- Department of Neurosurgery, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy.
- Neurosurgical Intensive Care Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy.
Correspondence Address:
Nicola Montano, Department of Neurosurgery, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy.
DOI:10.25259/SNI_42_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nicola Montano1, Francesco Signorelli1, Martina Giordano1, Ginevra Federica D’Onofrio1, Alessandro Izzo1, Manuela D’Ercole1, Eleonora Ioannoni2, Giovanni Pennisi1, Anselmo Caricato2, Roberto Pallini1, Alessandro Olivi1. Factors associated with cerebrospinal fluid leak after a retrosigmoid approach for cerebellopontine angle surgery. 07-Jun-2021;12:258
How to cite this URL: Nicola Montano1, Francesco Signorelli1, Martina Giordano1, Ginevra Federica D’Onofrio1, Alessandro Izzo1, Manuela D’Ercole1, Eleonora Ioannoni2, Giovanni Pennisi1, Anselmo Caricato2, Roberto Pallini1, Alessandro Olivi1. Factors associated with cerebrospinal fluid leak after a retrosigmoid approach for cerebellopontine angle surgery. 07-Jun-2021;12:258. Available from: https://surgicalneurologyint.com/surgicalint-articles/factors-associated-with-cerebrospinal-fluid-leak-after-a-retrosigmoid-approach-for-cerebellopontine-angle-surgery/
Abstract
Background: The retrosigmoid approach represents a crucial surgical route to address different lesions in the cerebellopontine angle but cerebrospinal fluid (CSF) leak still remains the most frequent complication after this approach. Here, we analyzed the impact of different factors in CSF leak development after a retrosigmoid approach. Identifying risk factors related to a specific approach may help the surgeon to tailor the perioperative management and to appropriately counsel patients regarding their risk profile.
