- Department of Neurosurgery, Nagoya City University West Medical Center, Nagoya, Aichi, Japan.
- Department of Neurosurgery, Nagoya City University Graduate School of Medical Sciences and Medical School, Nagoya, Aichi, Japan.
- Department of Neurosurgery, Chutoen General Medical Center, Shizuoka, Japan.
Correspondence Address:
Teishiki Shibata, Department of Neurosurgery, Nagoya City University West Medical Center, Nagoya, Aichi, Japan.
DOI:10.25259/SNI_1035_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Teishiki Shibata1, Yusuke Nishikawa2, Takumi Kitamura3, Mitsuhito Mase2. Cavernous sinus dural arteriovenous fistula accessed through a straightened superficial temporal vein. 30-Dec-2021;12:634
How to cite this URL: Teishiki Shibata1, Yusuke Nishikawa2, Takumi Kitamura3, Mitsuhito Mase2. Cavernous sinus dural arteriovenous fistula accessed through a straightened superficial temporal vein. 30-Dec-2021;12:634. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11317
Abstract
Background: Transvenous embolization through the inferior petrosal sinus (IPS) is the most common treatment procedure for cavernous sinus dural arteriovenous fistula (CSDAVF). When the IPS is inaccessible or the CSDAVF cannot be treated with transvenous embolization through the IPS, the superficial temporal vein (STV) is used as an alternative access route. However, the approach through the STV is often challenging because of its tortuous and abruptly angulated course. We report a case of recurrent CSDAVF which was successfully treated using a chronic total occlusion (CTO)-dedicated guidewire and by straightening the STV.
Case Description: A 63-year-old woman was diagnosed with CSDAVF on examination for oculomotor and abducens nerve palsy. She was initially treated with transvenous embolization through the IPS. However, CSDAVF recurred, and transvenous embolization was performed through the STV. A microcatheter could not be navigated because of the highly meandering access route through the STV. By inserting a CTO-dedicated guidewire into the microcatheter, the STV was straightened and the microcatheter could be navigated into a shunted pouch of the CS. Finally, complete occlusion of the CSDAVF was achieved.
