- Department of Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Enyinna Nwachuku, Department of Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
DOI:10.25259/SNI_748_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Enyinna Nwachuku, Confidence Njoku-Austin, Kevin P. Patel, Austin W. Anthony, Aditya Mittal, David Kojo Hamilton, Adam Kanter, Peter C. Gerszten, David Okonkwo. Isolated traumatic occipital condyle fractures: Is external cervical orthosis even necessary?. 19-Oct-2021;12:524
How to cite this URL: Enyinna Nwachuku, Confidence Njoku-Austin, Kevin P. Patel, Austin W. Anthony, Aditya Mittal, David Kojo Hamilton, Adam Kanter, Peter C. Gerszten, David Okonkwo. Isolated traumatic occipital condyle fractures: Is external cervical orthosis even necessary?. 19-Oct-2021;12:524. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11188
Abstract
Background: Occipital condyle fractures (OCFs) have been reported in up to 4–16% of individuals suffering cervical spine trauma. The current management of OCF fractures relies on a rigid cervical collar for 6 weeks or longer. Here, we calculated the rate of acute and delayed surgical intervention (occipitocervical fusion) for patients with isolated OCF who were managed with a cervical collar over a 10-year period at a single institution.
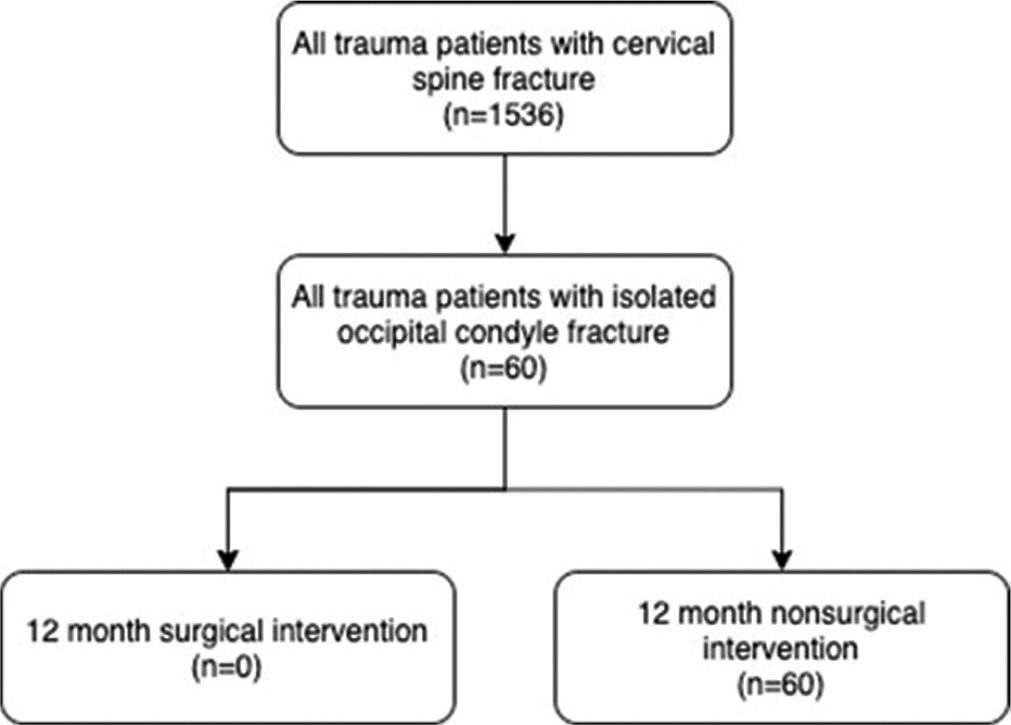
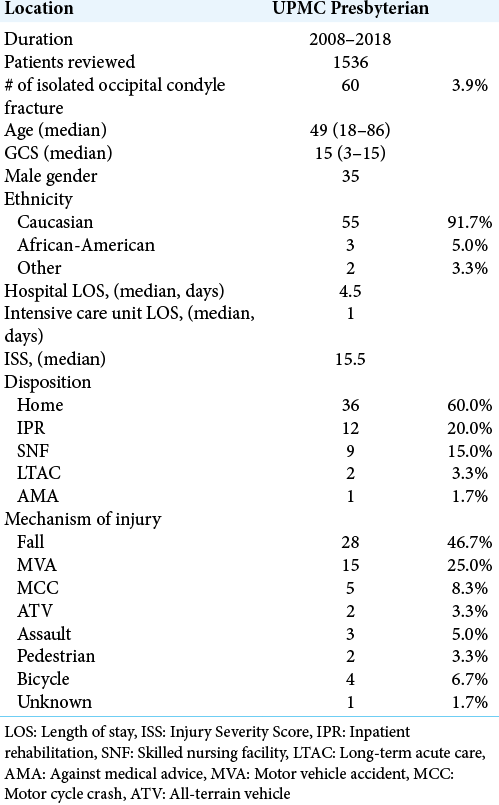
Methods: This was a retrospective analysis performed on all patients admitted to a Level 1 Trauma Center between 2008 and 2018 who suffered traumatic isolated OCF managed with an external rigid cervical orthosis. Radiographic imaging was reviewed by several board-certified neuroradiologists. Demographic and clinical data were collected including need for occipitocervical fusion within 12 months after trauma.
