- Department of Neurosurgery, Wake Forest School of Medicine, Winston-Salem, North Carolina, United States.
- Department of Public Health Sciences, Wake Forest University Health Sciences, Winston-Salem, North Carolina, United States.
- Department of Neurosurgery, Wake Forest Baptist Health, Winston-Salem, North Carolina, United States.
Correspondence Address:
Katriel E. Lee
Department of Neurosurgery, Wake Forest Baptist Health, Winston-Salem, North Carolina, United States.
DOI:10.25259/SNI_954_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Katriel E. Lee1, Tamriage A. Martin1, Keyan A. Peterson1, Carol Kittel2, Aqib H. Zehri3, Jonathan L. Wilson3. Factors associated with length of stay after single-level posterior thoracolumbar instrumented fusion primarily for degenerative spondylolisthesis. 10-Feb-2021;12:48
How to cite this URL: Katriel E. Lee1, Tamriage A. Martin1, Keyan A. Peterson1, Carol Kittel2, Aqib H. Zehri3, Jonathan L. Wilson3. Factors associated with length of stay after single-level posterior thoracolumbar instrumented fusion primarily for degenerative spondylolisthesis. 10-Feb-2021;12:48. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10584
Abstract
Background: The postoperative length of stay (LOS) is an important prognostic indicator for patients undergoing instrumented spinal fusion surgery. Increased LOS can be associated with higher infection rates, higher incidence of venous thromboembolisms, and a greater frequency of hospital-acquired delirium. The day of surgery and early postoperative mobilization following single-level posterior thoracolumbar stabilizations may impact the LOS. In this study, we evaluated the effects of weekday (Monday–Thursday) versus weekend (Friday–Sunday) surgery and postoperative rehabilitation services on LOS following primarily transforaminal lumbar interbody fusion (TLIF) for degenerative spondylolisthesis (DS).
Methods: In this single-institution retrospective chart review, we identified 198 adults who received a one-level thoracolumbar instrumented fusion through a posterior only approach (2017–2019). The majority of these patients underwent TLIF for DS. A zero truncated negative binomial model was used for predictors of the primary outcome of LOS (weekday of surgery, duration of operation, first or repeat surgery, and physical therapy/ occupational therapy [PT/OT] evaluation). Covariates were sex, age, and body mass index.
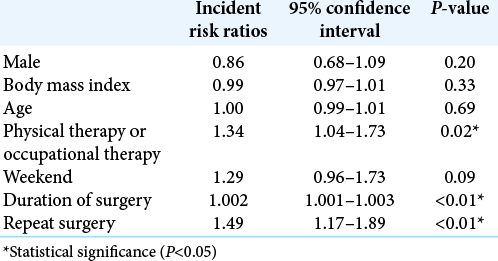
Results: We found that operative duration, repeat surgery, and in-hospital PT/OT all significantly increased the LOS (P P = 0.09).
Conclusion: In our patient sample, duration, repeat surgery, and in-hospital PT/OT increased the LOS following primarily TLIF for DS. The increased LOS in these cases is likely due to higher overall disease burden and case complexity. In addition, those patients with a greater likelihood of extended recovery and ongoing neurologic deficits are more likely to have PT/OT evaluations. Notably, LOS was not significantly impacted by the day of surgery at our institution.
Keywords: Length of stay, Rehabilitation, Spinal fusion, Spine
INTRODUCTION
Thoracic and lumbar posterior fusions have proven effective for the treatment of degenerative spinal pathologies, trauma, infection, and neoplasia. Postoperative length of stay (LOS) is a valuable prognostic indicator for patients undergoing spine surgery, as longer LOS after spine surgery is associated with increased risk of postoperative infection, venous thromboembolism, and delirium.[
MATERIALS AND METHODS
This is a single-institution retrospective chart review of 198 patients who underwent single-level thoracolumbar fusion through a posterior only approach with or without interbody placement (2017–2019) at Wake Forest Baptist Medical Center, Davie Medical Center, and High Point Medical Center. Data collected included demographics, ambulatory status, surgical factors (indication, level of surgery, approach, duration of operation, and day of week of surgery), LOS, PT/OT visits, complications, disposition, and readmissions.