Methods: We retrospectively reviewed the clinical, surgical, and outcome data of 103 consecutive patients (M/F, 47/56; mean follow-up 35.6 ± 23.9 months) who underwent a retrosigmoid approach for different cerebellopontine angle pathologies and studied the impact of different factors on the occurrence of a CSF leak to univariate and multivariate analysis.
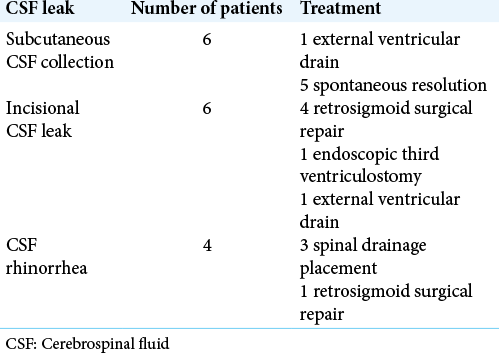
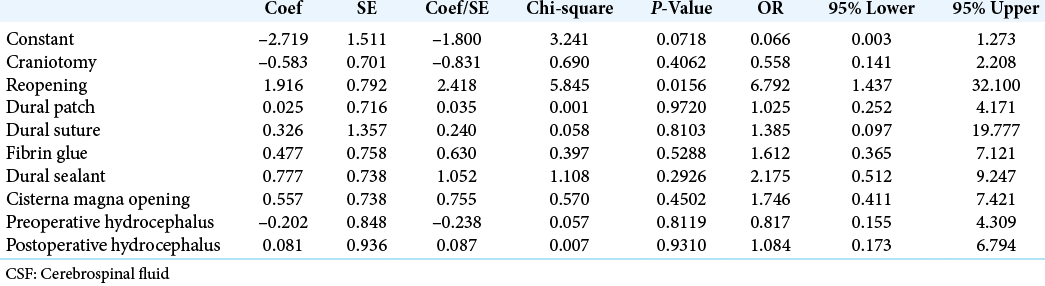
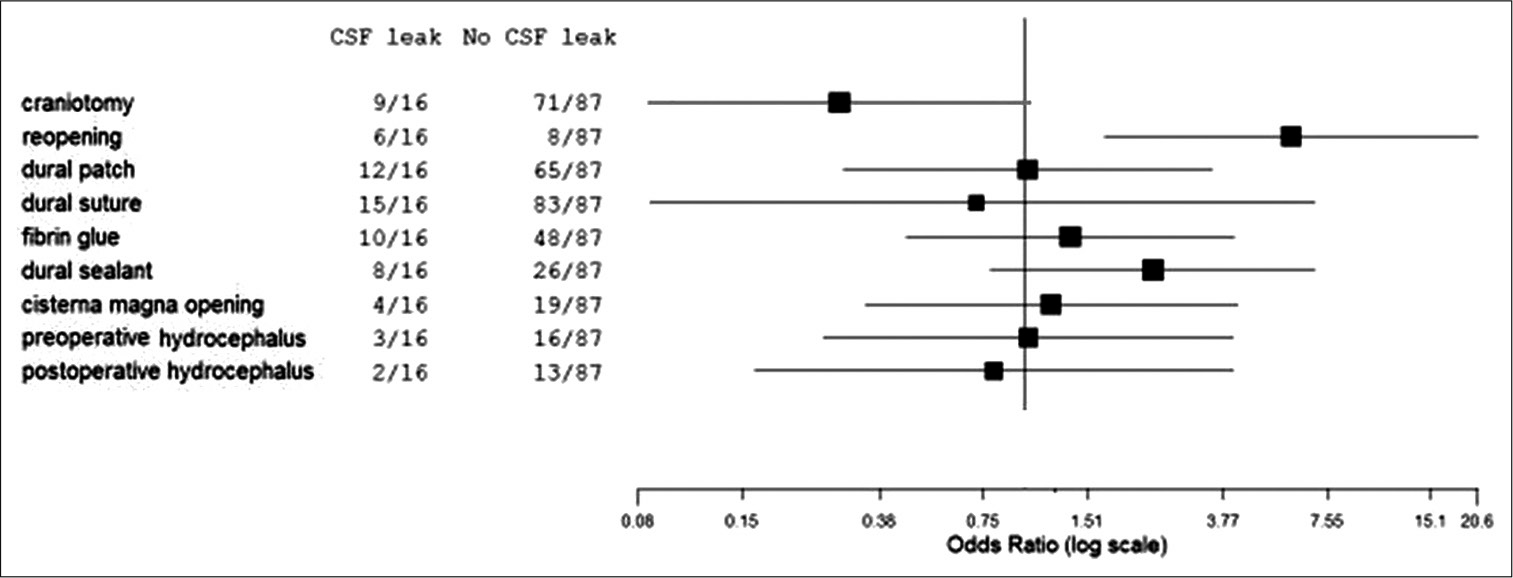
Results: Seventy-nine patients (76.7%) were operated for tumors growing in the cerebellopontine angle. Twenty-four patients (23.2%) underwent microvascular decompression to treat a drug-resistant trigeminal neuralgia. Sixteen patients (15.5%) developed CSF leak in the postoperative course of which six underwent surgical revision. Performing a craniectomy as surgical procedure (P = 0.0450) and performing a reopening procedure (second surgery; P = 0.0079) were significantly associated to a higher risk of developing CSF leak. Moreover, performing a reopening procedure emerged as an independent factor for CSF developing on multivariate analysis (P = 0.0156).
Conclusion: Patients submitted to craniectomy and patients who underwent a second surgery showed an higher CSF leak rate. Ongoing improvement of biomaterial technology may help neurosurgeons to prevent this potentially life-threatening complication.