Conclusion: If an access route is highly meandering, the approach can be facilitated by straightening the access route with a CTO-dedicated guidewire.
Keywords: Cavernous sinus, Dural arteriovenous fistula, Embolization, Transvenous
INTRODUCTION
For the curative treatment of cavernous sinus dural arteriovenous fistulas (CSDAVF), transvenous embolization (TVE) is the first choice, and the inferior petrosal sinus (IPS) is most often selected as an access route to the CS.[
CASE PRESENTATION
A 63-year-old woman presented with ptosis of the right eye at the ophthalmology department of our hospital. She was suspected to have a CSDAVF on brain magnetic resonance imaging and was referred to our department. On neurological examination, she displayed palsy of the oculomotor and abducens nerves. She had no history of trauma or surgery. Cerebral angiography showed a CSDAVF fed from the left accessory meningeal artery, left artery of foramen rotundum, right meningohypophyseal trunk, and right ascending pharyngeal artery. These feeding arteries converged at the posteromedial compartment of the right CS, formed a shunted pouch, and drained into the right IPS [
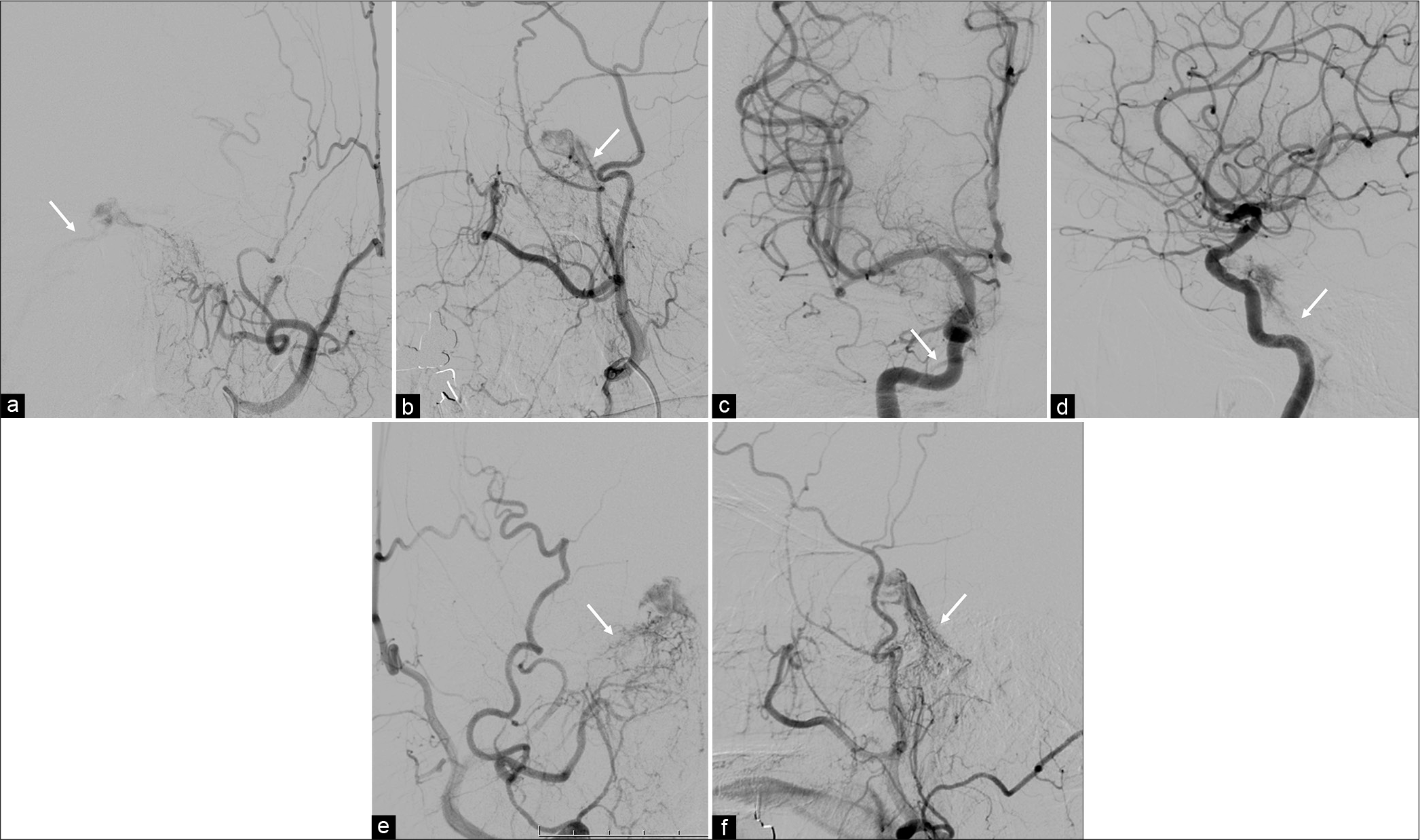
Figure 1:
The left external carotid artery angiogram (a: Anteroposterior view, b: Lateral view), the right internal carotid artery angiogram (c: Anteroposterior view, d: Lateral view), and the right external carotid artery angiogram (e: Anteroposterior view, f: Lateral view) show a cavernous sinus dural arteriovenous fistula that is mainly fed by the left accessory meningeal artery, left artery of foramen rotundum (a and b), right meningohypophyseal trunk (c and d), and right ascending pharyngeal artery (e and f). The cavernous sinus dural arteriovenous fistula has a shunted pouch on the posteromedial compartment of the right cavernous sinus and drains into the right inferior petrosal sinus (arrows in a-f).
