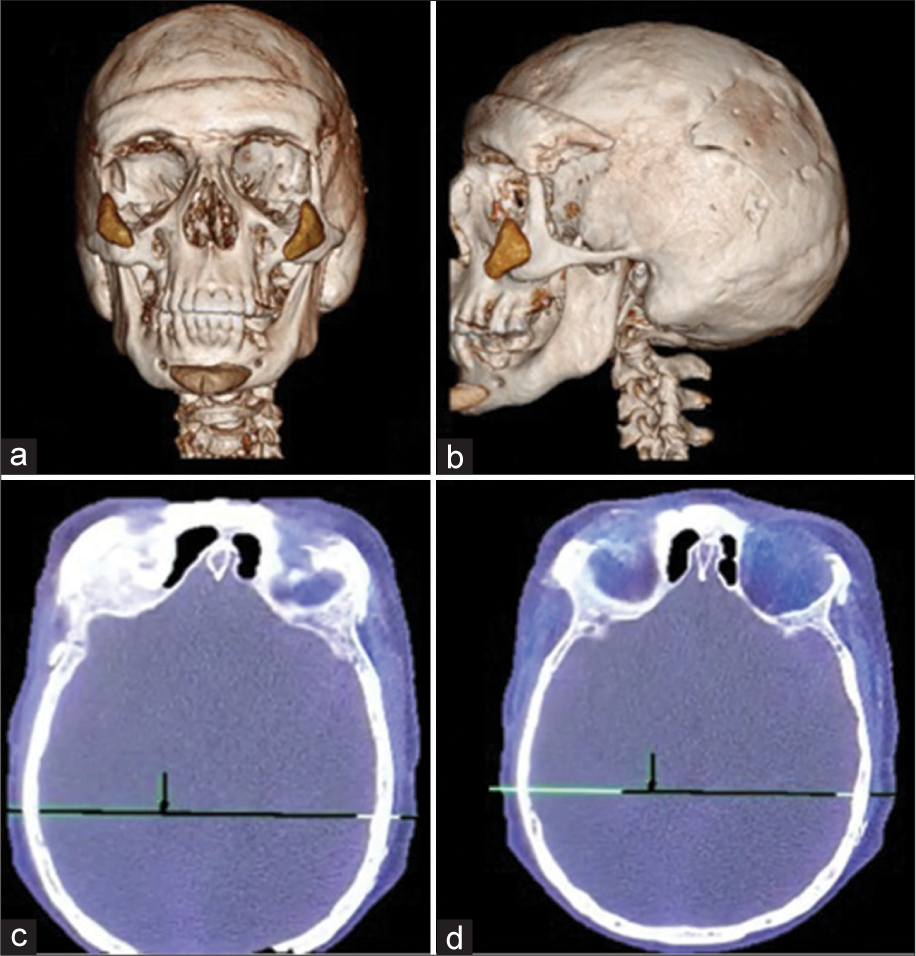
Figure 4:
(a and b) 3D computed tomography (CT) scan showing silicone implants in the chin and zygomatic bone, a supraorbital methyl methacrylate bar and plates in the bilateral parietal region (upper quadrants). (c and d) (Lower quadrants): 99mtechnetiumUbiquicidin (29–41)/three-phase bone single-photon emission computed tomography/CT scan control 3 years after the last surgical intervention showing diffuse uptake of the radiotracer, suggestive of an inflammatory process, an active infectious process is ruled out.