Keywords: Craniotomy, Cerebrospinal fluid leak, Craniectomy, Neurovascular conflict, Retrosigmoid approach, Vestibular schwannoma
INTRODUCTION
The retrosigmoid approach represents an excellent surgical route to address various tumors and vascular lesions in the cerebellopontine angle.[
MATERIALS AND METHODS
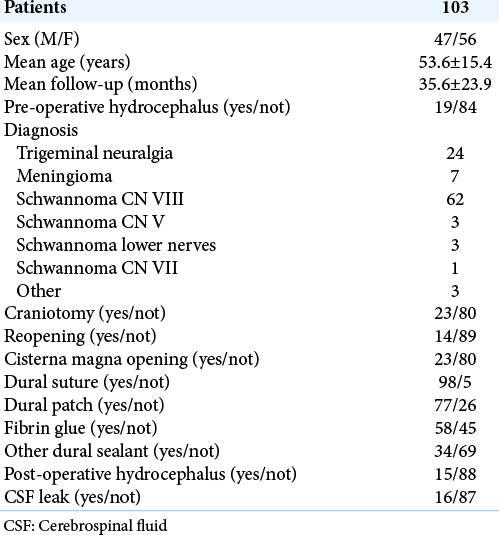
We retrospectively reviewed the clinical, surgical and outcome data of 103 consecutive patients (M/F, 47/56) who underwent a retrosigmoid approach for cerebellopontine angle pathologies between February 2013 and December 2019 at our department. The mean age was 53.6 ± 15.4 years and the mean follow-up was 35.6 ± 23.9 months. We studied the role of factors such as age, sex, the type of pathology, the evidence of preoperative and postoperative hydrocephalus, and the type of surgical procedure (craniotomy/craniectomy) or if the procedure was a reopening (second surgery), the cisterna magna opening during surgery, the use of dural suture, dural patch, fibrin glue, and other dural sealants during surgery on the occurrence of a CSF leak (subcutaneous collection, incisional leak, CSF rhinorrhea, and CSF otorrhea) in the postoperative course of these patients. The surgical procedures were performed by different neurosurgeons thus the closure techniques varied according to the surgeon’s preference. The dura was sutured either with a 3–0 silk suture (40 cases) or with a 4–0 nylon suture (58 cases). An artificial dural substitute was used in all cases of dural patch (77 cases). For patients in whom CSF leak occurred, the type of treatment was also recorded. Statistical comparison of categorical variables was performed by χ2 statistic, using the Fisher exact test. A multivariate logistic regression model was used to estimate the odds ratio of developing a CSF leak, while adjusting for baseline variables. Differences were considered significant at P < 0.05. Statistical analyses were done using StatView version 5 software (SAS Institute Inc.).
RESULTS
Data of patients are summarized in
DISCUSSION
The retrosigmoid approach to the cerebellopontine angle, first popularized in the 1930s by Dandy,[
Our study has some limitations due to the retrospective nature of data. For this reason, we were not able to study the impact of body mass index which might affect the complication rate in this type of surgery.[
CONCLUSION
In our study, we identified subgroups of patients who were at risk for CSF leak occurrence after a retrosigmoid approach for the treatment of different pathologies. Patients submitted to craniectomy and patients who underwent a second surgery showed an higher CSF leak rate. Ongoing improvement of biomaterial technology[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aldahak N, Dupre D, Ragaee M, Froelich S, Wilberger J, Aziz KM. Hydroxyapatite bone cement application for the reconstruction of retrosigmoid craniectomy in the treatment of cranial nerves disorders. Surg Neurol Int. 2017. 8: 115
2. Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2007. 31: 556-61
3. Brennan JW, Rowed DW, Nedzelski JM, Chen JM. Cerebrospinal fluid leak after acoustic neuroma surgery: Influence of tumor size and surgical approach on incidence and response to treatment. J Neurosurg. 2001. 94: 217-23
4. Bryce GE, Nedzelski JM, Rowed DW, Rappaport JM. Cerebrospinal fluid leaks and meningitis in acoustic neuroma surgery. Otolaryngol Head Neck Surg. 1991. 104: 81-7
5. Chern A, Hunter JB, Bennett ML. Cost analysis of cerebrospinal fluid leaks and cerebrospinal fluid leak prevention in patients undergoing cerebellopontine angle surgery. Otol Neurotol. 2016. 38: 147-51
6. Ciric I, Zhao JC, Rosenblatt S, Wiet R, O’Shaughnessy B. Suboccipital retrosigmoid approach for removal of vestibular schwannomas: Facial nerve function and hearing preservation. Neurosurgery. 2005. 56: 560-70
7. Copeland WR, Mallory GW, Neff BA, Driscoll CL, Link MJ. Are there modifiable risk factors to prevent a cerebrospinal fluid leak following vestibular schwannoma surgery?. J Neurosurg. 2015. 122: 312-6
