- Department of Neurological Surgery, University of Pittsburgh School of Medicine, UPMC Presbyterian, Pittsburgh, Pennsylvania, United States.
- Department of Neurological Surgery, University of Pittsburgh Medical Center, UPMC Presbyterian, Pittsburgh, Pennsylvania, United States.
- Department of Neurological Surgery, Albert Einstein College of Medicine, Bronx, New York, United States.
- Department of Neurological Surgery, Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania, United States.
Correspondence Address:
Nduka M. Amankulor, MD, Department of Neurological Surgery, Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania, United States.
DOI:10.25259/SNI_1110_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Emade Jaman1, Xiaoran Zhang2, Jordan Allen3, Raj G. Saraiya1, Savannah Tollefson1, D. Kojo Hamilton2, Nduka M. Amankulor4. Percutaneous fixation for the treatment of metastatic spinal disease provides effective symptom palliation with low rates of hardware failure. 11-Feb-2022;13:50
How to cite this URL: Emade Jaman1, Xiaoran Zhang2, Jordan Allen3, Raj G. Saraiya1, Savannah Tollefson1, D. Kojo Hamilton2, Nduka M. Amankulor4. Percutaneous fixation for the treatment of metastatic spinal disease provides effective symptom palliation with low rates of hardware failure. 11-Feb-2022;13:50. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11381
Abstract
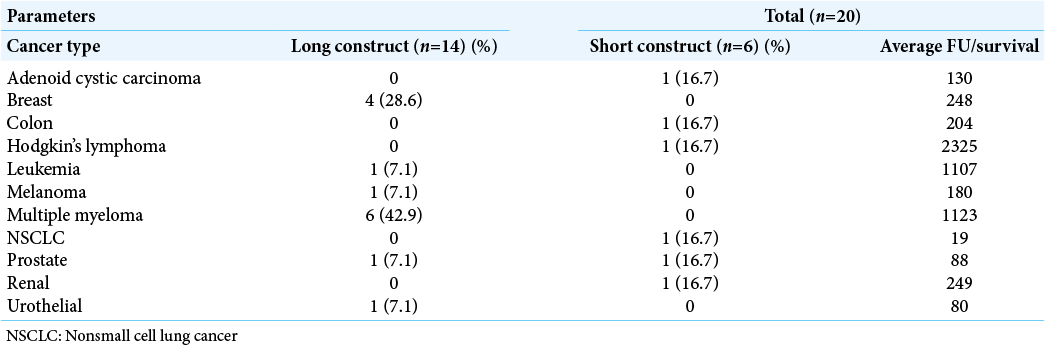