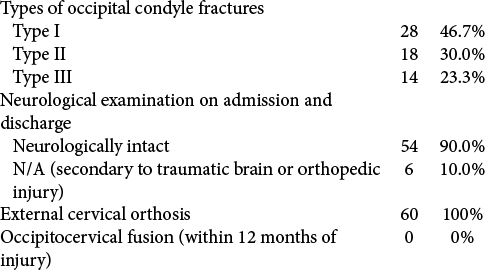
Results: The incidence of isolated OCF was 4% (60/1536) for those patients admitted with cervical spine fractures. They averaged 49 years of age, and 58% were male falls accounted for the mechanism of injury in 47% of patients. Classification of OCF was most commonly classified in 47% as type I Anderson and Montesano fractures. Of the 60 patients who suffered isolated OCF that was managed with external cervical orthosis, 0% required occipitocervical fusion within 12 months posttrauma. About 90% were discharged, while the remaining 10% sustained traumatic brain/orthopedic injury that limited an accurate neurological assessment.
Conclusion: Here, we documented a 4% incidence of isolated OCF in our cervical trauma population, a rate which is comparable to that found in the literature year. Most notably, we documented a 0% incidence for requiring delayed occipital-cervical fusions.
Keywords: Arthrodesis, Fractures, Occipital condyle, Orthosis, Trauma
INTRODUCTION
Occipital condyle fractures (OCFs) have been reported in up to 4–16% of individuals sustaining cervical spine trauma.[
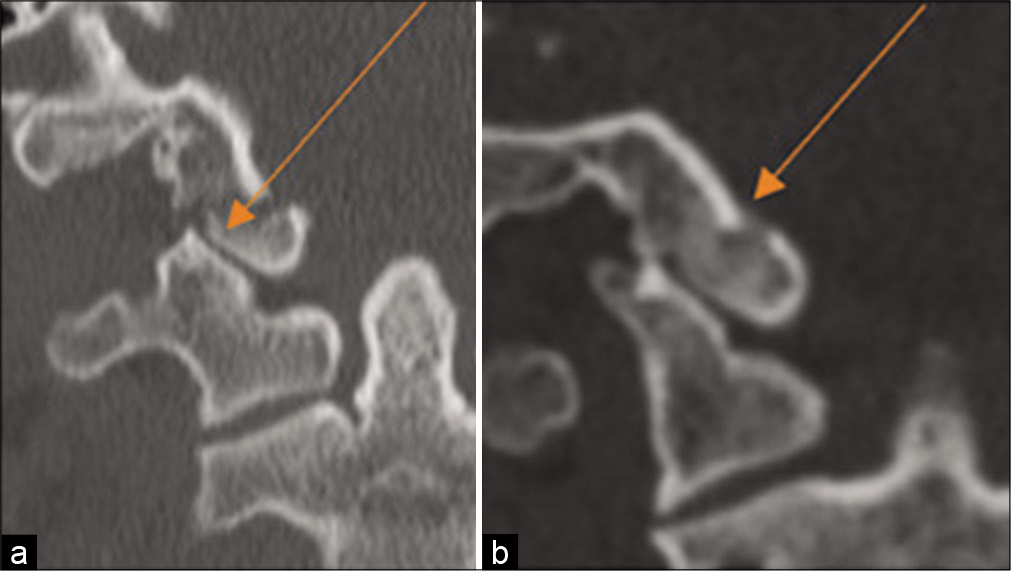
Figure 3:
(a) A 42-year-old female motor cycle crash (MCC) with left Type II occipital condyle fracture with concomitant TBI, GCS 7T. (b) One-month interval CT cervical spine – a 42-year-old female MCC with left Type II occipital condyle fracture with concomitant TBI, GCS 7T with early signs of cortication of fracture line.
The current practice guidelines typically support management of patients with OCF with a cervical collar for approximately 6 weeks or longer.[
Here, we analyzed the rate of delayed surgical intervention (occipitocervical fusion) warranted in patients with isolated OCF who were managed with a rigid cervical collar for 6 weeks or longer at a high-volume Level 1 Trauma Center over a 10-year period.
MATERIALS AND METHODS
All patients admitted to UPMC Presbyterian Hospital with OCF were analyzed from 2008 to 2018. All patients sustained an isolated traumatic OCF without other traumatic cervical injury [
RESULTS
Of the 1536 patients reviewed, 60 cases (4%) had OCF over the 10-year period [
DISCUSSION
Isolated OCFs are found in only 4% of cervical trauma series. At present, most individuals with OCF are managed with a cervical collar (external orthosis).[
In our cohort, no patient required surgery acutely or in delayed fashion to address occipitocervical instability or pseudoarthrosis. In addition, patients who were not limited by a TBI or other orthopedic injury were admitted and discharged with a normal neurological examination demonstrating that this fracture pattern poses very little to no risk of neurological injury in isolation.
