- Department of Pediatric Neurosurgery, Instituto Materno Infantil Professor Fernando Figueira-IMIP and Department of Neurosurgery, Hospital da Restauracao, Recife, Brazil.
- Department of Neurosurgery, HU-Univasf and IMIP-Petrolina, Recife, Brazil.
- Department of Neurosurgery, Hospital da Restauracao, Recife, Pernambuco, Brazil.
Correspondence Address:
Ricardo Brandão Fonseca, Department of Neurosurgery, HU-Univasf, Petrolina, Pernambuco, Brazil.
DOI:10.25259/SNI_458_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Igor Vilela Faquini1, Ricardo Brandão Fonseca2, Alyne Oliveira Correia2, Auricelio Batista Cezar Junior1, Eduardo Vieira De Carvalho Junior3, Nivaldo Sena de Almeida3, Hildo Rocha Cirne Azevedo-Filho3. Endoscopic third ventriculostomy in the treatment of hydrocephalus: A 20-year retrospective analysis of 209 consecutive cases. 03-Aug-2021;12:383
How to cite this URL: Igor Vilela Faquini1, Ricardo Brandão Fonseca2, Alyne Oliveira Correia2, Auricelio Batista Cezar Junior1, Eduardo Vieira De Carvalho Junior3, Nivaldo Sena de Almeida3, Hildo Rocha Cirne Azevedo-Filho3. Endoscopic third ventriculostomy in the treatment of hydrocephalus: A 20-year retrospective analysis of 209 consecutive cases. 03-Aug-2021;12:383. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11021
Abstract
Background: Endoscopic third ventriculostomy (ETV) has been shown to be a sufficient alternative to shunts in surgical treatment of obstructive hydrocephalus. Long-term failure, age limitations, and outcome by cause are some of the issues debated in literature. The objective of this article is to analyze the clinical success and failure of ETV and its main complications.
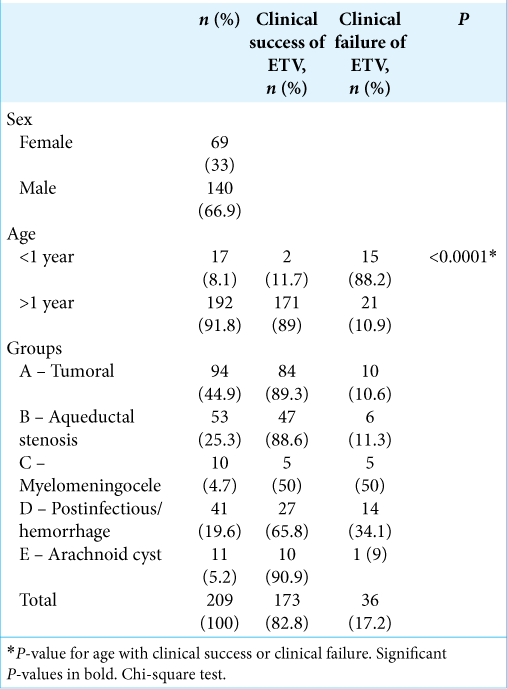
Methods: A total of 209 patients with hydrocephalus were submitted to ETV, including a mixed population of children and adults (from 0 to 59 years). Patients were divided into five groups: A – tumors, B – aqueductal stenosis, C – myelomeningocele, D – infection and hemorrhage, and E – arachnoid cyst. Variables were analyzed: age, ETV success rate, cerebrospinal fluid (CSF) fistula, mortality, and complications.
Results: The two main causes of hydrocephalus were tumors (44.9%) and aqueductal stenosis (25.3%). The overall success rate was of 82.8%, and patients in Group E had the highest rate 90.9%. Group A had a success rate of 89.3%, and Group B had a rate of 88.6%. The ETV success rate was significantly higher in patients older than 1 year (P P
Conclusion: Better results were observed in the groups of patients with tumors, aqueductal stenosis, and arachnoid cysts, while those whose primary causes of hydrocephalus were myelomeningocele, infections, or bleeding had higher rates of failure after the procedure. This study demonstrated that age under 1 year and hydrocephalus caused by myelomeningocele, bleeding, and infection were considered independent risk factors of poor prognosis in ETV.