Background: The incidence of survival from metastatic spinal disease (MSD) continues to rise. However, open surgery for MSD is associated with significant perioperative morbidity, while minimally invasive percutaneous pedicle screw fixation (MIPPSF) offers reduced tissue trauma, less blood loss, and a reduction in complications. Lytic bone disease plus perioperative radiation further increase risk for instrument failure, especially in long construct MIPPSF. Here, we compared 6 short construct and 14 long construct outcomes for MIPPSF performed in MSD patients, including multiple myeloma (MM).
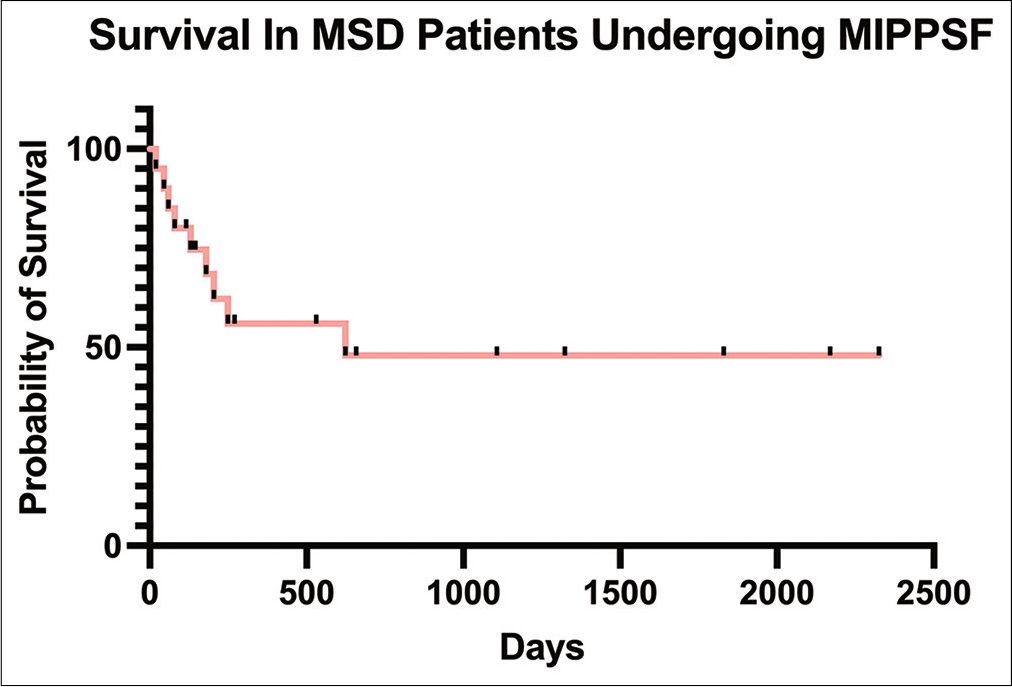
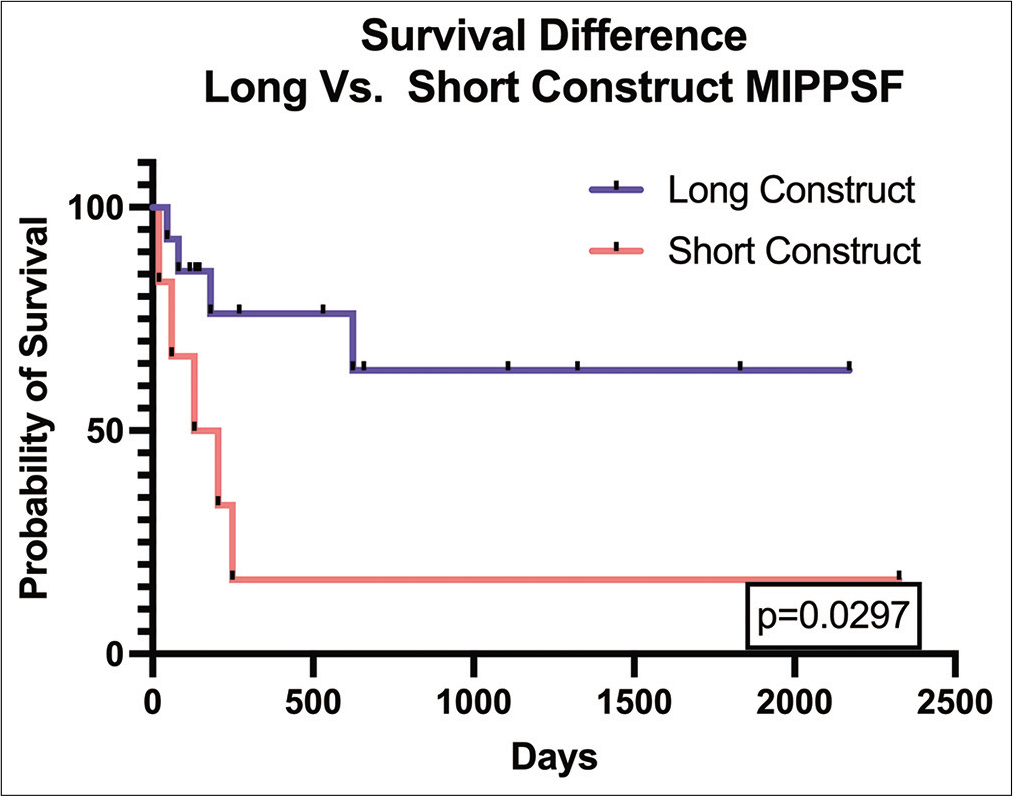
Methods: For 20 patients undergoing MIPPSF for MSD, we evaluated disease type, location, the extent of surgery, outcomes, and survival rates. Statistical comparisons were performed between long-segment construct and short-segment construct patients utilizing Kaplan–Meier survival curves, Mann–Whitney U, and Chi-squared tests.
Results: No instrument failure and comparable symptomatic relief were observed for both short and long MIPPSF constructs. However, long construct patients experienced; a higher incidence of postoperative complications, including screw loosening, but exhibited longer overall survivals (likely related to underlying type of MSD, with MM patients making up the largest portion of long construct patients).
Conclusion: Long construct MIPPSF in MSD did not have increased risk of construct failure and offered effective symptomatic relief, including for MM patients, without introducing a greater risk construct instability.