After 6 weeks from the operation, the patient developed exophthalmos and conjunctival congestion of the right eye and palsy of the oculomotor and abducens nerves worsened. Cerebral angiography showed recurrence of the CSDAVF. The feeder was the right meningohypophyseal trunk, and the shunted pouch was identified as the anterolateral compartment of the right CS. The right superior ophthalmic vein (SOV), the main drainer, drained into the STV [
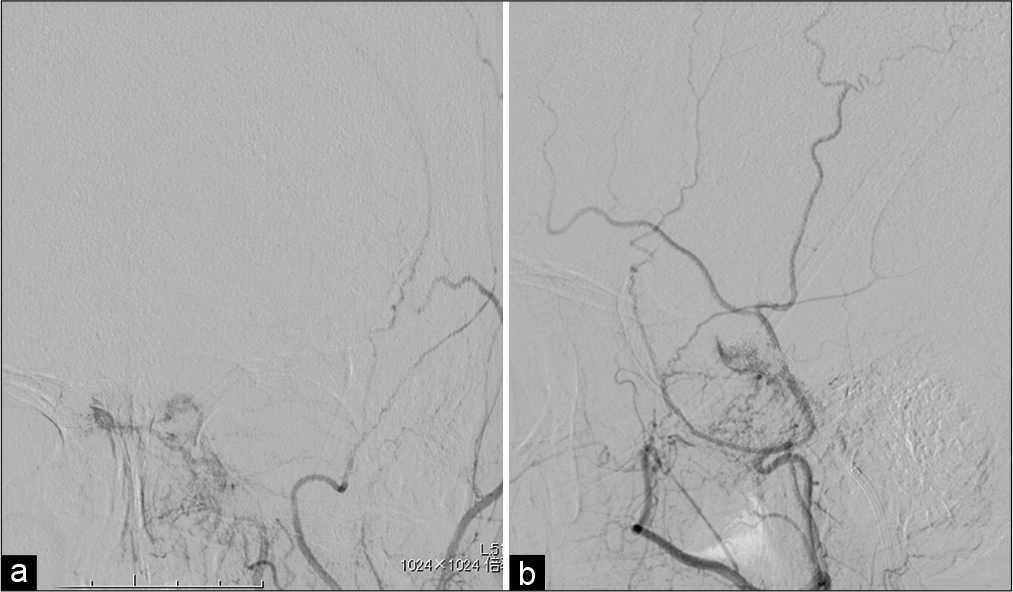
Figure 3:
The right internal carotid angiogram (a: Anteroposterior view, b: Lateral view) shows a cavernous sinus dural arteriovenous fistula that is fed by the right meningohypophyseal trunk and drains into the right superior ophthalmic vein (dotted arrows). The venous phase of the right internal carotid angiogram (c: Anteroposterior view, d: Lateral view) shows the cavernous sinus dural arteriovenous fistula draining from the superior ophthalmic vein to the superficial temporal vein (arrowheads), with ipsilateral inferior petrosal sinus occlusion. Axial (e) and sagittal (f) reformatted images of the rotational angiography show a shunted pouch located at the anterolateral compartment of the right cavernous sinus (arrows).
Endovascular retreatment with transvenous embolization
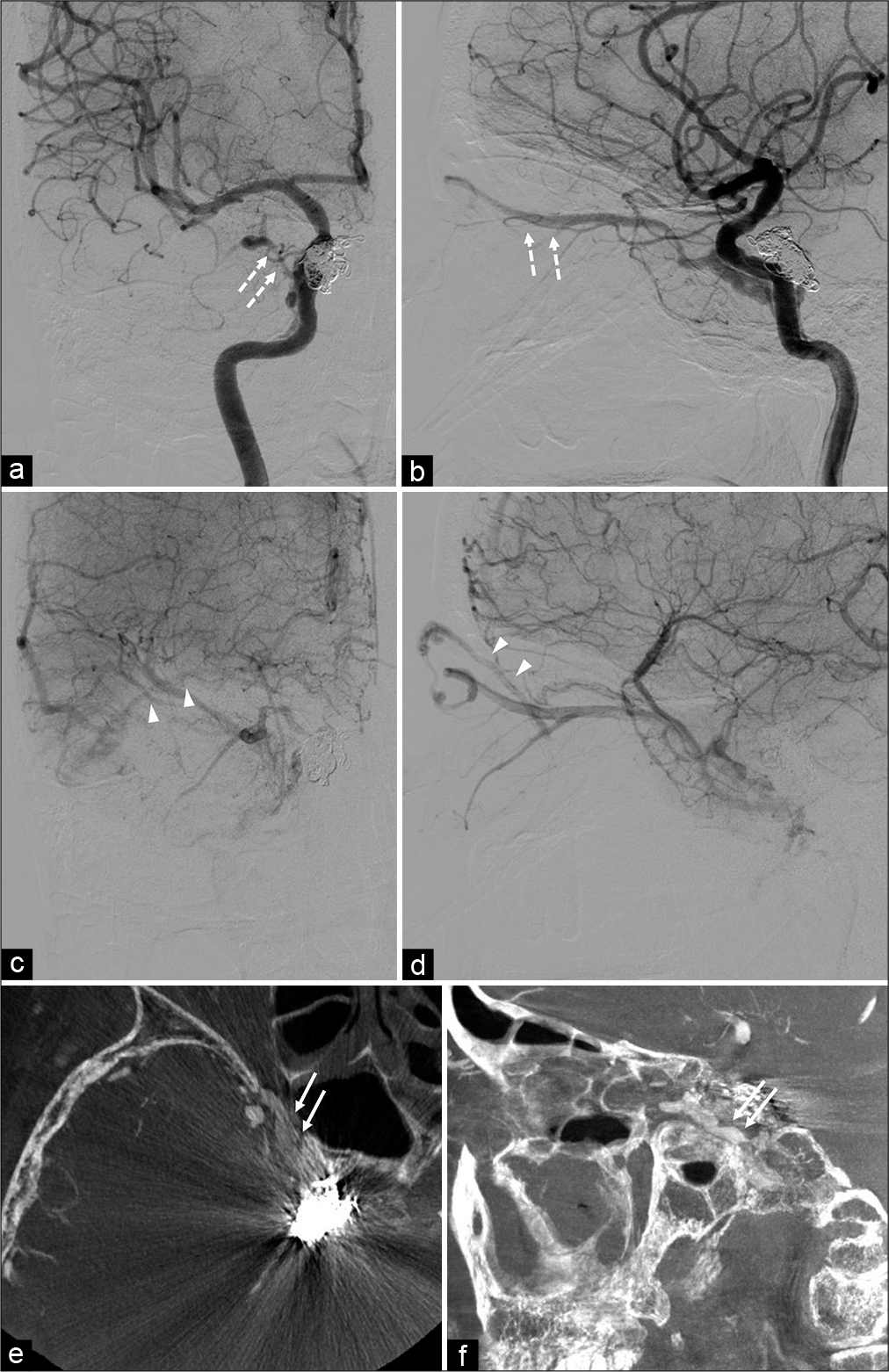
The patient was sedated with dexmedetomidine and was given pentazocine during endovascular treatment. The transfemoral venous approach with systemic heparinization was performed. For intraprocedural angiography, a 4-F catheter was positioned at the right internal carotid artery. A 5-F Slim Guide guiding catheter 93 cm (Medikit Co., Tokyo, Japan) was positioned at the right external jugular vein. Through the 5-F guiding catheter, a 3.4-F TACTICS 130 cm (Technocrat Corporation, Aichi, Japan), which was used as a distal access catheter, and a CHIKAI black 18 (Asahi Intecc Co., Aichi, Japan), which was a 0.018" guidewire, were navigated into the right STV from the right retromandibular vein. Subsequently, from the TACTICS, a 1.9-F Carnelian MARVEL nontaper microcatheter 160 cm (Tokai Medical Products Inc., Aichi, Japan) and a Transend 10 microwire (Stryker, Kalamazoo, MI, USA) were used to attempt to advance to the