- Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan,
- Department of Pathology, Juntendo University Urayasu Hospital, Urayasu, Japan.
Correspondence Address:
Satoshi Tsutsumi, Department of Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Japan.
DOI:10.25259/SNI_219_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Satoshi Tsutsumi1, Hiroshi Izumi2, Hisato Ishii1. Isolated idiopathic myositis of the inferior oblique muscle biopsied through lateral orbitotomy. 08-Apr-2022;13:130
How to cite this URL: Satoshi Tsutsumi1, Hiroshi Izumi2, Hisato Ishii1. Isolated idiopathic myositis of the inferior oblique muscle biopsied through lateral orbitotomy. 08-Apr-2022;13:130. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11520
Abstract
Background: Isolated orbital myositis of the inferior oblique muscle (IObM) is rare, with few reported cases.
Case Description: A 65-year-old woman was aware of double vision and left dacryorrhea for 2 months. At presentation, the patient showed mild restriction on the downward gaze. In addition, a subcutaneous mass was palpated on the left eyelid. The blood examination showed normal findings. Cranial computed tomography revealed an isodense mass in the left orbit, located in the inferior, inferolateral, and posterior aspects of the bulb. On magnetic resonance imaging, the mass was well-demarcated, appeared isointense on both T1- and T2-weighted imaging, and was intensely enhanced after intravenous infusion of gadolinium. The patient underwent biopsy through lateral orbitotomy. Microscopically, the resected specimen showed sheet-like proliferation of small round nonneoplastic cells. These cells were positively immunostained for both B- and T-lymphocyte markers. Therefore, we diagnosed the patient with isolated idiopathic myositis of the IObM. The patient was managed with steroids, which resulted in a remarkable resolution of her orbital symptoms.
Conclusion: Biopsy findings should be considered when the presentation of orbital myositis is atypical. Lateral orbitotomy may provide a useful surgical window when approaching the posterior belly of the IObM.
Keywords: Biopsy, Inferior oblique muscle, Lateral orbitotomy, Orbital myositis
INTRODUCTION
Myositis is a common orbital disorder that can affect one or more extraocular muscles. It can develop in association with herpes zoster virus infection, Sjögren’s syndrome, Wegener’s granulomatosis, amyloidosis, dabrafenib and trametinib therapy, or H1N1 influenza vaccinations.[
Among the six extraocular muscles, the superior, lateral, medial, and inferior rectus muscles are frequently affected in orbital myositis, whereas the superior and IObMs are infrequently involved.[
The IObM presents a peculiar anatomy. It arises from the orbital floor, 5.14 ± 1.21 mm posterior to the inferior orbital rim, on a line extending from the infraorbital foramen to 10±0.9 mm inferior to the supraorbital notch that is commonly found along the superomedial orbital rim. The muscle belly of the IObM extends from this origin to its insertion into the posterolateral bulb in an oblique direction.[
Here, we report a probable case of isolated idiopathic myositis of the IObM that was comfortably biopsied through lateral orbitotomy.
