- Department of Neurosurgery, Graduate School of Medicine, Tohoku University, Sendai, Miyagi, Japan.
- Department of Neurosurgery, Kohnan Hospital, , Tohoku University, Sendai, Miyagi, Japan.
- Department of Neurosurgical Engineering and Translational Neuroscience, Graduate School of Biomedical Engineering, , Tohoku University, Sendai, Miyagi, Japan.
- Department of Neurosurgical Engineering and Translational Neuroscience, Graduate School of Medicine, Tohoku University, Sendai, Miyagi, Japan.
Correspondence Address:
Hidenori Endo
Department of Neurosurgery, Graduate School of Medicine, Tohoku University, Sendai, Miyagi, Japan.
DOI:10.25259/SNI_38_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuto Shingai1, Hidenori Endo1,2, Toshiki Endo1, Shin-ichiro Osawa1, Kuniyasu Nizuma1,3,4, Teiji Tominaga1. Ocular neuromyotonia caused by a recurrent sphenoidal ridge meningioma. 10-May-2021;12:219
How to cite this URL: Yuto Shingai1, Hidenori Endo1,2, Toshiki Endo1, Shin-ichiro Osawa1, Kuniyasu Nizuma1,3,4, Teiji Tominaga1. Ocular neuromyotonia caused by a recurrent sphenoidal ridge meningioma. 10-May-2021;12:219. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10795
Abstract
Background: Ocular neuromyotonia (ONM) is a rare ocular motility disorder characterized by involuntary paroxysmal extraocular muscle contraction and is caused by radiation therapy, vascular compression, and inflammatory disease. This study includes a rare case of ONM caused by a recurrent meningioma.
Case Description: A 56-year-old man presented with diplopia due to the right oculomotor nerve palsy caused by a sphenoidal atypical meningioma, with improved symptoms after initial surgery. During the next 7 years, he underwent local radiation therapy, second surgery, and Gamma Knife radiosurgery to control the tumor’s repetitive