Data analysis
A zero truncated negative binomial model was constructed to predict the primary outcome of LOS. Predictors included weekends versus weekdays, duration of surgery, repeat surgery, and PT/OT (yes vs. no). Covariates included sex, body mass index (BMI), and age. Negative binomial regression was chosen to model LOS as the distribution of counts is skewed right and overdispersed. Incident risk ratios with 95% confidence intervals (CI) are reported. All analyses were conducted using R:A language and environment for statistical computing, R Foundation for Statistical Computing, Version 3.6.1, Vienna Austria and RStudio: Integrated Development for R., Version 1.1.456 Rstudio, Inc., Boston, MA, USA.
RESULTS
Patient characteristics, complications, and disposition
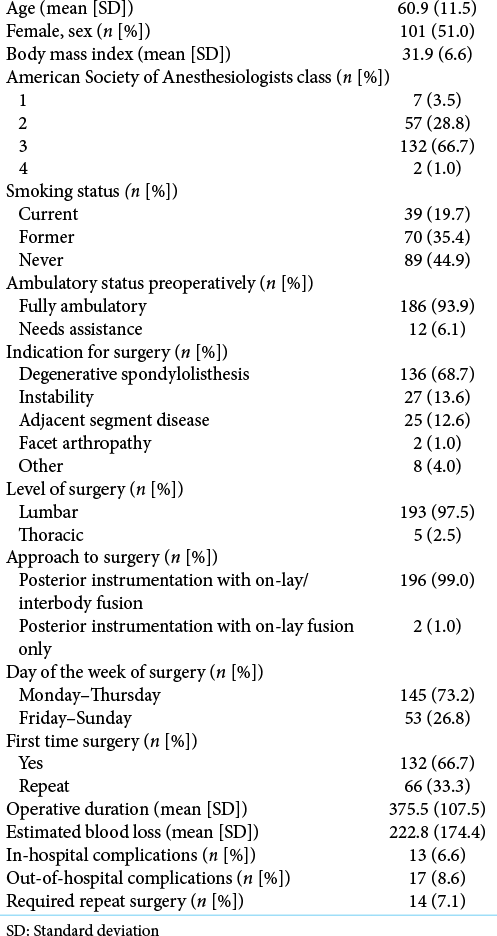
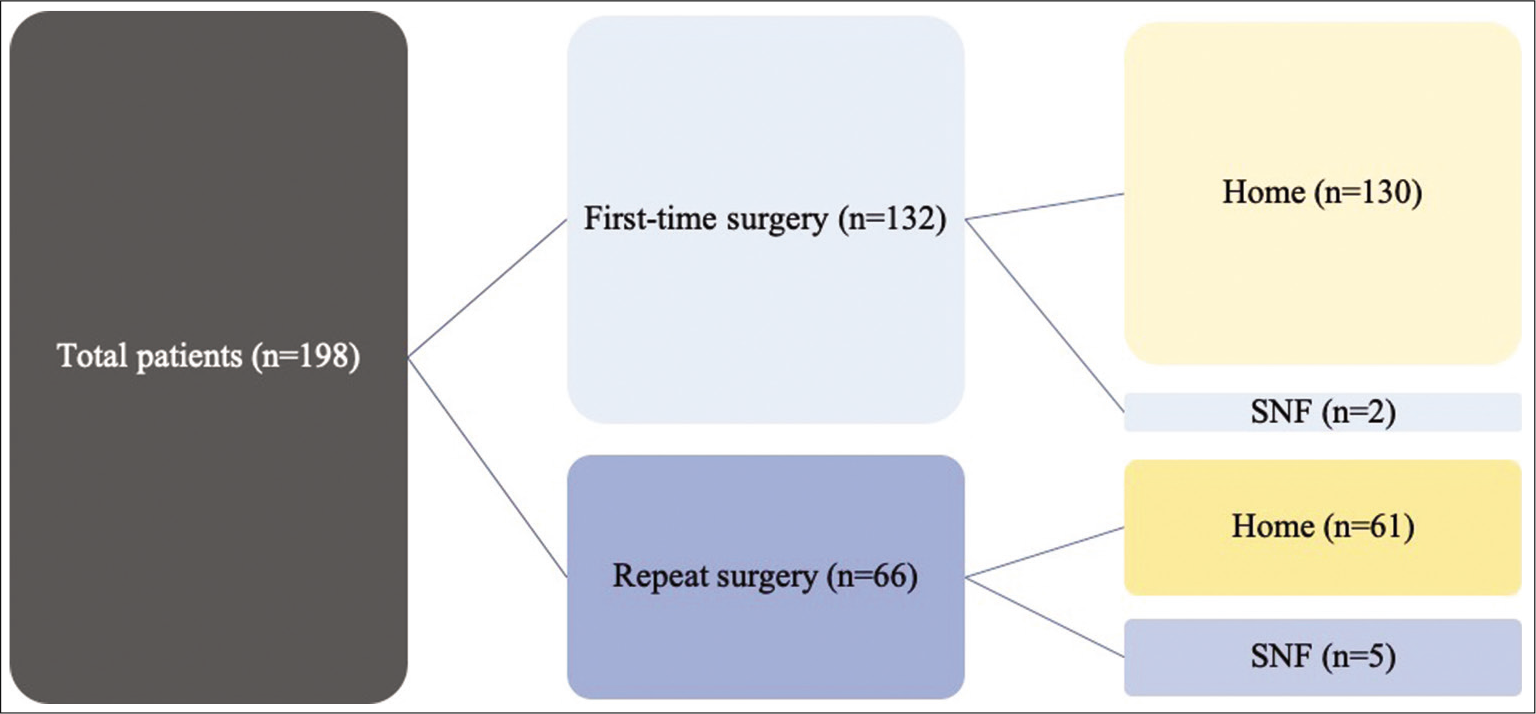
The study included 198 patients whose clinical data/ characteristics and outcomes are defined in [
LOS
The range of LOS was 1–20 days with a median [IQR] of 2[
Effect of PT/OT
Of the 198 patients, 104 patients (52.5%) underwent PT or OT during their hospital stay, receiving an average of 1.9 PT sessions and 1.41 OT sessions while inpatient. Of those who underwent PT or OT, 57.7% utilized both PT and OT services.
Patients who had PT and/or OT in the hospital had a LOS 1.34 times longer than those who did not (CI [1.04–1.73], P = 0.02). For each additional PT session in the hospital, discharge is extended by 0.4 days (P = 0.04). The average time from PT order being placed to the patient first being seen by PT is 0.52 days. For each additional OT session in the hospital, discharge is extended by 0.8 days (P = 0.01). The average time from OT order being placed to the patient first being seen by OT is 0.76 days. There was no significant difference in time from OT order placed to being seen on the weekends versus the weekdays (P = 0.42) or in time from PT order placed to being seen on weekends versus weekdays (P = 0.86). Patients were most often seen by PT/OT on postoperative day (POD) 1, with mean standard deviation (SD) first PT visit on POD 1.46 (1.28) and mean (SD) first OT visit on POD 0.76 (0.84).
Patients who underwent PT/OT did not differ significantly in BMI (P = 0.38) or preoperative ambulatory status (P = 0.45). However, patients who did get PT/OT had an ASA class more likely to be greater than or equal to 3 (P = 0.04).