Keywords: Endoscopic third ventriculostomy, Hydrocephalus, Posterior fossa tumor, Treatment outcome
INTRODUCTION
Hydrocephalus is a pathology caused by excessive increase in the amount of cerebrospinal fluid (CSF) in the brain ventricles, thus increasing intracranial pressure and injuring the brain. In Brazil, the occurrence of hydrocephalus is reported in 1–3 of every 1000 live births. Moreover, approximately 60% of cases affect newborns, whereas approximately 40% of cases are in elderly patients, and it is more likely to develop in the male sex.[
In pediatric patients, hydrocephalus continues to be one of the most recurrent causes of admission to pediatric neurosurgery units. In 1923, William Jason Mixter demonstrated that endoscopic fenestration of the floor of the third ventricle could successfully treat congenital hydrocephalus, thus giving rise to endoscopic third ventriculostomy (ETV) as a therapeutic approach to hydrocephalus, avoiding extracranial shunts.[
ETV is an intracerebral surgery performed by the neuroendoscopic approach, which makes it possible to divert the flow of CSF trapped in the ventricles to the subarachnoid cisterns. The efficiency of ETV has frequently been described in the literature, and it is dependent on correct surgical indication.[
In 1994, ETV was adopted as an important tool for the treatment of children and adults with hydrocephalus in two leading neurosurgical centers located in the Northeast Region of Brazil. The objective of this article is to analyze the clinical success and failure of ETV and its main complications.
MATERIALS AND METHODS
From April 1994 to June 2014, 209 patients with hydrocephalus (140 males, 66.9%, and 69 females, 33%) were submitted to ETV at the Hospital da Restauração and the Professor Fernando Figueira Integral Medicine Institute. All patients diagnosed with hydrocephalus operated by ETV in the mentioned period were included in the study. No patients were excluded from this study. We performed magnetic resonance imaging preoperatively in 60% of patients, and the remaining cases were diagnosed by computed tomography. Follow-up ranged from 1 to 98 months, with an average of 19.2 months. Postoperative control magnetic resonance imaging was performed in 80% of cases. Based on hydrocephalus etiology, patients were divided into the following five groups: Group A – tumors, Group B – aqueductal stenosis, Group C – myelomeningocele, Group D – infection or hemorrhage, and Group E – arachnoid cysts (posterior cranial fossa cysts).
The patients included in this study had intracranial hypertension with Cushing’s triad (hypertension, bradycardia, and irregular breathing rhythm) and/or symptoms such as vomiting, headache, and altered level of consciousness, and, in children, aspects such as bulging of the anterior fontanelle, increased head circumference, engorgement of superficial veins, and other clinical signs. Choice of surgical treatment was discussed and evaluated on a case-by-case basis. The criteria used to evaluate success of treatment with ETV were clinical improvement and shunt independence (clinical success), with disappearance of initial symptoms, in conjunction with confirmation by imaging examination (magnetic resonance in 80% of cases), in accordance with the Canadian Pediatric Study Group.[
Characteristics of patients
The main results are summarized in [
Endoscopic technique
All surgeries were performed using a 0° rigid endoscope (Aesculap, 2.7 mm diameter). The head was flexed at 30° and trepanation was performed at Kocher’s point. The puncture cannula was inserted by the freehand technique, and it was never fixed during the procedure.