DISCUSSION
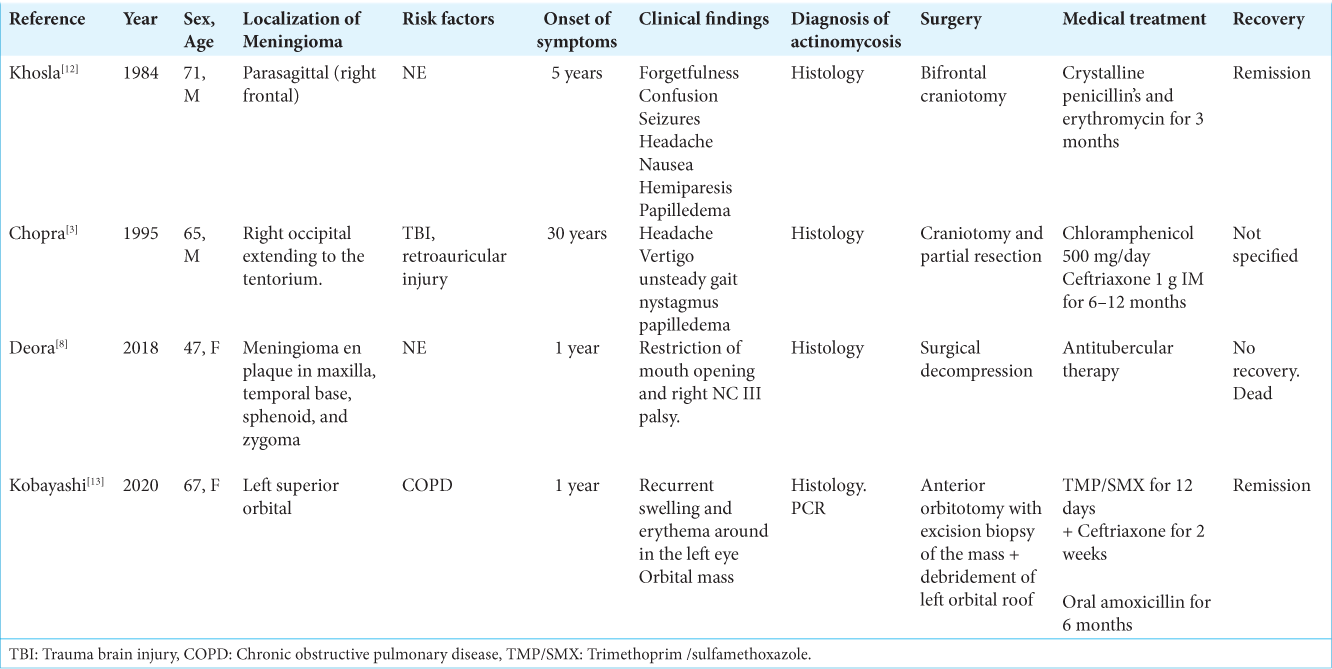
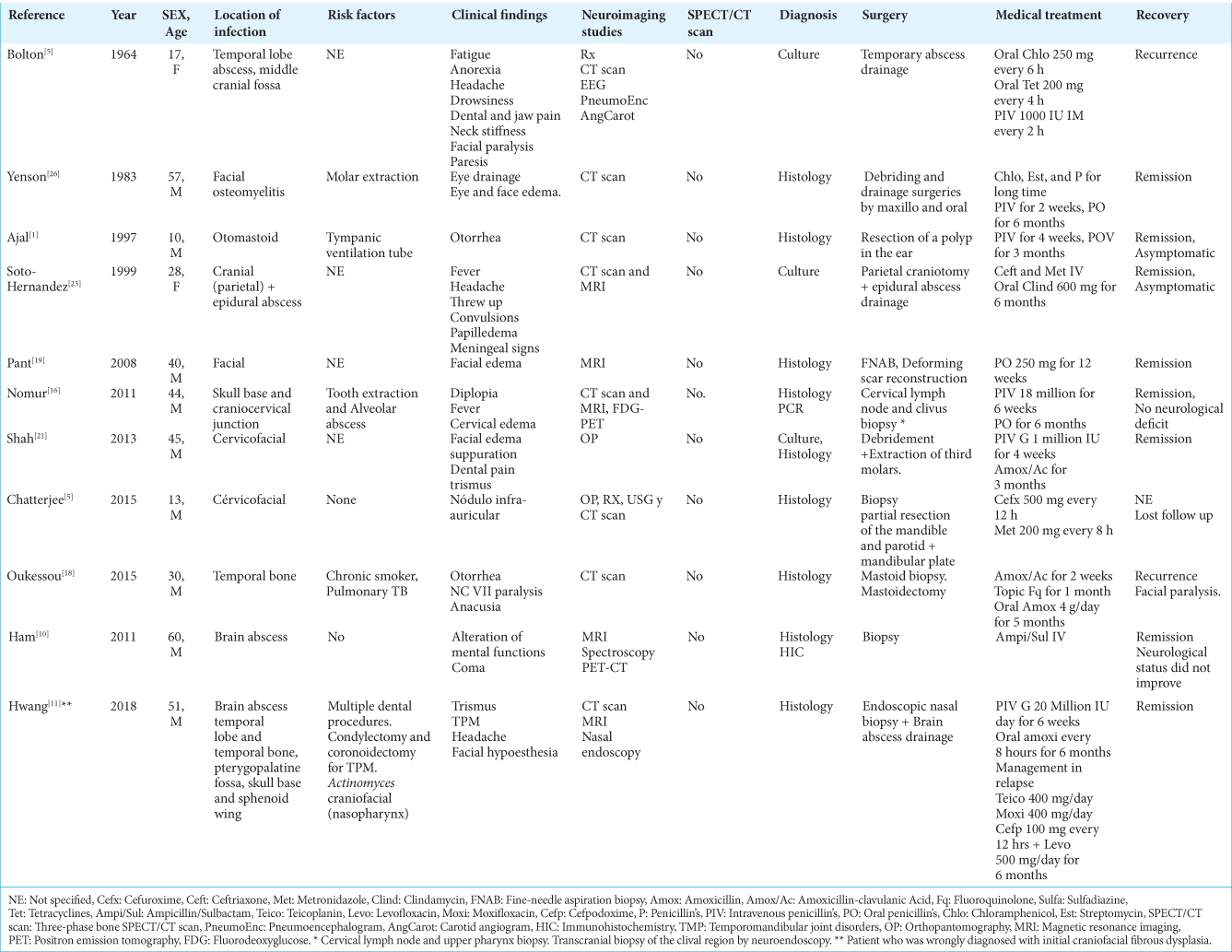
Cervicofacial[
A positive uptake with 18F-fluorodeoxyglucose positron emission tomography/CT,[
A positive actinomycosis culture occurs in 50% of cases. Therefore, diagnosis is generally made by histology.[
Patients with actinomycosis require high doses of penicillin’s G or amoxicillin for long periods of time (6–12 months), but the duration of antimicrobial therapy could be reduced to 3 months in patients with total surgical resection.[
CONCLUSION
Craniofacial actinomycosis is the most common presentation of actinomycosis. However, it continues to be a rare and difficult disease to diagnose and is often confused with a neoplastic process. Resective surgery still plays an important role for diagnosis, while chronic treatment with high-dose penicillin’s remains the therapeutic pillar to control the disease and prevent recurrence. Histology is the cornerstone diagnostic study in patients with craniofacial presentation. 99mTc-UBI 29-41 bone SPECT/CT scan is a noninvasive study that identifies bacterial infection and could be play an auxiliary role in the diagnosis and follow-up of these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
None.
