- Department of Neurosurgery, The Jikei University School of Medicine, Minato-Ku, Tokyo, Japan.
- Department of Neurosurgery, Higashi-Yokohama Neurosurgery Hospital, Yokohama, Kanagawa, Japan.
Correspondence Address:
Toshihiro Ishibashi, Department of Neurosurgery, The Jikei University School of Medicine, Minato-Ku, Tokyo, Japan.
DOI:10.25259/SNI_1165_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toshihiro Ishibashi1, Shogo Kaku2, Shota Sonoda2, Yuichi Murayama1. Remote neuro-endovascular consultation using a secure telemedicine system: A feasibility study. 11-Feb-2022;13:47
How to cite this URL: Toshihiro Ishibashi1, Shogo Kaku2, Shota Sonoda2, Yuichi Murayama1. Remote neuro-endovascular consultation using a secure telemedicine system: A feasibility study. 11-Feb-2022;13:47. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11390
Abstract
Background: Telemedicine has been rapidly implemented under COVID-19 conditions, to assess the ability to use an audio-visual telemedicine system for neuro-endovascular remote consultation.
Methods: The system consists of a live streaming function for angiography and an operating room (OR) camera using a smartphone application (JOIN; Allm Inc, Tokyo, Japan) in conjunction with verbal communication using the Zoom app. The