right CS by guiding these through the right STV and the right SOV. The route from the STV to the SOV was tortuous and abruptly angulated. The 5-F guiding catheter was guided to the distal retromandibular vein and the TACTICS was guided as far as possible to distal STV to increase the support of the microcatheter, and the navigation of MARVEL to the right CS was attempted. However, the STV and the SOV were looping, and the right CS was inaccessible. Although various microcatheters and microwires were used and manually stretching the looped STV was attempted, the microcatheter could not be navigated into the right CS. Finally, a 0.014" ATHLETERUBY PT SUPPORT (Japan Lifeline Co., Tokyo, Japan), a CTO-dedicated guidewire, was inserted into the microcatheter, being careful not to allow the tip of the guidewire come out of the microcatheter, and the STV was linearized [
Video 1
Figure 4:
The abruptly angulated and tortuous course from the superficial temporal vein (STV) to the superior ophthalmic vein (SOV) is shown in the Anteroposterior (a) and Lateral (b) views of the right internal carotid artery angiogram and in the Anteroposterior (c) and Lateral (d) views of snapshot images. A microcatheter (white arrows in a-d) cannot be navigated from the STV to the SOV, with a distal access catheter (white dotted arrows in a-d) guided into the STV. The right internal carotid artery angiogram (e: Anteroposterior view, f: Lateral view) shows the straightened STV route (white arrowheads in e and f) by inserting an ATHLETERUBY PT guidewire into the microcatheter. The distal access catheter can be guided from the STV to the angular vein (white dotted arrows in e-h) and a 5-F guiding catheter can guided from the distal retromandibular vein to the STV (black arrows in e-h). The microcatheter (white arrows in e-h) can be navigated into a shunted pouch of the right cavernous sinus and the microcatheter injection (g: Anteroposterior view, h: Lateral view) reveals the shunted pouch of the right cavernous sinus draining into the SOV. Transvenous coil embolization is performed and complete occlusion of cavernous sinus dural arteriovenous fistula is achieved on postprocedural angiography (i: Anteroposterior view, j: Lateral view).
