- Department of Orthopedics, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
- Department of Medicine, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
- Department of Orthopedics, Railway Hospital, Mumbai, Maharashtra, India.
- Department of Spine Services, Indian Spinal Injuries Centre, New Delhi, Delhi, India.
Correspondence Address:
Pauras Pritam Mhatre, Department of Medicine, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_679_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nandan Marathe1, Pauras Pritam Mhatre2, Shubhanshu Bhaladhare1, Aditya Dahapute1, Ayush Sharma3, Abhinandan Reddy Mallepally4. Plain roentgenographic and CT scan morphometric analysis of the anterior atlantodens interval (AADI) and posterior atlantodens interval (PADI) in the Indian population. 24-Aug-2021;12:427
How to cite this URL: Nandan Marathe1, Pauras Pritam Mhatre2, Shubhanshu Bhaladhare1, Aditya Dahapute1, Ayush Sharma3, Abhinandan Reddy Mallepally4. Plain roentgenographic and CT scan morphometric analysis of the anterior atlantodens interval (AADI) and posterior atlantodens interval (PADI) in the Indian population. 24-Aug-2021;12:427. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11055
Abstract
Background: The anterior atlantodental interval (AADI) and posterior atlantodental interval (PADI) on X-ray and computed tomography (CT) studies can both be used to gauge the risk and/or presence of neurological compression.
Methods: This retrospective observational study was conducted at a tertiary care center in 116 patients with head injuries additionally warranting routine cervical X-ray and CT examinations.
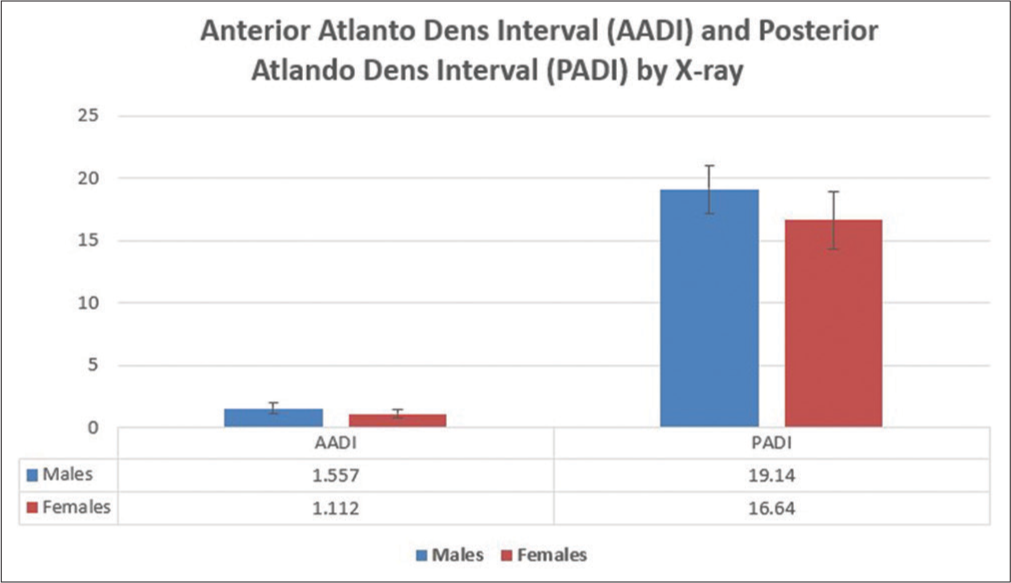
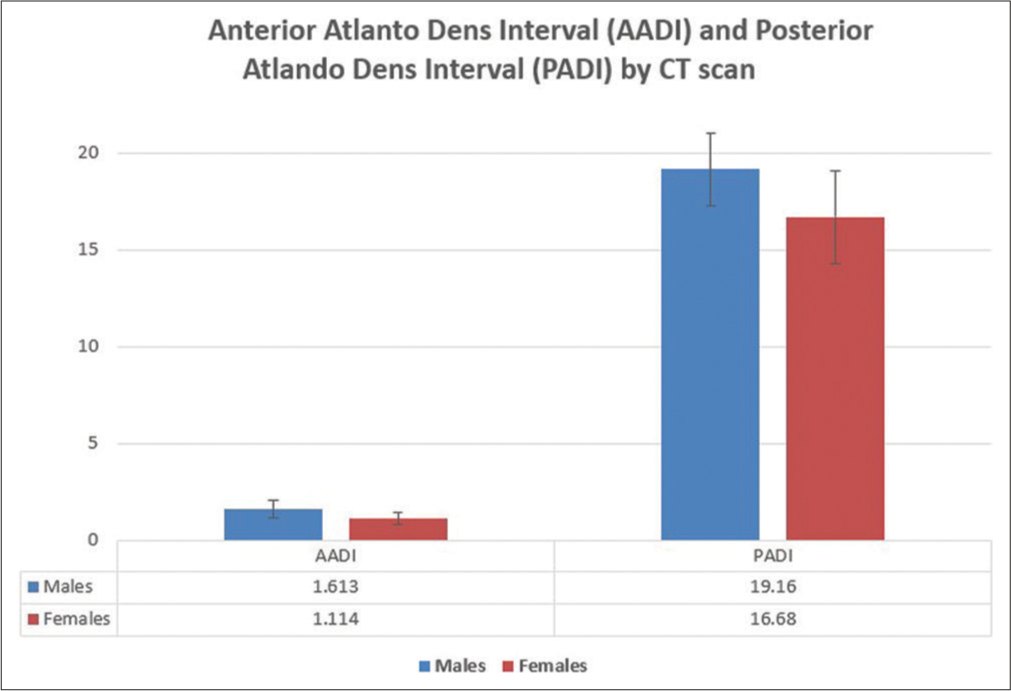
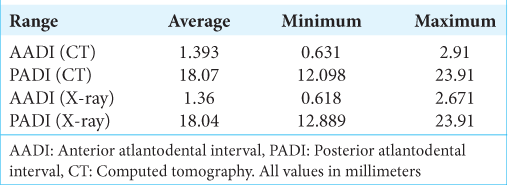
Results: The AADI averaged 1.36 ± 0.45 mm (X-ray) and 1.393 ± 0.47 mm (CT), while the mean PADI was 18.04 ± 2.44 mm (X-ray), and 18.07 ± 2.43 mm (CT). Notably, 93.96% of the total subjects had AADI below 2 mm. Further, 6.8% of patients with PADI =/
Conclusion: No significant differences were observed for X-ray versus CT studies, measuring AADI and PADI. Therefore, X-rays should continue to prove reliable for assessing craniovertebral junction anatomy in emergency settings. Of interest, the normal upper limit of AADI on sagittal CT reconstructions should now be changed to 2 mm from the previously accepted upper limit of 3 mm.