system allows us to display multiple angiographic images in addition to streaming video from the 4K camera recording the operator’s procedure and from the 4K camera showing the OR view on the monitor of any smart device.
Results: The operator was able to speak with the senior supervisor through a bone conduction headphone and to talk to assistants or radiology technicians without any hearing difficulties. The remote supervisor was able to check the streaming images, which had almost the same imaging quality as real digital subtraction angiogram (DSA) monitors, and he could advise the handling of devices and preparation through the 4K video camera systems. The DSA image delay was within 2 s.
Conclusion: A remote consultation system with real-time audio-visual capability may play an important role in acute stroke management and maintain the quality of patient care under COVID-19 conditions.
Keywords: Education, Endovascular, Remote, Stroke, Telemedicine
INTRODUCTION
Telemedicine has been quickly applied under COVID-19 conditions. Several studies have shown that telemedicine is effective in the management of stroke care.[
We recently established a telemedicine system that allows further remote support, including real-time imaging and verbal communication, for neuro-endovascular therapy. We report our initial clinical experience in acute stroke treatment and scheduled unruptured aneurysm embolization using a remote neuroendovascular support system.
MATERIALS AND METHODS
This system was developed at the university and was used for case consultation at an affiliated hospital. The study protocol was reviewed and approved by the ethics committee and the research review board at the affiliated hospital. All patients were provided informed consent, and each site had obtained Institutional Review Board approval and signed consent forms. The participants and any identifiable individuals consented to the publication of their image.
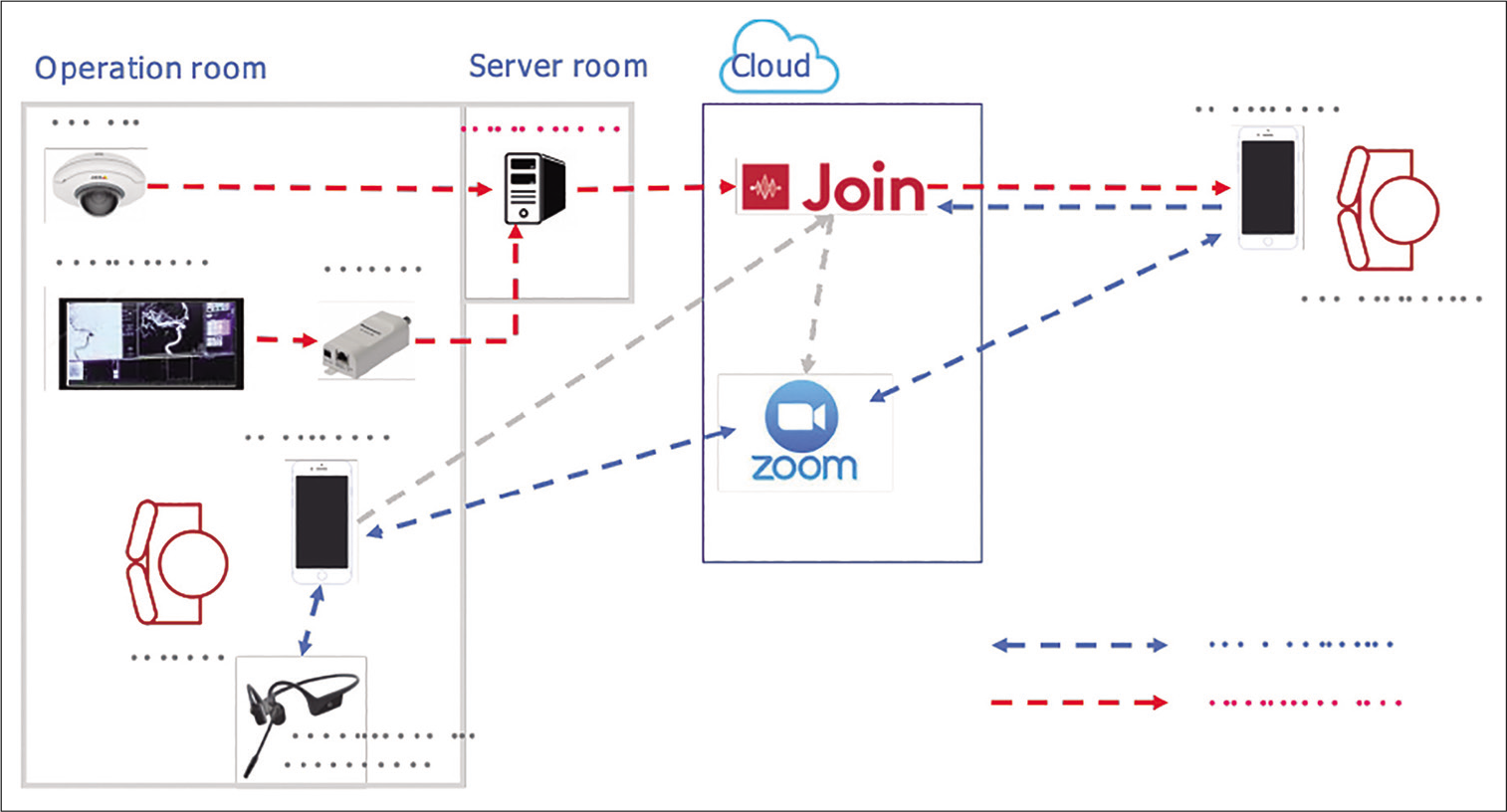
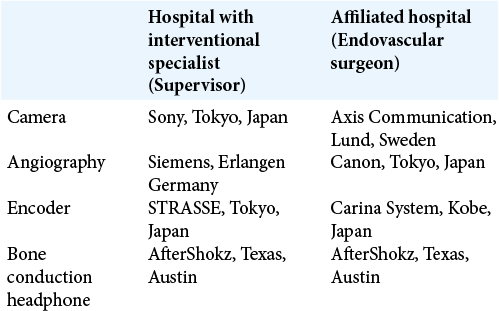
The system consists of 1) a live streaming function for angiography and cameras and 2) a verbal communication function [
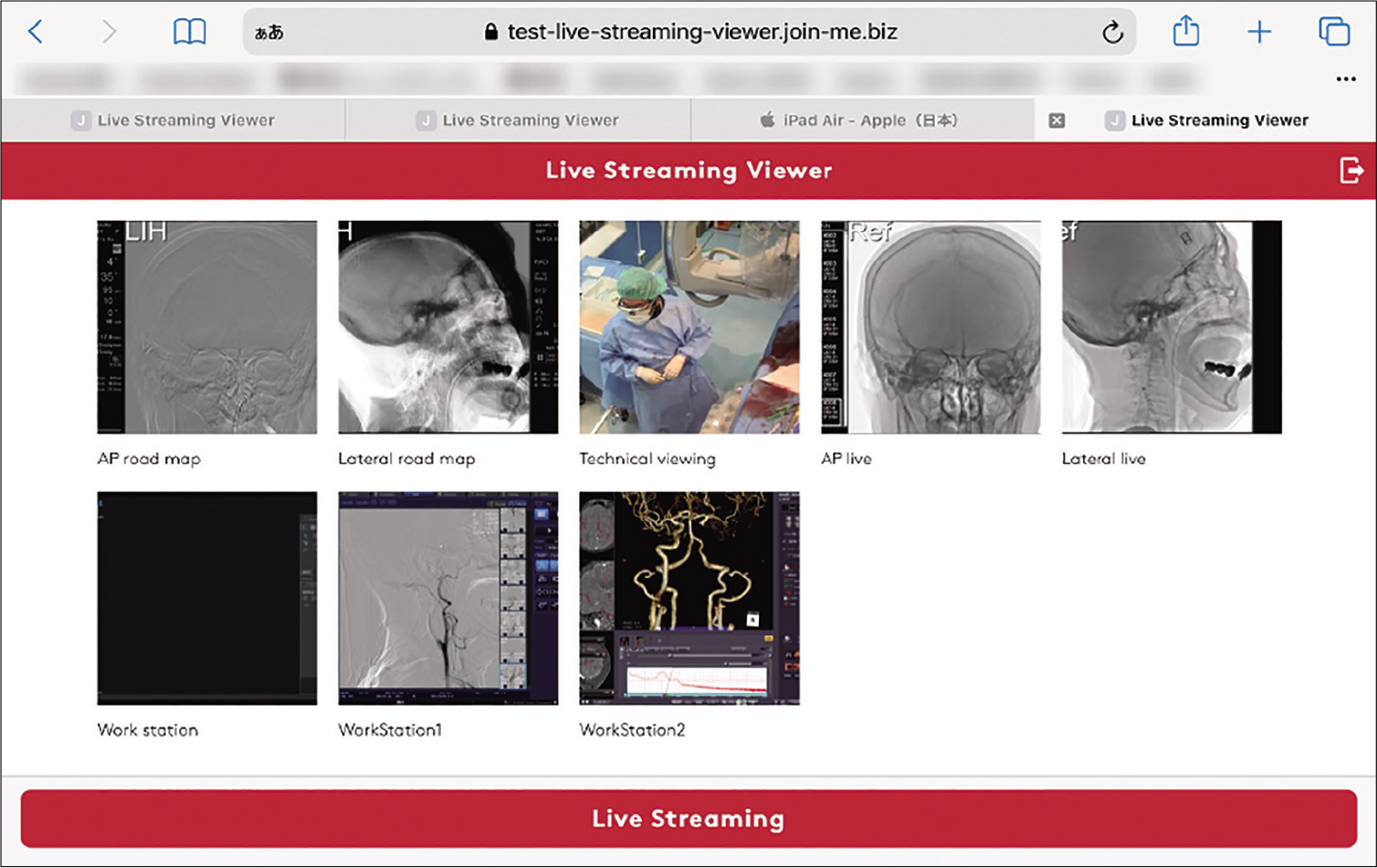
The system allows us to display AP, lateral view; native AP, lateral view; reference AP, lateral view; and workstation images, in addition to the 4K operator’s procedure streaming video camera and the 4K operating room (OR) view video camera on the monitor of any smart devices. A total of eight images can be displayed simultaneously on the iPad (Apple Inc., Cupertino, CA, USA) [