CASE PRESENTATION
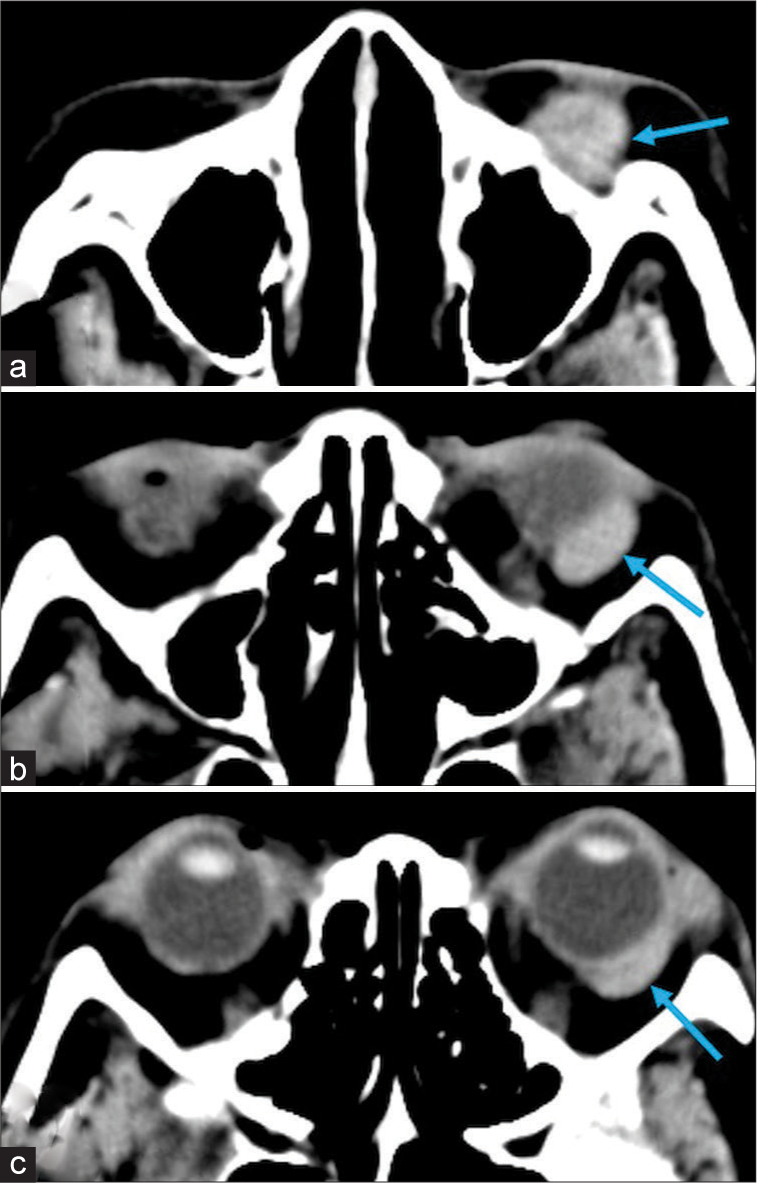
A 65-year-old woman was aware of double vision and left dacryorrhea for 2 months. Her medical history was unremarkable and did not include thyroid disorder, autoimmune disease, amyloidosis, and malignant neoplasms. A local ophthalmologist found a left orbital mass and the patient was referred to our department. At presentation, the patient showed mild restriction on the downward gaze. In addition, a subcutaneous mass was palpated on the left eyelid. The mass was 2 × 1.5 cm in dimension, painless, mobile, and elastic hard. Conjunctival hyperemia and proptosis were not observed. The blood examination showed normal findings. Cranial computed tomography revealed a mass in the anterior part of the left orbit. The mass was isodense relative to the extraocular muscles and located in the inferior, inferolateral, and posterior aspects of the bulb [
Figure 1:
Serial images of noncontrast axial computed tomography scans of the region below the orbital floor (a), at the level of the lower bulb (b), and at the level of the equator of the bulb (c) showing a mass lesion in the anterior part of the left orbit that is isodense relative to the extraocular muscles and located in the inferior (a), inferolateral (b), and posterior (c) aspects of the bulb (arrow). a (inferior)→c (superior).