The floor of the third ventricle was perforated and dilated with a 4 Fr Fogarty balloon catheter. Following dilation, the endoscope was advanced toward the opening to visualize structures of the prepontine cistern and to confirm perforation of the Liliequist membrane. Hemostasis of the puncture tunnel was obtained with Surgicel®. Surgery concluded with the closure of subcutaneous and epidermal layers.[
It worth underscoring that perforation of the Liliequist membrane is considered essential to a successful procedure. In ETV, after opening the tuber cinereum, the underlying structure is the Liliequist membrane, which is the upper limit of the interpeduncular cistern. If the membrane is not opened, communication between the ventricular system and the subarachnoid system is not achieved, in which case, the operation is not completed and is ineffective.[
Statistical analysis
All data were collected from patients’ medical files in a retrospective cohort study. Statistical analysis was carried out using IBM SPSS version 20 (IBM Corp., Charlotte, NC, USA) and Prism 5.0 GraphPad (GraphPad Software Inc., La Jolla, CA, USA). Frequency tests were performed to determine percentages; Chi-square test (χ2) was used to analyze categorical variables. Results were considered significant at P < 0.05.
RESULTS
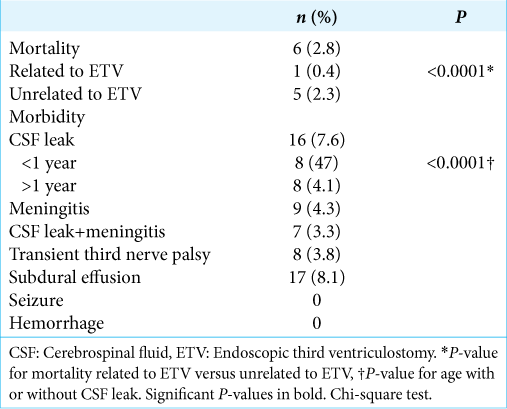
Morbidity/Mortality
The main results are summarized in [
Prognosis after ETV
Average duration of follow-up was 19.2 months (ranging from 1 to 98 months).
During this period, overall success rate (clinical success) was 82.8% (173 patients). No procedure was aborted due to bleeding or anatomical variations. The method proved ineffective in 17.2% (36 patients) of cases, and all of those were submitted to a ventriculoperitoneal shunt.
Taken alone, patients in Group E (arachnoid cysts) had the highest success rate, namely, 90.9%. Patients in Group A had a success rate of 89.3%, and patients in Group B had a rate of 88.6%.
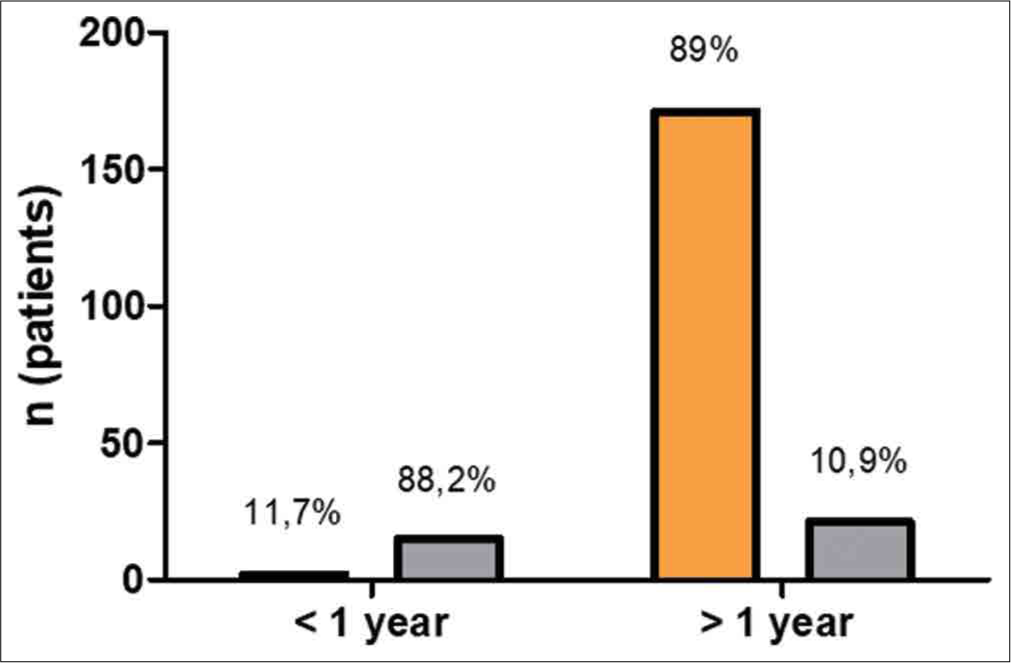
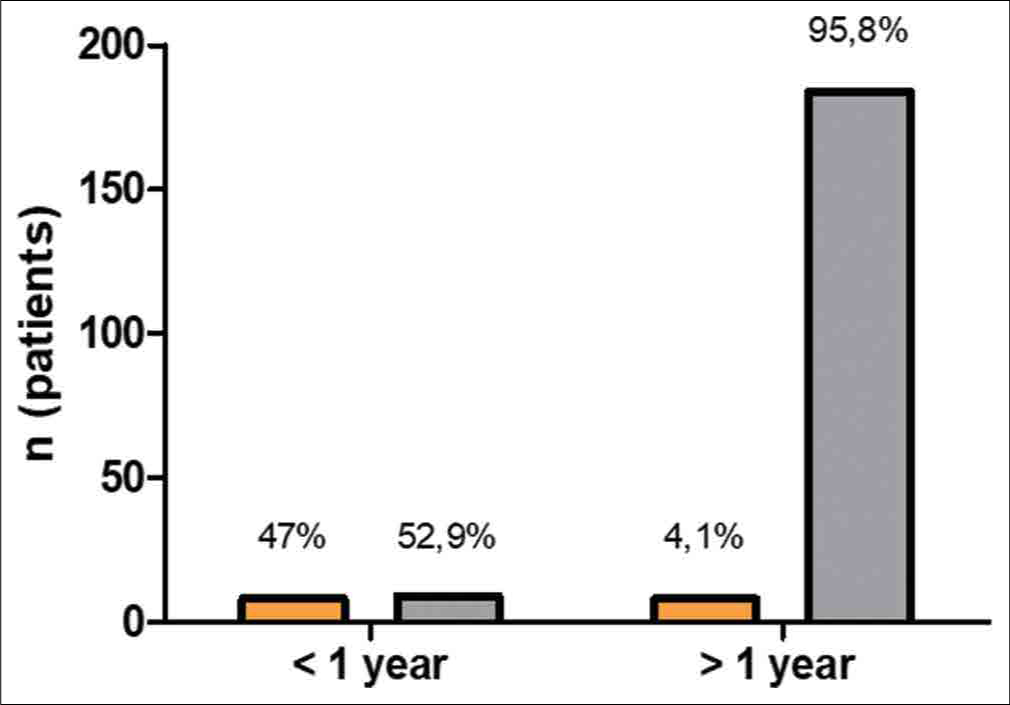
Patients older than 1 year had a significantly higher success rate in relation to those younger than 1 year of age (P < 0.001) [
DISCUSSION
ETV has been established as the treatment of choice for cases of obstructive hydrocephalus in recent years. The need for equipment and know-how makes its dissemination throughout multiple centers in developing countries challenge that still needs to be overcome. It is worth emphasizing that the endoscopic technique reduces costs,[
In the present study, we did not perform ventricular measurements after endoscopy; however, there are conflicts in the literature regarding the fact that no decrease in ventricular size after ETV may or may not affect patients’ cognitive development. Sainte-Rose and Chumas[