recurrence around the right anterior clinoid process. After these treatments, residual tumor was controlled for the next 3 years. However, 3 months after his last visit, he started to suffer from the right ONM and visual disturbance. The magnetic resonance imaging results revealed a rapid growth of the posterior part of the residual tumor, involving the right oculomotor nerve. The third tumor resection was performed to prevent further aggravation of the symptoms. Decompression of the right oculomotor nerve was achieved, and ONM disappeared immediately after surgery.
Conclusion: If nerve compression by the tumor is clearly indicated with the neuroradiological assessment, surgical intervention is the treatment of choice to improve ONM.
Keywords: Diplopia, Meningioma, Ocular neuromyotonia, Radiation, Surgery
INTRODUCTION
Neuromyotonia is a condition of spontaneous and continuous muscle fiber activity of the peripheral nerve origin.[
CASE REPORT
A 56-year-old man presented with diplopia due to the right oculomotor nerve palsy. The magnetic resonance imaging (MRI) results revealed a large sphenoidal tumor [
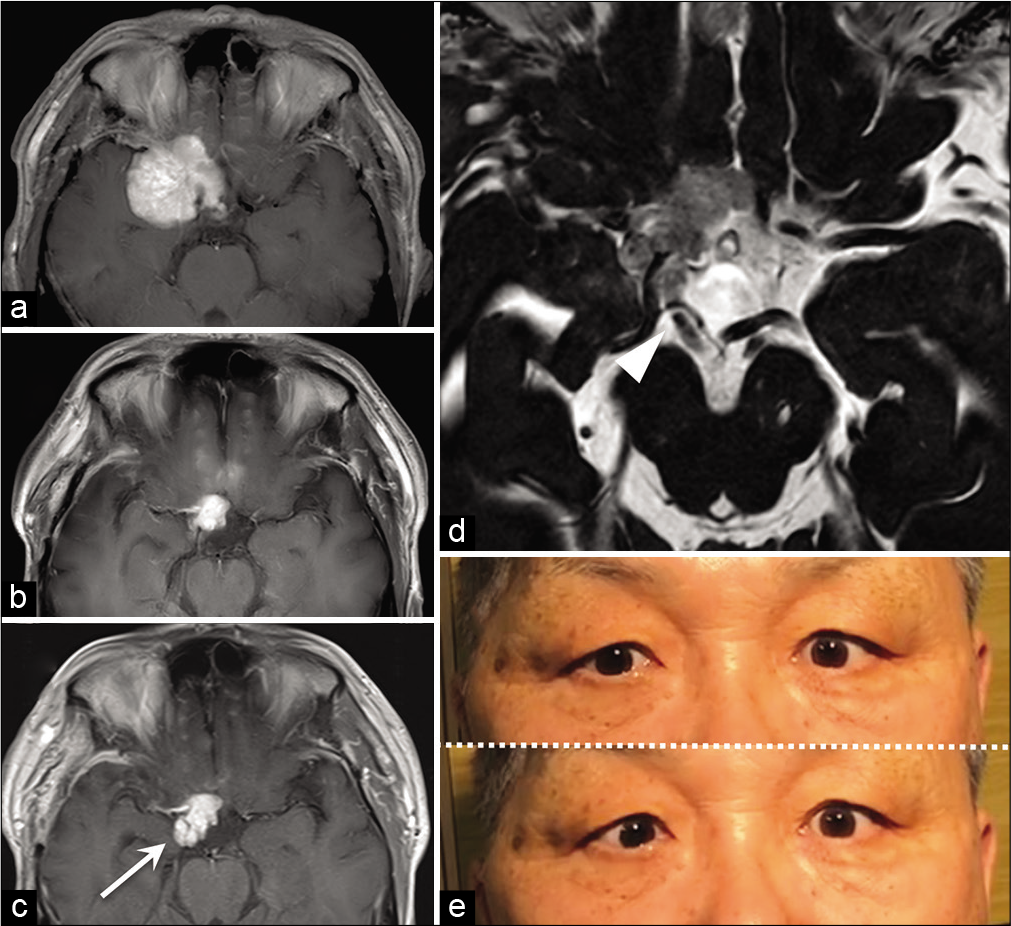
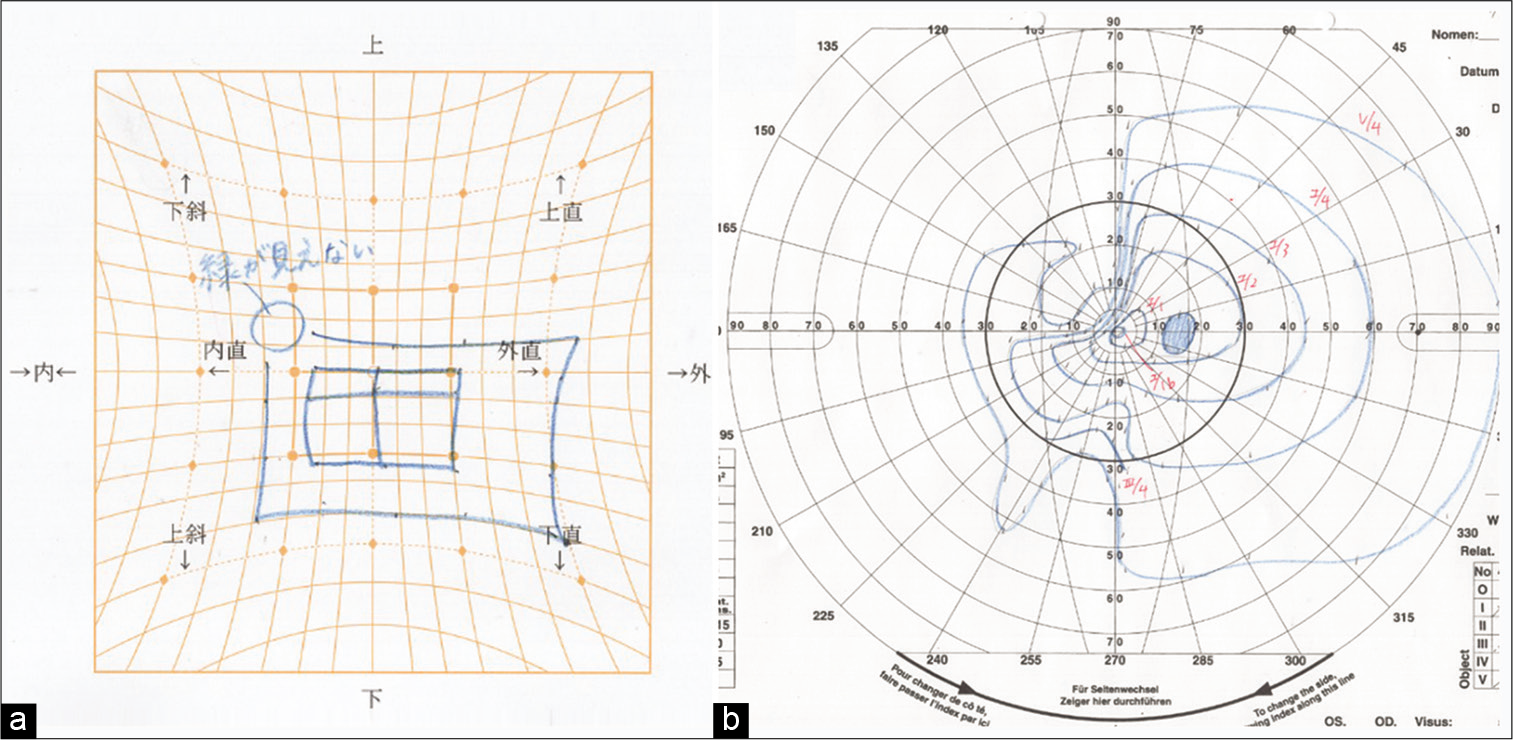
Figure 1:
(a) T1-weighted imaging with gadolinium enhancement at the initial presentation showing a large right sphenoidal tumor. (b) T1-weighted imaging after Gamma Knife radiosurgery for recurrent tumor showing a residual tumor around the right anterior clinoid process. (c) T1-weighted imaging during the occurrence of ocular neuromyotonia (ONM) showing a rapid growth of the posterior part of the tumor (arrow). (d) Heavily T2-weighted imaging during the occurrence of ONM showing the right oculomotor nerve involvement (arrowhead). (e) ONM symptom. The position of the eyes in the normal status (upper) and ONM (lower).