Notably, rigid external cervical orthosis is associated with risk and complications that include aspiration pneumonia, limitation in driving, and/or other nonstrenuous activities of daily living, pressure ulcers, and cellulitis that can lead to bacteremia and possibly sepsis in vulnerable individuals.[
CONCLUSION
Sixty (4%) patients had isolated OCF out of 1536 patients presenting with traumatic cervical injuries, and none required acute and/or delayed occipital-cervical surgical fusions. Although historically, these fractures are primarily managed with an external cervical orthosis (C-collar), these findings provide a platform for prospective analysis comparing collar versus no-collar management for isolated OCF.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to give gratitude to the University of Pittsburgh Medical Center for providing the cohort for this manuscript.
References
1. Ackland HM, Cooper DJ, Malham GM, Kossmann T. Factors predicting cervical collar-related decubitus ulceration in major trauma patients. Spine (Phila Pa 1976). 2007. 32: 423-8
2. Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976). 1988. 13: 731-6
3. Barkana Y, Stein M, Scope A, Maor R, Abramovich Y, Friedman Z. Prehospital stabilization of the cervical spine for penetrating injuries of the neck-is it necessary?. Injury. 2000. 31: 305-9
4. Byström O, Jensen TS, Poulsen FR. Outcome of conservatively treated occipital condylar fractures-a retrospective study. J Craniovertebr Junction Spine. 2017. 8: 322-7
5. Connell RA, Graham CA, Munro PT. Is spinal immobilisation necessary for all patients sustaining isolated penetrating trauma?. Injury. 2003. 34: 912-4
6. Ham W, Schoonhoven L, Schuurmans MJ, Leenen LP. Pressure ulcers from spinal immobilization in trauma patients: A systematic review. J Trauma Acute Care Surg. 2014. 76: 1131-41
7. Hanson JA, Deliganis AV, Baxter AB, Cohen WA, Linnau KF, Wilson AJ. Radiologic and clinical spectrum of occipital condyle fractures: Retrospective review of 107 consecutive fractures in 95 patients. AJR Am J Roentgenol. 2002. 178: 1261-8
8. Haut ER, Kalish BT, Efron DT, Haider AH, Stevens KA, Kieninger AN. Spine immobilization in penetrating trauma: More harm than good?. J Trauma. 2010. 68: 115-20
9. Holla M. Value of a rigid collar in addition to head blocks: A proof of principle study. Emerg Med J. 2012. 29: 104-7
10. Houghton DJ, Curley JW. Dysphagia caused by a hard cervical collar. Br J Neurosurg. 1996. 10: 501-2
11. Karam YR, Traynelis VC. Occipital condyle fractures. Neurosurgery. 2010. 66: 56-9
12. Kelly A, Parrish R. Fracture of the occipital condyle: The forgotten part of the neck. J Accid Emerg Med. 2000. 17: 220-1
13. Leone A, Cerase A, Colosimo C, Lauro L, Puca A, Marano P. Occipital condylar fractures: A review. Radiology. 2000. 216: 635-44
14. Lockey DJ, Coats T, Parr MJ. Aspiration in severe trauma: A prospective study. Anaesthesia. 1999. 54: 1097-8
15. Maserati MB, Stephens B, Zohny Z, Lee JY, Kanter AS, Spiro RM. Occipital condyle fractures: Clinical decision rule and surgical management. J Neurosurg Spine. 2009. 11: 388-95
16. Musbahi O, Khan AH, Anwar MO, Chaudery H, Ali AM, Montgomery AS. Immobilisation in occipital condyle fractures: A systematic review. Clin Neurol Neurosurg. 2018. 173: 130-9
17. Shem K, Castillo K, Wong SL, Chang J, Kolakowsky-Hayner S. Dysphagia and respiratory care in individuals with tetraplegia: Incidence, associated factors, and preventable complications. Top Spinal Cord Inj Rehabil. 2012. 18: 15-22
18. Tomaszewski R, Wiktor Ł. Occipital condyle fractures in adolescents. Ortop Traumatol Rehabil. 2015. 17: 219-27
19. Velopulos CG, Shihab HM, Lottenberg L, Feinman M, Raja A, Salomone J. Prehospital spine immobilization/ spinal motion restriction in penetrating trauma: A practice management guideline from the eastern association for the surgery of trauma (EAST). J Trauma Acute Care Surg. 2018. 84: 736-44
20. Webber-Jones JE, Thomas CA, Bordeaux RE. The management and prevention of rigid cervical collar complications. Orthop Nurs. 2002. 21: 19-25