It should be borne in mind that, in cases of hydrocephalus secondary to posterior fossa tumors, and some cases of secondary aqueductal stenosis, treatment of the primary cause can, by itself, lead to an improvement of hydrocephalus, and the ETV success rate may, therefore, be overestimated. The success of ETV depends on several factors, and the cause of hydrocephalus (obstructive or communicating) is only one among many. Age has also been identified as a watershed in indications for endoscopic treatment. In our study, we found better results in patients older than 1 year of age, with favorable prognosis occurring in 89% (171 cases), in comparison with only 11.7% (2 cases) among those under 1 year of age. These data corroborate those obtained by Kim et al.[
Kulkarni et al.[
Within this panorama, Gorgoglione et al.[
In the present study, the incidence of CSF leakage was 47% (8 cases) of patients younger than 1 year old. Val (2009) published a study using minicraniotomy for ETV, minimizing the occurrence of CSF fistula and subgaleal collections in very young babes. This technique can be implemented in our future cases, without modifying the duration, safety, and efficacy of the procedure.[
Texakalidis et al.[
A substantial discussion has been raised by studies demonstrating that better prognosis is linked not to age per se, but rather to the cause of hydrocephalus. In our opinion, both factors seem to contribute significantly to the success or failure of endoscopy in this population. In children, the presence of immaturity in CSF absorption pathways and the emergence of new arachnoid membranes may contribute to the high rate of treatment failure.[
Notwithstanding the potential occurrence of technical failures inherent to the method, endoscopy has accomplished its mission as an excellent alternative for keeping thousands of patients free from ventriculoperitoneal shunts, especially in the context of a developing nation like Brazil, where malnutrition, poor access to specialized neurosurgical services, and lack of health-care resources are still present in some regions.
Cinalli et al.[
Procedure failures can be classified as early or late, according to time after endoscopy. Early failures are assessed when the patient continues to have intracranial hypertension, as the CSF absorption system is still in the adaptive period due to new drainage conditions, which can last weeks or possibly months. The use of serial lumbar punctures (up to 3 times weekly) and inhibitors of carbonic anhydrase for short periods seems to favor better outcome in cases with reabsorption difficulties (effusion in place of trepanation, low output fistulas, or even mildly symptomatic patients).[