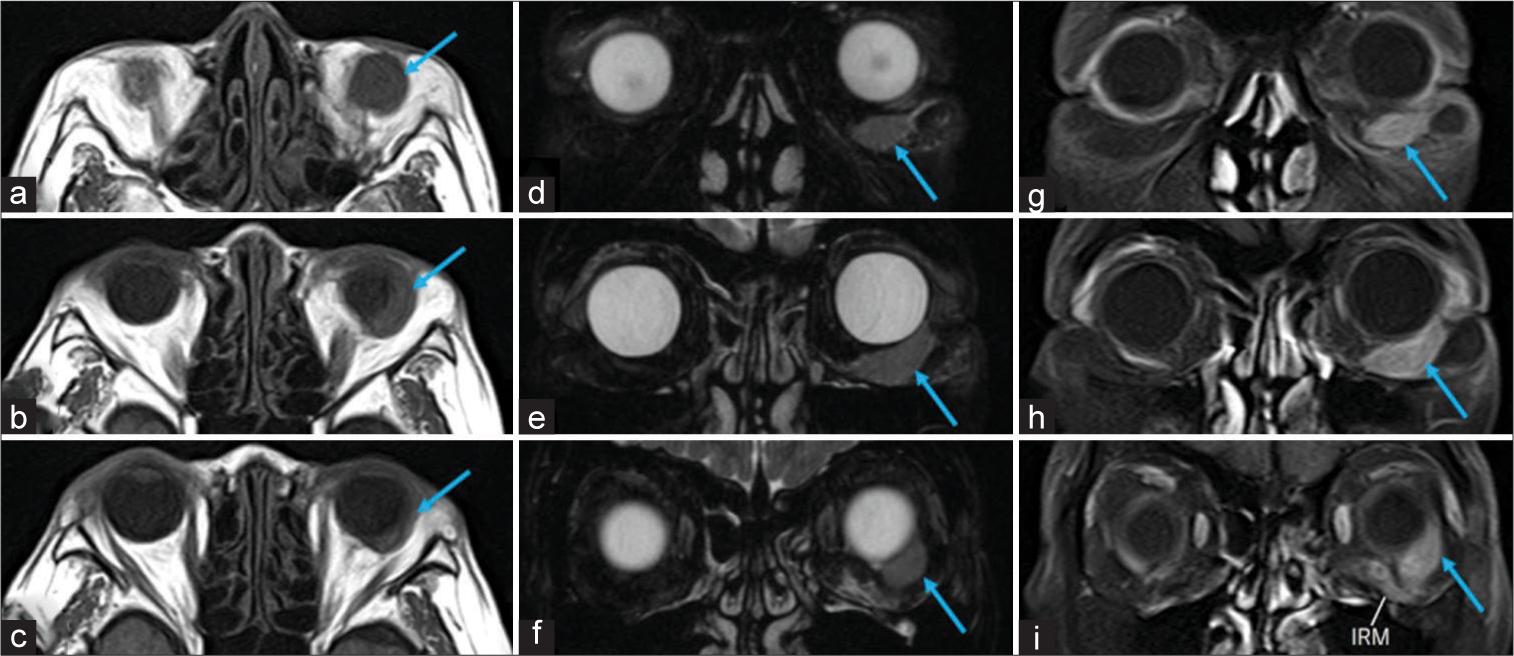
Figure 2:
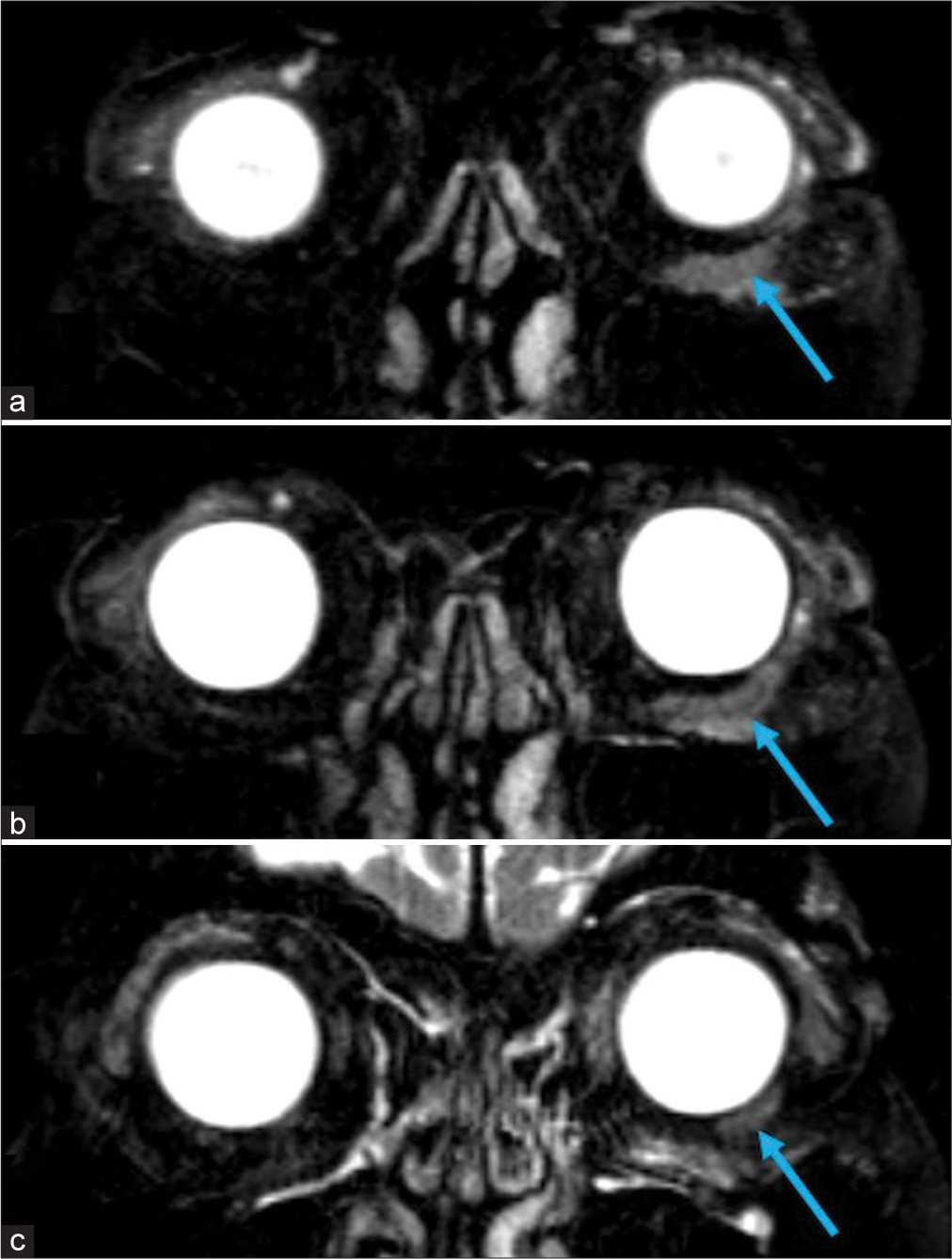
Serial images of the axial T1- (a-c) and T2-weighted (d-f) magnetic resonance imaging (MRI) and postcontrast fat suppression T1-weighted coronal MRI (g-i) showing the left orbital lesion (arrow) that is well-demarcated and separate from the inferior rectus muscle, appearing isointense both on T1- and T2-weighted imaging, and intensely enhanced after intravenous infusion of gadolinium. a (inferior)→c (superior); d (anterior)→f (posterior); g (anterior)→i (posterior).