Postoperative course
After the second operation, exophthalmos and conjunctival congestion and the palsy of oculomotor and abducens nerves disappeared. There was no recurrence during the 3 years of observation.
DISCUSSION
TVE is the first-line curative treatment for CSDAVF, and the success rate of complete occlusion of the fistula by TVE is reported to be 81–82%.[
In this case, direct puncture of the STV or the SOV may have been considered an alternative treatment route, but direct puncture of the STV may cause occlusion due to STV injury. If the STV is occluded and a new drainage route from the SOV to the FV does not appear, congestion of the ophthalmic veins can cause increased intraocular pressure, which results in visual impairment. Furthermore, in such a case, only direct puncture of the SOV can be used as an approach route. For direct puncture of the SOV, various complications, such as puncture-related intraorbital hemorrhage, injury of the levator muscle and supraorbital nerve, orbital infection, granulomas, damage to the trochlear nerve, and nonarteritic ischemic optic neuropathy, have been reported.[
The approach from the STV or FV to the SOV is often difficult to achieve due to significant meandering and steep flexion of the route. To solve this problem, there are methods to manually unbend the veins or to guide using a triple coaxial system.[
The ATHLETERUBY PT guidewire is a CTO-dedicated guidewire used for CTO of peripheral blood vessels.[
CONCLUSION
We treated a patient with CSDAVF through ipsilateral IPS, however, it recurred and was retreated through the STV. Although the access route from the STV to the SOV was tortuous and abruptly angulated, access to the CS was achieved by straightening the STV with a CTO-dedicated guidewire. Finally, the CSDAVF was diminished. If the access route is highly meandering, straightening the route with a CTO-dedicated guidewire can facilitate the approach.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
References
1. Alexandre AM, Visconti E, Lozupone E, D’Argento F, Pedicelli A. Embolization of dural arteriovenous fistula of the cavernous sinus through percutaneous ultrasound-guided puncture of the facial vein. World Neurosurg. 2017. 99: 812.e13-20
2. Briganti F, Caranci F, Leone G, Napoli M, Cicala D, Briganti G. Endovascular occlusion of dural cavernous fistulas through a superior ophthalmic vein approach. Neuroradiol J. 2013. 26: 565-72
3. Cheng KM, Chan CM, Cheung YL. Transvenous embolisation of dural carotid-cavernous fistulas by multiple venous routes: A series of 27 cases. Acta Neurochir (Wien). 2003. 145: 17-29
4. Chihara H, Hatano T, Sadamasa N, Kai Y, Saka M, Ando M. A case of cavernous sinus dural arteriovenous fistula treated by transfacial vein placement of a distal access catheter in the cavernous sinus. JNET J Neuroendovasc Ther. 2017. 11: 431-6
5. Choi JH, Shin YS, Kim BS. Making microguidewire loop facilitates navigation through tortuous or abruptly angulated head and neck veins to access cavernous sinus dural arteriovenous fistulas. World Neurosurg. 2019. 129: e561-5
6. Heran MK, Volders D, Haw C, Shewchuk JR. Imaging-guided superior ophthalmic vein access for embolization of dural carotid cavernous fistulas: Report of 20 cases and review of the literature. AJNR Am J Neuroradiol. 2019. 40: 699-702