DISCUSSION
Prior studies assessing LOS in lumbar fusion patients have inconsistent findings and did not specifically explore the effects of PT/OT as related to the day of the week of surgery in posterior single-level thoracolumbar fusions.[
Past studies have explored the effect of weekend hospital admissions on LOS and outcomes. One meta-analysis revealed that the mean hospital LOS was 1 day shorter on weekends, with the exception of studies regarding elective procedures and maternity admissions. However, this was partly attributed to a higher proportion of patient deaths and higher acuity cases among weekend admissions.[
Rather than PT/OT decreasing LOS, patients who had PT or OT in the hospital had a LOS 1.34 times longer than those who did not. This increased LOS can partly be explained by the indications for ordering PT/OT. The use of PT/OT in patients at our institution is not standardized and is dependent on provider discretion. Older patients, patients with more comorbidities, or patients with a complicated operative course are generally recommended to receive PT/OT. The therapy team may also recommend continued inpatient rehab before discharge, thus prolonging LOS. The increased LOS may also be due to the delay from time ordering PT/OT to the time seeing the patient. This is potentially a modifiable factor that could be mitigated by more staff dedicated solely to mobilization of these patients while awaiting more advanced therapy service evaluation and/or purely hiring more PT/OT staff. In addition, most of our patients received PT/OT on POD 1 rather than on the same day of surgery. Earlier mobilization on POD 0 versus POD 1 has been found to decrease LOS in patients with total joint arthroplasty,[
Our findings that PT and OT are associated with an increased LOS create a unique challenge for surgeons as they are faced with the decision whether or not to order PT/OT after single-level thoracolumbar fusions. In medically complex patients, increased LOS is associated with increased morbidities; however, early postoperative mobilization can minimize these same risks. Using our data, in combination with previous literature, we recommend mobilization on POD 0 for patients with a higher ASA score, more complex surgery (extended duration or blood loss), and difficulty mobilizing preoperatively.
Our present study is limited in the fact that it is not prospective in nature, and the follow-up interval was on average less than a year. Our sample size of 198 appears small for a large academic center; this is because patients at our institution have increased likelihood of multilevel disease and deformity, which limits number of single level fusions only. In addition, our average mobilization was POD 1, when data suggest for other elective surgeries that PT/OT should be initiated on POD 0. Future prospective, randomized studies with a larger sample size are needed to further explore the relationships between PT/OT, LOS, and patient-level factors that may indicate more successful PT/ OT intervention.
CONCLUSION
LOS significantly increased for patients who underwent single-level thoracolumbar instrumented fusion primarily for DS with increased operative duration, repeat procedures, and PT/OT intervention with mobilization on POD 1–2, while there was only a trend toward increased LOS for surgery performed on weekdays versus weekends.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aylin P, Alexandrescu R, Jen MH, Mayer EK, Bottle A. Day of week of procedure and 30 day mortality for elective surgery: Retrospective analysis of hospital. BMJ. 2013. 346: f2424
2. Basques B, Fu M, Buerba R, Bohl D, Golinvaux N, Grauer J. Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine (Phila Pa 1976). 2015. 39: 497-502
3. Bell C, Redelmeier D. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001. 345: 663-8
4. Chen AF, Stewart MK, Heyl AE, Klatt BA. Effect of immediate postoperative physical therapy on length of stay for total joint arthroplasty patients. J Arthroplasty. 2012. 27: 851-6
5. Chen Y, Armoiry X, Higenbottam C, Cowley N, Basra R, Watson SI. Magnitude and modifiers of the weekend effect in hospital admissions: A systematic review and meta-analysis. BMJ Open. 2019. 9: e025764
6. Epstein NE. A review article on the benefits of early mobilization following spinal surgery and other medical/ surgical procedures. Surg Neurol Int. 2014. 5: S66-73
7. Gruskay JA, Fu M, Bohl DD, Webb ML, Grauer JN. Factors affecting length of stay after elective posterior lumbar spine surgery: A multivariate analysis. Spine J. 2015. 15: 1188-95
8. Hijji FY, Narain AS, Haws BE, Khechen B, Kudaravalli KT, Yom KH. Does day of surgery affect hospital length of stay and charges following minimally invasive transforaminal lumbar interbody fusion?. Clin Spine Surg. 2018. 31: E291-5
9. Nielsen P, Jorgensen L, Dahl B, Pedersen T, Tonesen H. Prehabilitation and early rehabilitation after spinal surgery: Randomized clinical trial. Clin Rehabil. 2010. 24: 137-48
10. Sivaganesan A, Devin CJ, Khan I, Kerezoudis P, Nian H, Harrell FE. Is length of stay influenced by the weekday on which lumbar surgery is performed?. Neurosurgery. 2019. 85: 494-9
11. Wang D, Teddy PJ, Henderson NJ, Shine BS, Gardner BP. Mobilization of patients after spinal surgery for acute spinal cord injury. Spine (Phila Pa 1976). 2001. 26: 2278-82