Keywords: Long construct, Metastatic spinal disease, Minimally invasive, Multiple myeloma, Percutaneous pedicle screw fixation, Spine
INTRODUCTION
Metastatic spinal disease (MSD) is the most common type (60%) of bone metastases in cancer patients.[
MATERIALS AND METHODS
Clinical, surgical data, and outcomes for 20 patients with MSD
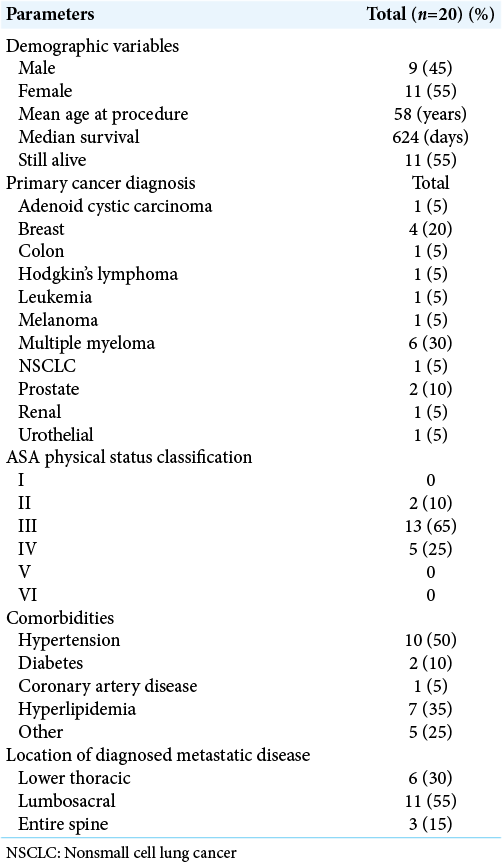
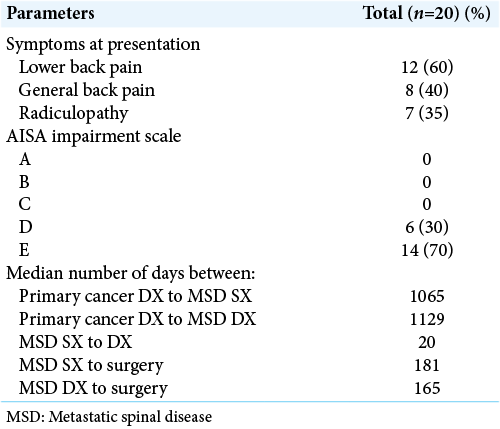
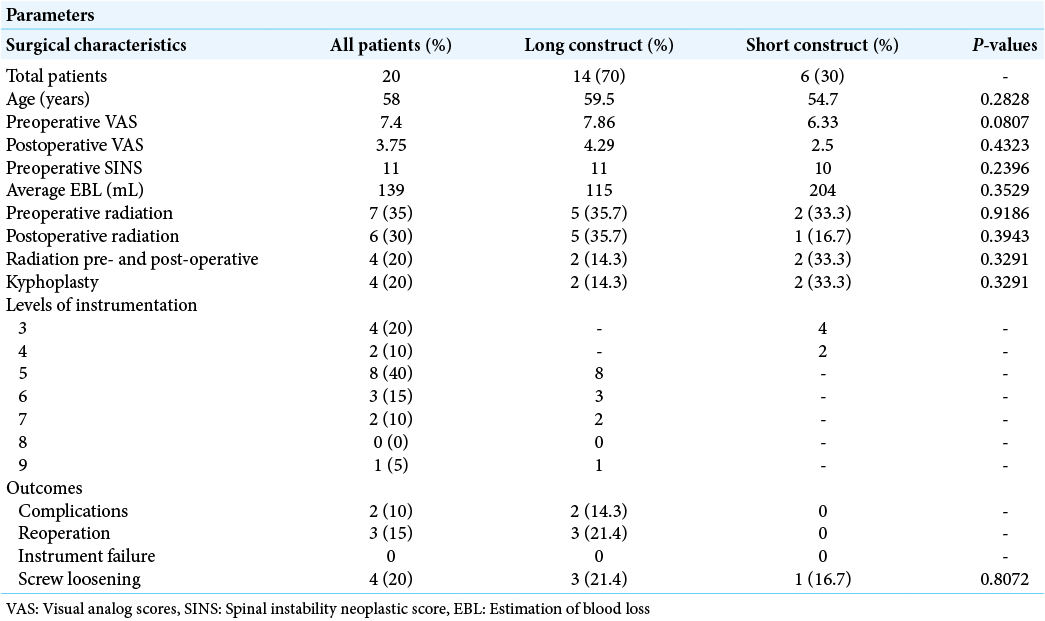
We evaluated the demographic variables for 20 patients with MSD including; age, sex, comorbidities, primary cancer type, dates of diagnosis, and length of follow-up or time to death. Surgical data included; fused levels, location of metastases, estimated blood loss, adjuvant radiation treatment, and perioperative complications. The primary outcome measures included; implant failure (i.e., screw pull out, breakage, and angular deformity) and the reoperation/instrumentation revision rate. Secondary outcomes measures included follow-up duration and time to death. In addition, we defined long constructs as percutaneous screw fixation involving five or more levels.
