- Department of Neurosurgery, Royal North Shore Hospital, St Leonards, New South Wales, Australia.
Correspondence Address:
Ragavan Manoharan, Department of Neurosurgery, Royal North Shore Hospital, St Leonards, New South Wales, Australia.
DOI:10.25259/SNI_805_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ragavan Manoharan, Jonathon Parkinson. Pure epidural spinal cavernous haemangioma. 19-Oct-2021;12:523
How to cite this URL: Ragavan Manoharan, Jonathon Parkinson. Pure epidural spinal cavernous haemangioma. 19-Oct-2021;12:523. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11189
Abstract
Background: Pure epidural spinal cavernous hemangiomas (SCH) account for only 4% of all spinal epidural lesions. Our literature review identified 61 publications reporting on, a total of 175 cases in the magnetic resonance imaging era. Here, we reviewed those cases, and have added our case of what appeared to be a multifocal SCH.
Case Description: A 72-year-old male presented with a progressive paraparesis attributed to a T5/T6 dorsolateral extradural mass extending into the right T5/6 foramen. Surgical excision documented the lesion, histologically, was a SCH. A second similar lesion was noted involving the left C7/T1 foramen; as the patient was asymptomatic from this lesion, and no additional biopsy was performed. The patient returned to normal neurological function within 2 months postoperatively.
Conclusions: Here, a 72-year-old male presented with a pathologically confirmed T5/T6 epidural SCH and a secondary C7/T1 foraminal lesion suspected to represent a secondary focus of an epidural SCH.
Keywords: Cavernous hemangioma, Epidural, Myelopathy, Spinal, Surgical excision
INTRODUCTION
Pure epidural spinal cavernous hemangiomas (SCH) account for only 4% of all spinal epidural lesions. Notably, 61 studies identified 175 cases in the magnetic resonance imaging (MRI) era. Here, we reviewed those cases, and now add 72-year-old male with a pathologically confirmed T5/T6 epidural SCH lesion.
CASE DESCRIPTION
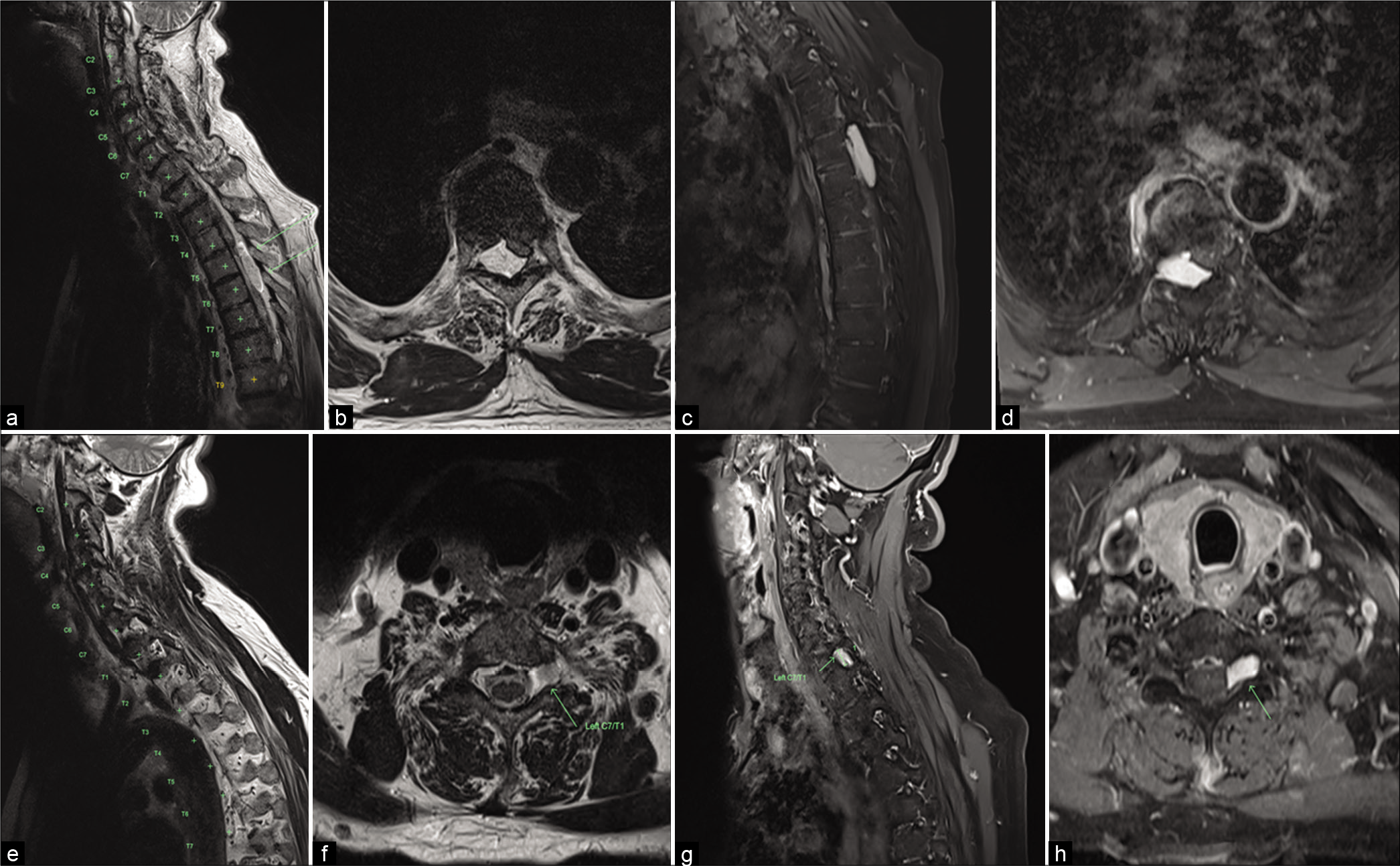
A 72-year-old male presented with slowly progressive incoordination and mild lower extremity weakness. The computed tomography (CT) scan documented an extradural T5/T6 lesion with the right T5/6 foraminal bony remodeling/extension. The MR further demonstrated that the lesion was well-circumscribed, and occupied the right T5/T6 dorsolateral spinal canal; it was hypointense on T1/hyperintense on T2-weighted images, and homogeneously enhanced with contrast [
Figure 1:
(a) T2 sagittal magnetic resonance imaging (MRI) demonstrating T2 hyperintense extradural mass at T5/6; (b) T2 axial MRI demonstrating right-sided dorsolateral mass with cord compression; (c and d) T1 + Gad sagittal and axial MRI demonstrating homogenous enhancement; (e and f) T2 sagittal and axial MRI demonstrating T2 hyperintense mass at the left C7/T1 foramen; (g and h) T1 + Gad sagittal and axial MRI demonstrating homogenous enhancement.