Three months after his last visit, he started to suffer from intermittent diplopia. MRI revealed a rapid growth of the posterior part of the residual tumor [
Video 1
The third tumor resection was performed through the right pterional approach to prevent further visual disturbance aggravation. After the removal of the tumor occupying the right retrocarotid space, the oculomotor nerve was found within the tumor and was preserved [
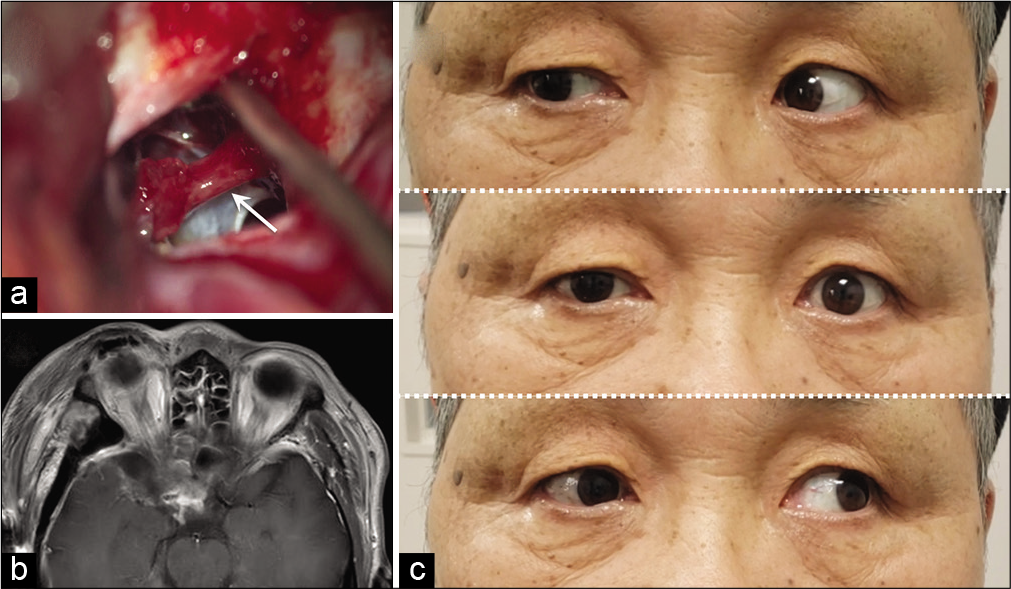
Figure 3:
(a) An intraoperative view of the right oculomotor nerve after tumor removal (arrow). (b) T1-weighted imaging with gadolinium enhancement after surgery showing that most of the tumor was removed. (c) Eye movement after surgery showing a resolution of the right ONM with only a slight disturbance of the inward movement of the right eye.
ONM disappeared immediately after surgery. A transient worsening of the right oculomotor nerve palsy occurred, which gradually recovered in the preoperative level [
Video 2
DISCUSSION
Paroxysmal ocular movement abnormalities can be caused by the damage of the cranial nerves, such as the oculomotor, trochlear, and abducens nerves. Among them, the symptom associated with the trochlear and oculomotor nerves or the abducens nerve is known as superior oblique myokymia[
The exact mechanism of ONM remains unclear. Several mechanisms have been proposed in recent literatures. One of the hypotheses is that nerve injury leads to segmental demyelination, resulting in local ephaptic transmission.[
In this case, previous radiation therapy might have potentially impaired the right oculomotor nerve. Subsequently, nerve compression by the tumor recurrence overlapped. Considering the improvement of ONM after surgery, the tumor compression of the right oculomotor nerve was the main cause of his symptom, which can be explained by the improvement of trigeminal neuralgia or hemifacial spasm after microvascular decompression.