RESULTS
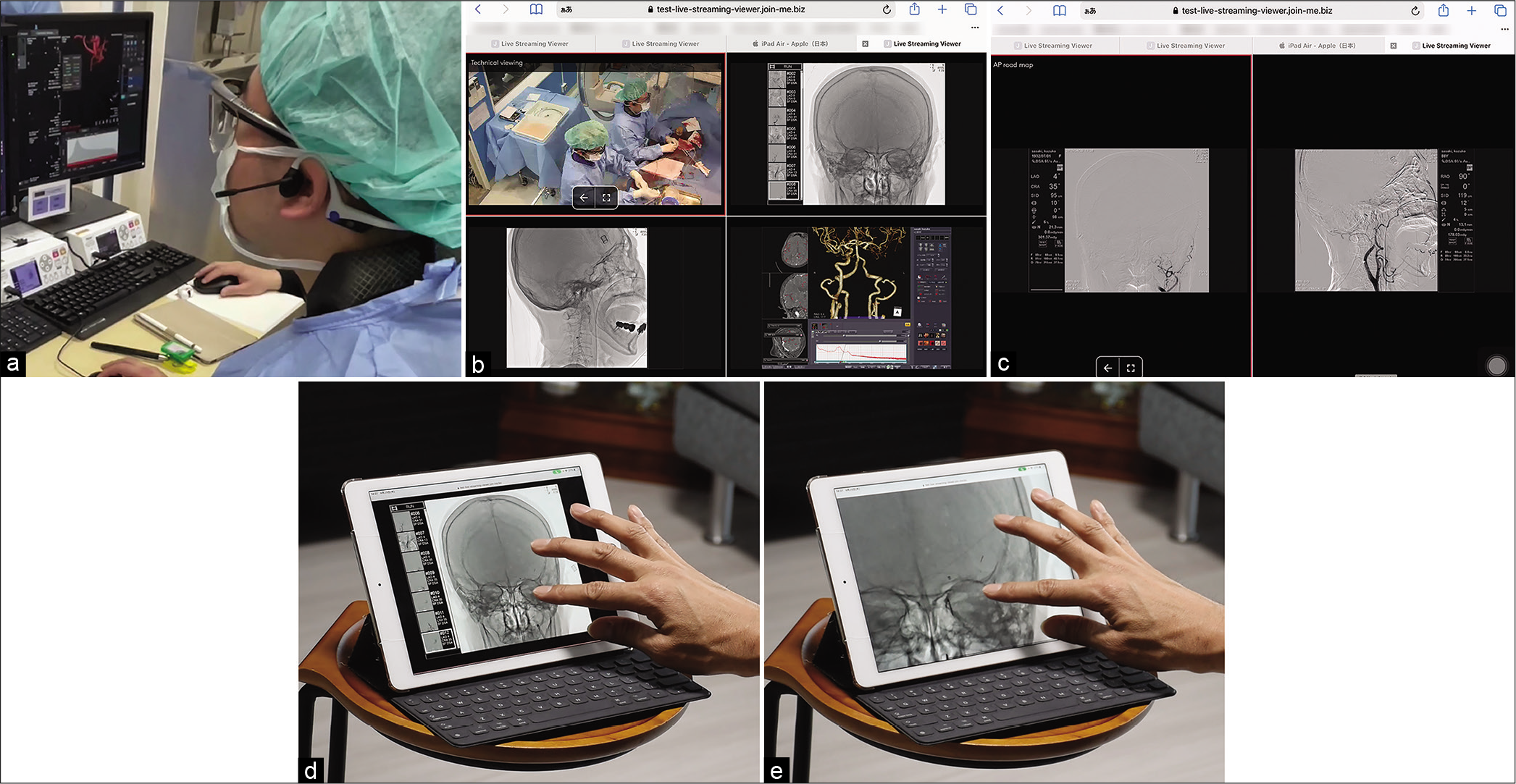
The operator was able to speak with the senior supervisor through a bone conduction headphone and to talk to assistants or radiology technicians without any hearing difficulties [
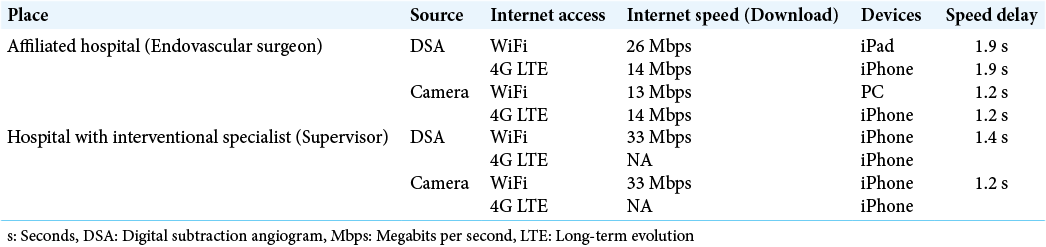
We used 4G Long Term Evolution (LTE) and internet WiFi as the network infrastructure. However, the hospital with the interventional specialist could not use 4G LTE because the radio waves did not reach the OR where we conducted the measurements. The range of delay speed was approximately 1–2 s [
Figure 3:
Acute ischemic stroke supervised at home. Acute ischemic stroke due to the left middle cerebral artery occlusion. Thrombectomy with a stent retriever was performed by neuroendovascular trainees. The operator was able to speak with the senior supervisor through a bone conduction headphone and to talk to assistants or radiology technicians without any hearing difficulties (a). Live streaming images of split monitors on the iPad (b). By selecting areas on images, left ICA occlusion was made clearly visible on the screen (c). The supervisor at home could freely change the size of the image by pinching in and pinching out. The senior physician could supervise the procedure while at home (d and e).