Keywords: Atlantodens interval, Cervical spine, Morphometry
INTRODUCTION
An anterior atlantodental interval (AADI) of more than 10 mm is clinically significant as it suggests transverse ligament rupture and the normal upper limit of normal in adults is 3 mm.[
MATERIALS AND METHODS
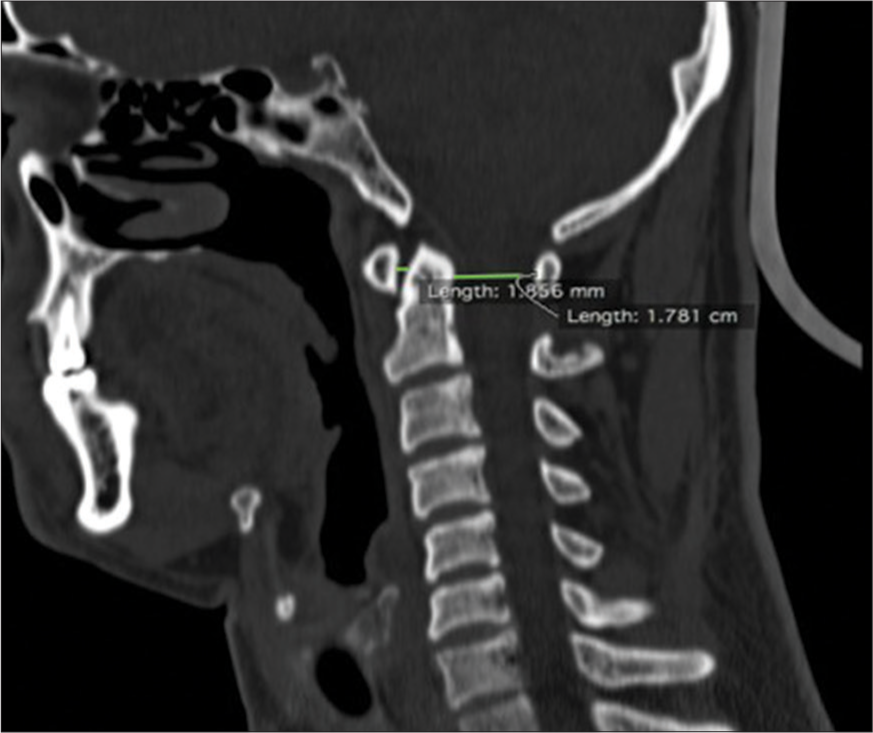
There were 116 patients with head injuries who underwent cervical X-rays and CT scans in this study. Films were independently evaluated by two orthopedic surgeons who similarly measured AADI and PADI on plain radiographs versus CT scans [
RESULTS
AADI ranged from 1.36 ± 0.45 mm on X-rays to 1.393 ± 0.47 mm on CT scans, while PADI varied from 18.04 ± 2.44 mm on X-rays to 18.07 ± 2.43 mm on CT scans [
DISCUSSION
The values of AADI and PADI obtained in the present study differed significantly from the previously published values based on standard plain radiographs. We found that the differences in measurements of AADI and PADI made on X-ray and CT scans were not statistically significant. Therefore, X-rays are reliable for assessing the CVJ anatomy in emergency scenarios, especially where CT scans are not available.
Rojas et al.[
Chen et al. studied the AADI in a normal Chinese population using CT;[
Liu et al.[
Boden et al.[
CONCLUSION
We found the normal upper limit of AADI on sagittal CT scans was 2 mm versus the previously accepted 3 mm. Further, there can be patients with a PADI below 14 mm who have no neurological symptoms.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine: A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993. 75: 1282-97
2. Chen Y, Zhuang Z, Qi W, Yang H, Chen Z, Wang X. A three-dimensional study of the atlantodental interval in a normal Chinese population using reformatted computed tomography. Surg Radiol Anat. 2011. 33: 801-6
3. Hinck VC, Hopkins CE. Measurement of the atlanto-dental interval in the adult. AJR Am J Roentgenol. 1960. 84: 945
4. Liu K, Xie F, Wang D, Guo L, Qi Y, Tian J, Zhao B, Chhabra A. Reference ranges for atlantodental interval in adults and its variation with age and gender in a large series of subjects on multidetector computed tomography. Acta Radiol. 2015. 56: 465-70
5. Rojas CA, Bertozzi JC, Martinez CR, Whitlow J. Reassessment of the craniocervical junction: Normal values on CT. AJNR Am J Neuroradiol. 2007. 28: 1819-23