8. Cueva RA, Mastrodimos B. Approach design and closure techniques to minimize cerebrospinal fluid leak after cerebellopontine angle tumor surgery. Otol Neurotol. 2005. 26: 1176-81
9. Dandy WE. Removal of cerebellopontine (acoustic) tumors through a unilateral approach. Arch Surg. 1934. 29: 337-44
10. Della Pepa GM, Montano N, Lucantoni C, Alexandre AM, Papacci F, Meglio M. Craniotomy repair with the retrosigmoid approach: The impact on quality of life of meticulous reconstruction of anatomical layers. Acta Neurochir (Wien). 2011. 153: 2255-8
11. Duong DH, O’Malley S, Sekhar LN, Wright DG. Postoperative hydrocephalus in cranial base surgery. Skull Base Surg. 2000. 10: 197-200
12. Falcioni M, Romano G, Aggarwal N, Sanna M. Cerebrospinal fluid leak after retrosigmoid excision of vestibular schwannomas. Otol Neurotol. 2008. 29: 384-6
13. Fishman AJ, Marrinan MS, Golfinos JG, Cohen NL, Roland JT. Prevention and management of cerebrospinal fluid leak following vestibular schwannoma surgery. Laryngoscope. 2004. 114: 501-5
14. Hoffman RA. Cerebrospinal fluid leak following acoustic neuroma removal. Laryngoscope. 1994. 104: 40-58
15. Khrais TH, Falcioni M, Taibah A, Agarwal M, Sanna M. Cerebrospinal fluid leak prevention after translabyrinthine removal of vestibular schwannoma. Laryngoscope. 2004. 114: 1015-20
16. Legnani FG, Saladino A, Casali C, Vetrano IG, Varisco M, Mattei L. Craniotomy vs craniectomy for posterior fossa tumors: A prospective study to evaluate complications after surgery. Acta Neurochir (Wien). 2013. 155: 2281-6
17. Ling PY, Mendelson ZS, Reddy RK, Jyung RW, Liu JK. Reconstruction after retrosigmoid approaches using autologous at graft-assisted Medpor Titan cranioplasty: Assessment of postoperative cerebrospinal fluid leaks and headaches in 60 cases. Acta Neurochir (Wien). 2014. 156: 1879-88
18. Mangham CA. Retrosigmoid versus middle fossa surgery for small vestibular schwannomas. Laryngoscope. 2004. 114: 1455-61
19. Montano N, Giordano M, Caccavella VM, Ioannoni E, Polli FM, Papacci F. Hemopatch® with fibrin glue as a Dural sealant in cranial and spinal surgery. A technical note with a review of the literature. J Clin Neurosci. 2020. 79: 144-7
20. Ojemann RG. Retrosigmoid approach to acoustic neuroma (vestibular schwannoma). Neurosurgery. 2001. 48: 553-8
21. Ou C, Chen Y, Mo J, Wang S, Gai S, Xing R. Cranioplasty using polymethylmethacrylate cement following retrosigmoid craniectomy decreases the rate of cerebrospinal fluid leak and pseudomeningocele. J Craniofac Surg. 2019. 30: 566-70
22. Pabaney AH, Reinard KA, Asmaro K, Malik GM. Novel technique for cranial reconstruction following retrosigmoidcraniectomy using demineralized bone matrix. Clin Neurol Neurosurg. 2015. 136: 66-70
23. Park JS, Kong DS, Lee JA, Park K. Intraoperative management to prevent cerebrospinal fluid leakage after microvascular decompression: Dural closure witha plugging muscle method. Neurosurg Rev. 2007. 30: 139-42
24. Samii M, Gerganov VM, Samii A. Functional outcome after complete surgical removal of giant vestibular schwannomas. J Neurosurg. 2010. 112: 860-7
25. Selesnick SH, Liu JC, Jen A, Newman J. The incidence of cerebrospinal fluid leak after vestibular schwannoma surgery. Otol Neurotol. 2004. 25: 387-93
26. Shew M, Muelleman T, Harris M, Li M, Sykes K, Staecker H. Petrous apex pneumatization: Influence on postoperative cerebellopontine angle tumor cerebrospinal fluid fistula. Ann Otol Rhinol Laryngol. 2018. 127: 604-7
27. Stieglitz LH, Wrede KH, Gharabaghi A, Gerganov VM, Samii A, Samii M. Factors affecting postoperative cerebrospinal fluid leaks after retrosigmoidal craniotomy for vestibular schwannomas. J Neurosurg. 2009. 111: 874-83
28. Sugerman HJ, DeMaria EJ, Felton WL, Nakatsuka M, Sismanis A. Increased intra-abdominal pressure and cardiac filling pressures in obesity-associated pseudotumor cerebri. Neurology. 1997. 49: 507-11
29. Teo MK, Eljamel MS. Role of craniotomy repair in reducing postoperative headaches after a retrosigmoid approach. Neurosurgery. 2010. 67: 1286-91
30. Venable GT, Roberts ML, Lee RP, Michael LM 2nd. Primary dural closure for retrosigmoid approaches. J Neurol Surg B Skull Base. 2018. 79: 330-4