References
1. Ajal M, Turner J, Fagan P, Walker P. Actinomycosis otomastoiditis. J Laryngol Otol. 1997. 111: 1069-71
2. Aktolun C, Demirel D, Kir M, Bayhan H, Maden HA. Technetium-99m-MIBI and thallium-201 uptake in pulmonary actinomycosis. J Nucl Med. 1991. 32: 1429-31
3. Bolton CF, Ashenhurst EM. Actinomycosis of the brain; case report and review of the literature. Can Med Assoc J. 1964. 90: 922-8
4. Bonnefond S, Catroux M, Melenotte C, Karkowski L, Rolland L, Trouillier S. Clinical features of actinomycosis: A retrospective, multicenter study of 28 cases of miscellaneous presentations. Medicine (Baltimore). 2016. 95: e3923
5. Chatterjee RP, Shah N, Kundu S, Mahmud SA, Bhandari S. Cervicofacial actinomycosis mimicking osseous neoplasm: A rare case. J Clin Diagn Res. 2015. 9: ZD29-31
6. Chopra S, Christie M, Felimban H. Intracranial actinomycosis mimicking meningioma. Ann Saudi Med. 1995. 15: 515-8
7. de Murphy CA, Gemmel F, Balter J. Clinical trial of specific imaging of infections. Nucl Med Commun. 2010. 31: 726-33
8. Deora H, Beniwal M, Rao S, Rao K, Vikas V, Somanna S. Wolf in Sheep’s clothing: Intracranial actinomycosis masquerading as en-plaque meningioma. Surg Neurol Int. 2018. 9: 39
9. Dillmann-Arroyo C, Cantu-Leal R, Campa-Nunez H, Lopez-Cavazos C, Bermudez-Arguelles M, Mejia-Herrera JC. Application of the ubiquicidin 29-41 scan in the diagnosis of pyogenic vertebral osteomyelitis. Acta Ortop Mex. 2011. 25: 27-31
10. Ham HY, Jung S, Jung TY, Heo SH. Cerebral actinomycosis: Unusual clinical and radiological findings of an abscess. J Korean Neurosurg Soc. 2011. 50: 147-50
11. Hwang CS, Lee H, Hong MP, Kim JH, Kim KS. Brain abscess caused by chronic invasive actinomycosis in the nasopharynx: A case report and literature review. Medicine (Baltimore). 2018. 97: e0406
12. Khosla VK, Banerjee AK, Chopra JS. Intracranial actinomycoma with osteomyelitis simulating meningioma. Case report. J Neurosurg. 1984. 60: 204-7
13. Kobayashi T, Ford B, Fujita N, Appenheimer AB. Ocular actinomycosis mimicking meningioma. Open Forum Infect Dis. 2020. 7: ofaa170
14. Liu Y. Actinomycosis-induced adnexal and uterine masses mimicking malignancy on FDG PET/CT. Am J Obstet Gynecol. 2019. 220: 281
15. Love C, Palestro CJ. Nuclear medicine imaging of bone infections. Clin Radiol. 2016. 71: 632-46
16. Nomura M, Shin M, Ohta M, Nukui Y, Ohkusu K, Saito N. Atypical osteomyelitis of the skull base and craniovertebral junction caused by Actinomyces infection-case report. Neurol Med Chir (Tokyo). 2011. 51: 64-6
17. Oostman O, Smego RA. Cervicofacial actinomycosis: Diagnosis and management. Curr Infect Dis Rep. 2005. 7: 170-4
18. Oukessou Y, Elkerdoudi MA, Abada RL, Mahtar M. Complicated actinomycosis of the temporal bone: A historical case report. Eur Ann Otorhinolaryngol Head Neck Dis. 2015. 132: 227-9
19. Pant R, Marshall TL, Crosher RF. Facial actinomycosis mimicking a desmoid tumour: Case report. Br J Oral Maxillofac Surg. 2008. 46: 391-3
20. Pulverer G, Schutt-Gerowitt H, Schaal KP. Human cervicofacial actinomycoses: Microbiological data for 1997 cases. Clin Infect Dis. 2003. 37: 490-7
21. Shah KM, Karagir A, Kanitkar S, Koppikar R. An atypical form of cervicofacial actinomycosis treated with short but intensive antibiotic regimen. BMJ Case Rep. 2013. 2013: bcr2013008733
22. Smego RA, Foglia G. Actinomycosis. Clin Infect Dis. 1998. 26: 1255-61
23. Soto-Hernandez JL, Morales VA, Giron JC, Banares JB. Cranial epidural empyema with osteomyelitis caused by actinomyces, CT, and MRI appearance. Clin Imaging. 1999. 23: 209-14
24. Valour F, Senechal A, Dupieux C, Karsenty J, Lustig S, Breton P. Actinomycosis: Etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014. 7: 183-97
25. Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011. 343: d6099
26. Yenson A, deFries HO, Deeb ZE. Actinomycotic osteomyelitis of the facial bones and mandible. Otolaryngol Head Neck Surg. 1983. 91: 173-6