Late failures generally result from either scarification or gliosis in the area of the stoma or in the basal cisterns (most commonly in children), and the causes are still speculative (reduced CSF flow and/or change in differential pressure). As stated by Drake et al.,[
CONCLUSION
Notwithstanding the need for a specific learning curve and materials with considerably high prices, the use of ETV has served to reduce the costs generated by numerous revision surgeries following shunt placement and also to lower average hospital stay. Age (<1 year) and the primary cause of hydrocephalus were isolated prognostic factors for the outcome of ETV.
Better results were observed in the groups of patients with tumors, aqueductal stenosis, and arachnoid cysts, while those whose primary causes of hydrocephalus were myelomeningocele, infections, or bleeding had higher rates of failure after the procedure.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beems T, Grotenhuis JA. Is the success rate of endoscopic third ventriculostomy age-dependent? An analysis of the results of endoscopic third ventriculostomy in young children. Childs Nerv Syst. 2002. 18: 605-8
2. César J, Ramos R, Ramos MR, Apparecido MM, Ramos GR. Hidrocefalia aguda: Uma revisão bibliográfica/Acute hydrocephalus: A bibliographic review. Rev Salusvita. 2018. 37: 1019-28
3. Cinalli G, Spennato P, Ruggiero C, Aliberti F, Trischitta V, Buonocore MC. Complications following endoscopic intracranial procedures in children. Childs Nerv Syst. 2007. 23: 633-44
4. Costa Val JA. Minicraniotomy for endoscopic third ventriculostomy in babes: Technical note with a 7-year-segment analysis. Childs Nerv Syst. 2009. 25: 357-9
5. Demerdash A, Rocque BG, Johnston J, Rozzelle CJ, Yalcin B, Oskouian R. Endoscopic third ventriculostomy: A historical review. Br J Neurosurg. 2017. 31: 28-32
6. Drake J, Chumas P, Kestle J, Pierre-Kahn A, Vinchon M, Brown J. Late rapid deterioration after endoscopic third ventriculostomy: Additional cases and review of the literature. J Neurosurg. 2006. 105: 118-26
7. Drake JM. Endoscopic third ventriculostomy in pediatric patients: The Canadian experience. Neurosurgery. 2007. 60: 881-6
8. Gorayeb RP, Cavalheiro S, Zymberg ST. Endoscopic third ventriculostomy in children younger than 1 year of age. J Neurosurg. 2004. 100: 427-9
9. Gorgoglione N, Fazzari E, Alafaci C, Vitulli F, Zaccaria R, Angileri FF. An unusual but possible complication after endoscopic third ventriculostomy. World Neurosurg. 2021. 146: 287-91