Metrics of analysis
The ASA Physical Status Classification (scaled I–VI), body mass index, visual analog scores (VAS) (scale 1–10) were used to classify patients’ operative general health status and quantify pain both preoperatively and 2 weeks postoperatively. The spinal instability neoplastic score was used to determine the metastatic-related instability of the vertebral column. Finally, the American Spinal Cord Injury Association Impairment Scale (Graded A-E) was used for preoperative classification of impairment.
Operative technique
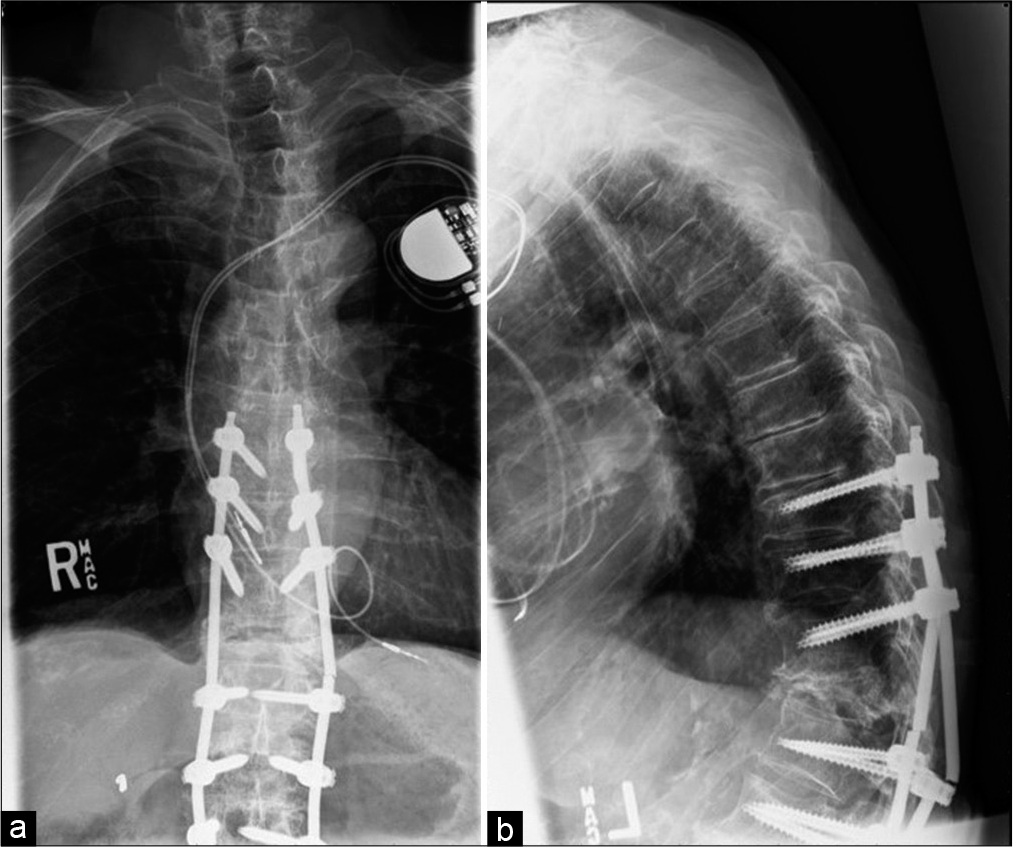
Pedicle screws were percutaneously placed 5 mm lateral to the lateral border of the thoracic pedicles and 3 mm laterally for L2-L5 lumbar screw placement.
Statistical analysis
Continuous variables were summarized with either means or medians. Standard deviation and range were included when appropriate. Continuous variables lacked normal distribution in our case series and intergroup comparisons were analyzed using the Mann–Whitney U-test. Discrete variables were analyzed by a Chi-squared test. Statistical significance was set to P ≤ 0.05. All statistical analyses were performed using GraphPad Prism version 9.0 for Windows, GraphPad Software, San Diego, California, USA.