Illustrative case 1
A 73-year-old patient who had an unruptured intracranial IC ophthalmic aneurysm was scheduled for stent-assisted coiling at the affiliated hospital (Kanagawa Prefecture). Under general anesthesia, the guiding system was advanced into the right internal carotid artery (ICA), and the microcatheter was placed in the aneurysm sac. The operator and consultant, who were located at the hospital with the interventional specialist (Tokyo), discussed the treatment strategy by viewing the same 3D workstation before the procedure. The distance between the 2 institutions was 30 miles. The consultant used 2 display systems and advised placing the microcatheter tip at the center of the aneurysm, and subsequently, a low profile visualized intraluminal support stent (Microvention/Termo, Tokyo, Japan) was placed. The consultant detected slight proximal stent corning before the operator realized it because of the high magnification of the image on the iPad (Apple Inc.). All procedures were safety conducted in the same manner as those under conventional supervision. There were no communication errors or image deteriorations during the procedures [
Video 1
Illustrative case 2
An 80-year-old female who presented with hemiparesis was transferred to the affiliated hospital. Her NIHSS scale was 13. CT and imaging work-up demonstrated left ICA occlusion [
DISCUSSION
Telemedicine is a rapidly growing component of the global health-care system under the circumstances of COVID-19.[
Because of a shortage of experienced neuroendovascular specialists, emergency stroke care for stroke intervention is limited. Young neurosurgeons who have just completed fellowships are sometimes dispatched from university hospitals to affiliated local hospitals to cover regional medical services. They need expert supervision when complex stroke patients are transferred to their hospital. However, since the beginning of the COVID-19 pandemic, there have been unprecedented limitations in the movement of people. In such situations, remote consultation systems with real-time audio-visual capability are extremely useful for safe procedures. In this report, we demonstrated the usefulness of a remote supervision system for young physicians. This system has several potentials, such as a two-way education system. Skilled physicians can demonstrate their technique for residents, trainees, or junior attending’s for teaching purposes under restrictions of patient privacy and security. Resident education or device training has also been restricted by hospital infection control. Using this system, trainees can learn the endovascular cutting-edge technique using their own monitoring system, such as the iPad. A similar system was reported by Orru et al.[
One limitation of this system is the requirement for a secure encoder system that connects the hospital DSA/streaming video network. The system anonymizes private patient data, such as the patient’s name or ID. Only the patient’s age and case number are displayed. This system transmits images in an unidentified HIPAA-compliant manner and complies with national guidelines.[
Despite such Japanese HIPPA compliance[
CONCLUSION
Under COVID-19 conditions, a remote consultation system with real-time audio-visual capability may play an important role in acute stroke management while maintaining the quality of patient care.
Ethics approval statements
The study protocol was reviewed and approved by the ethics committee and the research review board at the affiliated hospital. All patients were provided informed consent, and each site had obtained Institutional Review Board approval and signed consent forms. The participants and any identifiable individuals consented to the publication of their image.
Authors’ contributions
All authors have met the four criteria for authorship, as described by the journal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
[Video 1]-Available on
Acknowledgment
All authors thank Mr. Masahiro Kazama for his assistance regarding data equation.
References
1. Bechstein M, Buhk JH, Frölich AM, Broocks G, Hanning U, Erler M. Training and supervision of thrombectomy by remote live streaming support (RESS): Randomized comparison using simulated stroke interventions. Clin Neuroradiol. 2021. 31: 181-7
2. Bechstein M, Elsheikh S, Wodarg F, Taschner CA, Hanning U, Buhk JH. Republished: Interhospital teleproctoring of endovascular intracranial aneurysm treatment using a dedicated live-streaming technology: First experiences during the COVID-19 pandemic. J Neurointerv Surg. 2021. 1: e1
3. Cruz MJ, Nieblas-Bedolla E, Young CC, Feroze AH, Williams JR, Ellenbogen RG. United States medicolegal progress and innovation in telemedicine in the age of COVID-19: A primer for neurosurgeons. Neurosurgery. 2021. 89: 364-71
4. Martins SO, Mont’Alverne F, Rebello LC, Abud DG, Silva GS, Lima FO. Thrombectomy for stroke in the public health care system of Brazil. N Engl J Med. 2020. 382: 2316-26
5. Martins SC, Weiss G, Almeida AG, Brondani R, Carbonera LA, Souza A. Validation of a smartphone application in the evaluation and treatment of acute stroke in a comprehensive stroke center. Stroke. 2020. 51: 240-6
6. Orru’ E, Marosfoi M, Patel NV, Coon AL, Wald C, Repucci N. International teleproctoring in neurointerventional surgery and its potential impact on clinical trials in the era of COVID-19: Legal and technical considerations. J NeuroIntervent Surg. 2020. 13: 1-5
7. Website of the Ministry of Economy. Available from: https://www.meti.go.jp/policy/mono_info_service/healthcare/01gl.pdf [Last accessed on 2021 Nov 22].
8. Sakai K, Sato T, Komatsu T, Mitsumura H, Iguchi Y, Ishibashi T. Communication-type smartphone application can contribute to reducing elapsed time to reperfusion therapy. Neurol Sci. 2021. 26: 1-6
9. Takao H, Murayama Y, Ishibashi T, Karagiozov KL, Abe T. A new support system using a mobile device (smartphone) for diagnostic image display and treatment of stroke. Stroke. 2012. 43: 236-9
10. Takao H, Sakai K, Mitsumura H, Komatsu T, Yuki I, Takeshita K. A smartphone application as a telemedicine tool for stroke care management. Neurol Med Chir (Tokyo). 2021. 61: 260-7
11. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020. 27: 957-62