Surgery
Following a T5-6 laminectomy, a soft, purple, well-circumscribed mass was easily dissected away from the underlying dura, allowing for complete resection in a piecemeal manner.
Pathology
The histopathology of the T5/T6 lesion proved to be an epidural SCH.
Postoperative course
Postoperatively, the patient experienced a full neurological recovery.
DISCUSSION
Pure epidural SCH are rare, accounting for only 4% of spinal epidural lesions,[
Clinical findings
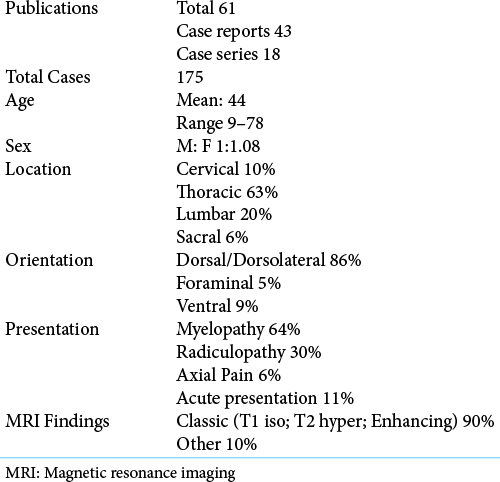
The 175 patients in 61 studies all had single SCH lesions. Patients typically presented with myelopathy (64%), followed by radiculopathy (30%), and axial pain (6%) [
SCH lesion locations
SCH lesions predominantly involved the thoracic spine (64%), followed by the lumbar (20%), cervical (10%), and sacral spinal levels (6%). Most lesions were dorsal/dorsolateral in location. Some lateral lesions produce foraminal remodeling. When present, dumbbell morphology frequently led to the misdiagnosis of these lesions as schwannomas.[
Imaging findings
On MR imaging, epidural SCH were classically iso-intense on T1, hyper-intense on T2, and homogeneously enhanced with contrast. Intralesional T2 hyper-intensity is thought to represent stagnant blood contained within large vascular channels.[
Operative findings
Although recurrent lesions may be adherent to the dura, most epidural SCH were well-defined, encapsulated, and readily separated from the dura.[
Prognosis
Surgical outcomes for SCH are generally favorable. However, those who present with the rapid onset of new neurological deficits secondary to acute intra-tumoral hemorrhages have poorer prognoses.[
CONCLUSION
Pure epidural SCH are rare and may mimic other more common benign tumors such as schwannomas. The natural history is one of slow symptom progression with favorable outcomes. However, the prognoses are guarded for the 10% who present with acute intra-tumoral hemorrhages and develop the rapid onset of paralysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Haimes AB, Krol G. Dumbbell-shaped spinal cavernous hemangioma: A case report. Am J Neuroradiol. 1991. 12: 1021-2
2. Killeen T, Czaplinski A, Cesnulis E. Extradural spinal cavernous malformation: A rare but important mimic. Br J Neurosurg. 2014. 28: 340-6
3. Li TY, Xu YL, Yang J, Wang J, Wang GH. Primary spinal epidural cavernous hemangioma: Clinical features and surgical outcome in 14 cases. J Neurosurg Spine. 2015. 22: 39-46
4. Tekkok IH, Akpinar G, Gungen Y. Extradural lumbosacral cavernous hemangioma. Eur Spine J. 2004. 13: 469-73
5. Zhang L, Qiao G, Shang A, Yu X. Clinical features and long-term surgical outcomes of pure spinal epidural cavernous hemangioma-report of 23 cases. Acta Neurochir (Wien). 2020. 162: 2915-21
6. Zhang L, Zhang Z, Yang W, Shang J, Jia W, Yang J. Spinal dumbbell-shaped epidural cavernous hemangioma (CM): Report of nine surgical cases and literature review. Chin Neurosurg J. 2018. 4: 3
7. Zhong W, Huang S, Chen H, Sun H, Cai B, Liu Y. Pure spinal epidural cavernous hemangioma. Acta Neurochir (Wien). 2012. 154: 739-45