Study demographics
All 20 patients presented with generalized back pain, among which seven also had radiculopathy. Sixteen patients (80%) had a previously known diagnosis of primary malignancy. All 20 patients with a history of MSD underwent MIPPSF for spinal metastases. Patient average age was 58 years [
RESULTS
Surgical outcomes
Fourteen patients (70%) underwent long construct MIPPSF, with 6 (30%) undergoing short construct MIPPSF. Both groups exhibited comparable symptomatic relief/improvement (VAS reduction of 45.42% in long constructs vs. 60.32% in short constructs, P = 0.43). Those in the long construct group showed no greater blood loss from surgery, but three had postoperative complications requiring reoperations (i.e., superficial infection/ dehiscence, radiculopathy due to medial placement of an S1 screw/revised, and reoperation 2 months later for epidural spinal cord compression with increased neurological deficits). Notably, no complications were observed in the short construct cohort, while 3 (21.4%) of the long construct patients exhibited instances of screw loosening versus 1 patient (16.7%) in the short construct group (P = 0.81) [
DISCUSSION
Advancements in oncological treatment for MSD have led to increased survival rates and patients with MSD requiring surgical decompression/fusion of the spine. Minimally invasive spinal surgery for MSD now includes percutaneous pedicle screw fixation (MIPPSF). Here, we compared multiple clinical, radiographic, and outcome variables for patients with MSD undergoing short and long construct MIPPSF.
Varying instrumentation failure rates using MIPPSF for MSD
Studies in the spine oncology literature demonstrate varying MIPPSF instrument failure particularly for longer constructs. Versteeg et al. conducted a retrospective study of 101 patients from which they observed n = 4 patients experiencing construct failure (4%), with n = 6 patients (5.9%) requiring revision surgery, bringing their instrument failure rate between 6% and 10%.[
Differences in survival
We observed a higher median survival in the patients undergoing long construct PSFS versus short constructs. This was likely attributed to the types of the primary underlying cancers. The literature shows that survival for MSD patients primarily depends on the tumor type with 2-year survival rates ranging from 9% in lung cancer to 44% in breast and prostate cancer, with only 10–20% of MSD patients still alive 2 years following diagnosis the time of their original diagnosis.[
CONCLUSION
In our retrospective cohort of 20 patients who underwent MIPPSF for MSD, we found that long-segment constructs were safe and did not increase the risk of instrumentation failure requiring reoperation. Notably, the inability to perform MIPPSF fusions did not correlate with poorer outcomes.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aly TA. Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: Meta-analysis. Asian Spine J. 2017. 11: 150-60
2. Amankulor NM, Xu R, Iorgulescu JB, Chapman T, Reiner AS, Riedel E. The incidence and patterns of hardware failure after separation surgery in patients with spinal metastatic tumors. Spine J. 2014. 14: 1850-9
3. Barzilai O, Robin AM, O’Toole JE, Laufer I. Minimally invasive surgery strategies: Changing the treatment of spine tumors. Neurosurg Clin N Am. 2020. 31: 201-9
4. Delank KS, Wendtner C, Eich HT, Eysel P. The treatment of spinal metastases. Dtsch Arztebl Int. 2011. 108: 71-80
5. Kumar N, Zaw AS, Reyes MR, Malhotra R, Wu PH, Makandura MC. Versatility of percutaneous pedicular screw fixation in metastatic spine tumor surgery: A prospective analysis. Ann Surg Oncol. 2015. 22: 1604-11
6. Mesfin A, Sciubba DM, Dea N, Nater A, Bird JE, Quraishi NA. Changing the adverse event profile in metastatic spine surgery: An evidence-based approach to target wound complications and instrumentation failure. Spine (Phila Pa 1976). 2016. 41: S262-70
7. Moussazadeh N, Rubin DG, McLaughlin L, Lis E, Bilsky MH, Laufer I. Short-segment percutaneous pedicle screw fixation with cement augmentation for tumor-induced spinal instability. Spine J. 2015. 15: 1609-17
8. Spratt DE, Beeler WH, de Moraes FY, Rhines LD, Gemmete JJ, Chaudhary N. An integrated multidisciplinary algorithm for the management of spinal metastases: An international spine oncology consortium report. Lancet Oncol. 2017. 18: e720-30
9. Ulmar B, Huch K, Kocak T, Catalkaya S, Naumann U, Gerstner S. The prognostic influence of primary tumour and region of the affected spinal segment in 217 surgical patients with spinal metastases of different entities. Z Orthop Ihre Grenzgeb. 2007. 145: 31-8
10. Versteeg AL, Verlaan JJ, de Baat P, Jiya TU, Stadhouder A, Diekerhof CH. Complications after percutaneous pedicle screw fixation for the treatment of unstable spinal metastases. Ann Surg Oncol. 2016. 23: 2343-9