10. Grunert P, Charalampaki P, Hopf N, Filippi R. The role of third ventriculostomy in the management of obstructive hydrocephalus. Minim Invasive Neurosurg. 2003. 46: 16-21
11. Hopf NJ, Grunert P, Fries G, Resch KD, Perneczky A. Endoscopic third ventriculostomy: Outcome analysis of 100 consecutive procedures. Neurosurgery. 1999. 44: 795-804
12. Kadrian D, van Gelder J, Florida D, Jones R, Vonau M, Teo C. Long-term reliability of endoscopic third ventriculostomy. Neurosurgery. 2005. 56: 1271-8
13. Kim SK, Wang KC, Cho BK. Surgical outcome of pediatric hydrocephalus treated by endoscopic III ventriculostomy: Prognostic factors and interpretation of postoperative neuroimaging. Childs Nerv Syst. 2000. 16: 161-8
14. Kulkarni AV, Riva-Cambrin J, Butler J, Browd SR, Drake JM, Holubkov R. Outcomes of CSF shunting in children: Comparison of hydrocephalus clinical research network cohort with historical controls. J Neurosurg Pediatr. 2013. 12: 334-8
15. Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E, Mugamba J, Ssenyonga P, Donnelly R. Endoscopic treatment versus shunting for infant hydrocephalus in Uganda. N Engl J Med. 2017. 377: 2456-64
16. Madsen PJ, Mallela AN, Hudgins ED, Storm PB, Heuer GG, Stein SC. The effect and evolution of patient selection on outcomes in endoscopic third ventriculostomy for hydrocephalus: A large-scale review of the literature. J Neurol Sci. 2018. 385: 185-91
17. Martins FJ, Beserra NC, Barbosa LG. Clinical and epidemiological profile of children hospitalized by hydrocephalia in a municipal hospital of São Paulo in the period 2014 to 2016. Rev Bras Neurol. 2018. 54: 25-31
18. McLaughlin MR, John BW, Kaufmann AM, Albright AL. Traumatic basilar aneurysm after endoscopic third ventriculostomy: Case report. Neurosurgery. 1997. 41: 1400-3
19. Sacko O, Boetto S, Lauwers-Cances V, Dupuy M, Roux FE. Endoscopic third ventriculostomy: Outcome analysis in 368 procedures. J Neurosurg Pediatr. 2010. 5: 68-74
20. Sainte-Rose C, Chumas P. Endoscopic third ventriculostomy. Tech Neurosurg. 1995. 1: 176-84
21. Sainte-Rose C, Cinalli G, Roux FE, Maixner W, Chumas PD, Mansour M. Management of hydrocephalus in pediatric patients with posterior fossa tumors: The role of endoscopic third ventriculostomy. J Neurosurg. 2001. 95: 791-7
22. Texakalidis P, Tora MS, Wetzel JS, Chern JJ. Endoscopic third ventriculostomy versus shunt for pediatric hydrocephalus: A systematic literature review and meta-analysis. Childs Nerv Syst. 2019. 35: 1283-93
23. Val Filho JA.editors. O Papel da Membrana de “Liliequist” na Terceiro Ventriculostomia Endoscópica (Doctoral Dissertation). Brazil: Universidade Federal de Minas Gerais; 2018. p.