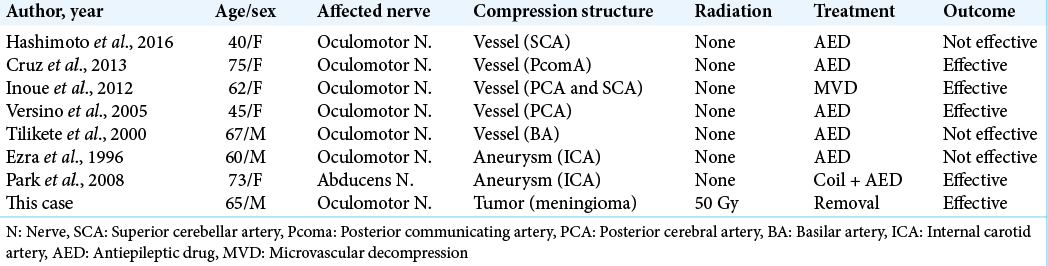
ONM has been treated with medication or surgery. Seven cases with ONM have been reported in the English literature, in which the relationship between the symptom and nerve compression was clearly indicated [
CONCLUSION
ONM is a rare ocular motility disorder caused due to nerve compression by an intracranial tumor. If nerve compression is clearly indicated with the neuroradiological assessment, then surgical intervention is the treatment of choice.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Ezra E, Spalton D, Sanders MD, Graham EM, Plant GT. Ocular neuromyotonia. Br J Ophthalmol. 1996. 80: 350-5
2. Hashimoto Y, Hideyama T, Yamagami A, Sasaki T, Maekawa R, Shiio Y. A case of ocular neuromyotonia caused by neurovascular compression of the oculomotor nerve by the elongated superior cerebellar artery. J Neurol. 2016. 263: 1236-8
3. Inoue T, Hirai H, Shimizu T, Tsuji M, Shima A, Suzuki F, Matsuda M. Ocular neuromyotonia treated by microvascular decompression: Usefulness of preoperative 3D imaging: Case report. J Neurosurg. 2012. 117: 1166-9
4. Kameyama S, Masuda H, Shirozu H, Ito Y, Sonoda M, Kimura J. Ephaptic transmission is the origin of the abnormal muscle response seen in hemifacial spasm. Clin Neurophysiol. 2016. 127: 2240-5
5. Kim KJ, Kim JM, Kim SH, Bae YJ. Coexistence of ocular neuromyotonia and hemifacial spasm. Neurology. 2016. 86: 402
6. Kung NH, Bucelli RC, McClelland CM, van Stavern GP. Ocular neuromyotonia associated with chronic inflammatory demyelinating polyneuropathy. Neuroophthalmology. 2015. 39: 240-2
7. Maddison P. Neuromyotonia. Clin Neurophysiol. 2006. 117: 2118-27
8. Mino M, Yoshida M, Morita T, Tominaga T. Outcomes of oculomotor nerve palsy caused by internal carotid artery aneurysm: Comparison between microsurgical clipping and endovascular coiling. Neurol Med Chir (Tokyo). 2015. 55: 885-90
9. Park HY, Hwang JM, Kim JS. Abducens neuromyotonia due to internal carotid artery aneurysm. J Neurol Sci. 2008. 270: 205-8
10. Soares-Dos-Reis R, Martins AI, Brás A, Matos A, Bento C, Lemos J. Ocular neuromyotonia. Pract Neurol. 2018. 18: 389-90
11. Strupp M, Dieterich M, Brandt T, Feil K. Therapy of vestibular paroxysmia, superior oblique myokymia, and ocular neuromyotonia. Curr Treat Options Neurol. 2016. 18: 34
12. Tilikete C, Vial C, Niederlaender M, Bonnier PL, Vighetto A. Idiopathic ocular neuromyotonia: A neurovascular compression syndrome?. J Neurol Neurosurg Psychiatry. 2000. 69: 642-4
13. Versino M, Colnaghi S, Todeschini A, Candeloro E, Ravaglia S, Moglia A. Ocular neuromyotonia with both tonic and paroxysmal components due to vascular compression. J Neurol. 2005. 252: 227-9