7. Ikeda N, Abiko M, Sakakura T, Nakano S, Nishizaki T. Endovascular treatment of chronic total occlusion of the internal carotid artery. Surg Cereb Stroke (Jpn). 2014. 42: 109-15
8. Ishii M, Hayashi M, Sato K, Iwama J, Hirai N, Hiramoto Y. Use of a superficial temporal vein approach for transvenous embolization of a cavernous sinus dural arteriovenous fistula: A case report. JNET J Neuroendovasc Ther. 2015. 9: 90-5
9. Jahan R, Gobin YP, Glenn B, Duckwiler GR, Viñuela F. Transvenous embolization of a dural arteriovenousfistula of the cavernous sinus through the contralateral pterygoid plexus. Neuroradiology. 1998. 40: 189-93
10. Kawarada O, Sakamoto S, Harada K, Ishihara M, Yasuda S, Ogawa H. Contemporary crossing techniques for infrapopliteal chronic total occlusions. J Endovasc Ther. 2014. 21: 266-80
11. Kazekawa K, Iko M, Sakamoto S, Aikawa H, Tsutsumi M, Kodama T. Dural AVFs of the cavernous sinus: Transvenous embolization using a direct superficial temporal vein approach. Radiat Med. 2003. 21: 138-41
12. Kirsch M, Henkes H, Liebig T, Weber W, Esser J, Golik S. Endovascular management of dural carotid-cavernous sinus fistulas in 141 patients. Neuroradiology. 2006. 48: 486-90
13. Klisch J, Huppertz HJ, Spetzger U, Hetzel A, Seeger W, Schumacher M. Transvenous treatment of carotid cavernous and dural arteriovenous fistulae: Results for 31 patients and review of the literature. Neurosurgery. 2003. 53: 836-56
14. Kuwayama N, Endo S, Kitabayashi M, Nishijima M, Takaku A. Surgical transvenous embolization of a cortically draining carotid cavernous fistula via a vein of the sylvian fissure. AJNR Am J Neuroradiol. 1998. 19: 1329-32
15. Matsumoto A, Okauchi M, Shindo A, Kawanishi M, Tamiya T. Cavernous sinus dural arteriovenous fistula treated by facial vein direct puncture: Case report and review of the literature. Interv Neuroradiol. 2017. 23: 301-6
16. Mounayer C, Piotin M, Spelle L, Moret J. Superior petrosal sinus catheterization for transvenous embolization of a dural carotid cavernous sinus fistula. AJNR Am J Neuroradiol. 2002. 23: 1153-5
17. Quiñones D, Duckwiler G, Gobin PY, Goldberg RA, Viñuela F. Embolization of dural cavernous fistulas via superior ophthalmic vein approach. AJNR Am J Neuroradiol. 1997. 18: 921-8
18. Shinoda N, Mori M, Tamura S, Korosue K, Kose S, Imai H. A patient with a cavernous sinus dural arteriovenous fistula in whom direct puncture of the superior ophthalmic vein led to rapidly progressing thrombosis and postoperative non-arteritic ischemic optic neuropathy: Pathogenesis with respect to a drainage route. JNET J Neuroendovasc Ther. 2019. 13: 221-7
19. Venturi C, Bracco S, Cerase A, Gennari P, Lorè F, Polito E. Endovascular treatment of a cavernous sinus dural arteriovenous fistula by transvenous embolisation through the superior ophthalmic vein via cannulation of a frontal vein. Neuroradiology. 2003. 45: 574-8
20. Yoshida K, Melake M, Oishi H, Yamamoto M, Arai H. Transvenous embolization of dural carotid cavernous fistulas: A series of 44 consecutive patients. AJNR Am J Neuroradiol. 2010. 31: 651-5
21. Yuen MH, Cheng KM, Cheung YL, Chan CM, Yu SC, Wong GK. Triple coaxial catheter technique for transfacial superior ophthalmic vein approach for embolization of dural carotid-cavernous fistula. Interv Neuroradiol. 2010. 16: 264-8