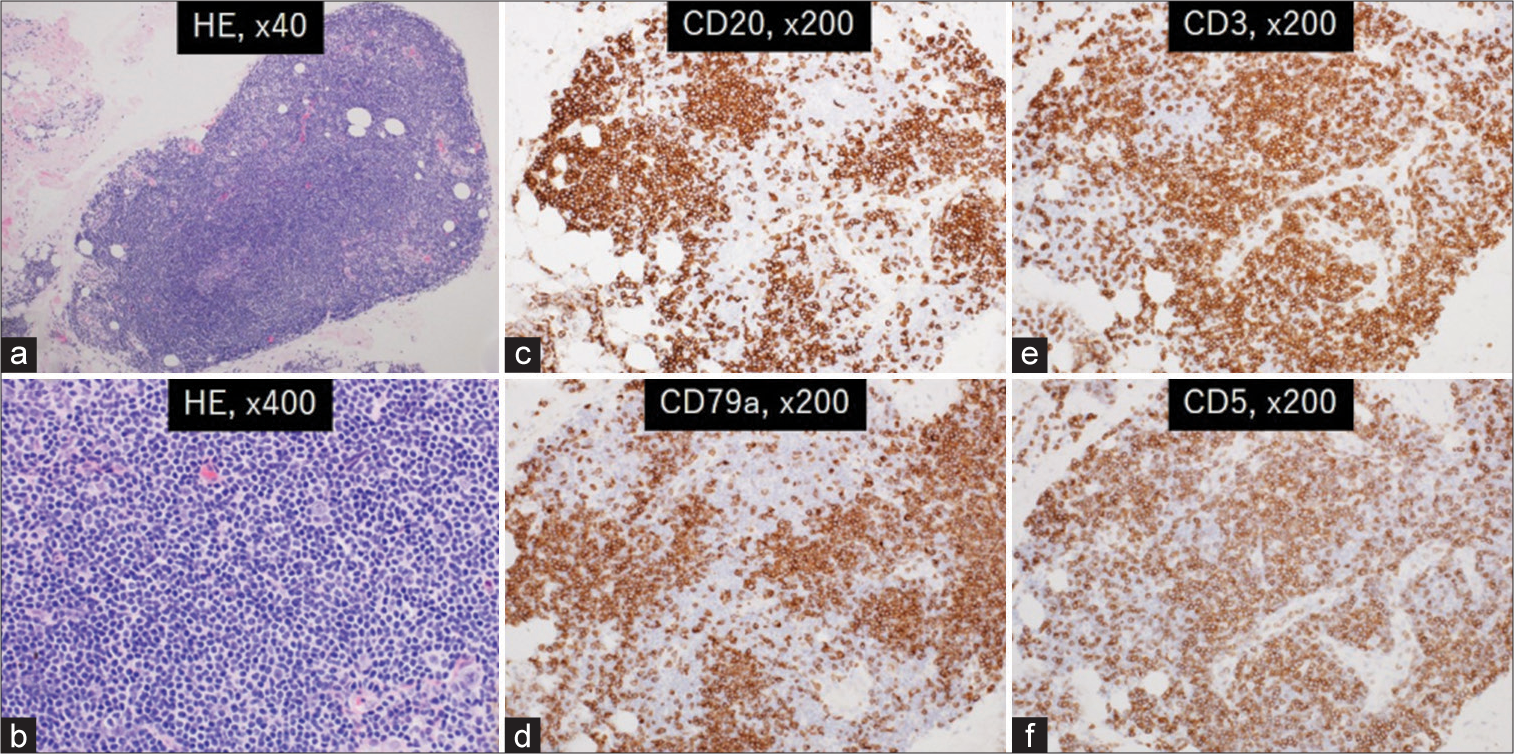
Figure 3:
Photomicrographs of the resected specimens showing sheet-like proliferation of small round cells with a high nuclear-to-cytoplasmic ratio and lacking findings of atypia (a and b). They are positively stained for CD20 (c) and CD79a (d) markers specific for B-lymphocytes, as well as CD3 (e) and CD5 (f) markers specific for T-lymphocytes. HE: Hematoxylin and eosin stain.
DISCUSSION
In the present case, there was no medical history relevant to orbital myositis with a normal blood profile. On neuroimaging, only the IObM appeared swollen among the six extraocular muscles with intense contrast enhancement. Furthermore, the histopathological findings of the resected specimen were consistent with orbital myositis represented by the proliferation of nonneoplastic B- and T-lymphocytes. The lesion responded well to steroid therapy. Therefore, we finally diagnosed as isolated idiopathic myositis of the IObM. As idiopathic orbital myositis may recur with a high probability, long-term follow-up is necessary after the initial remission.[
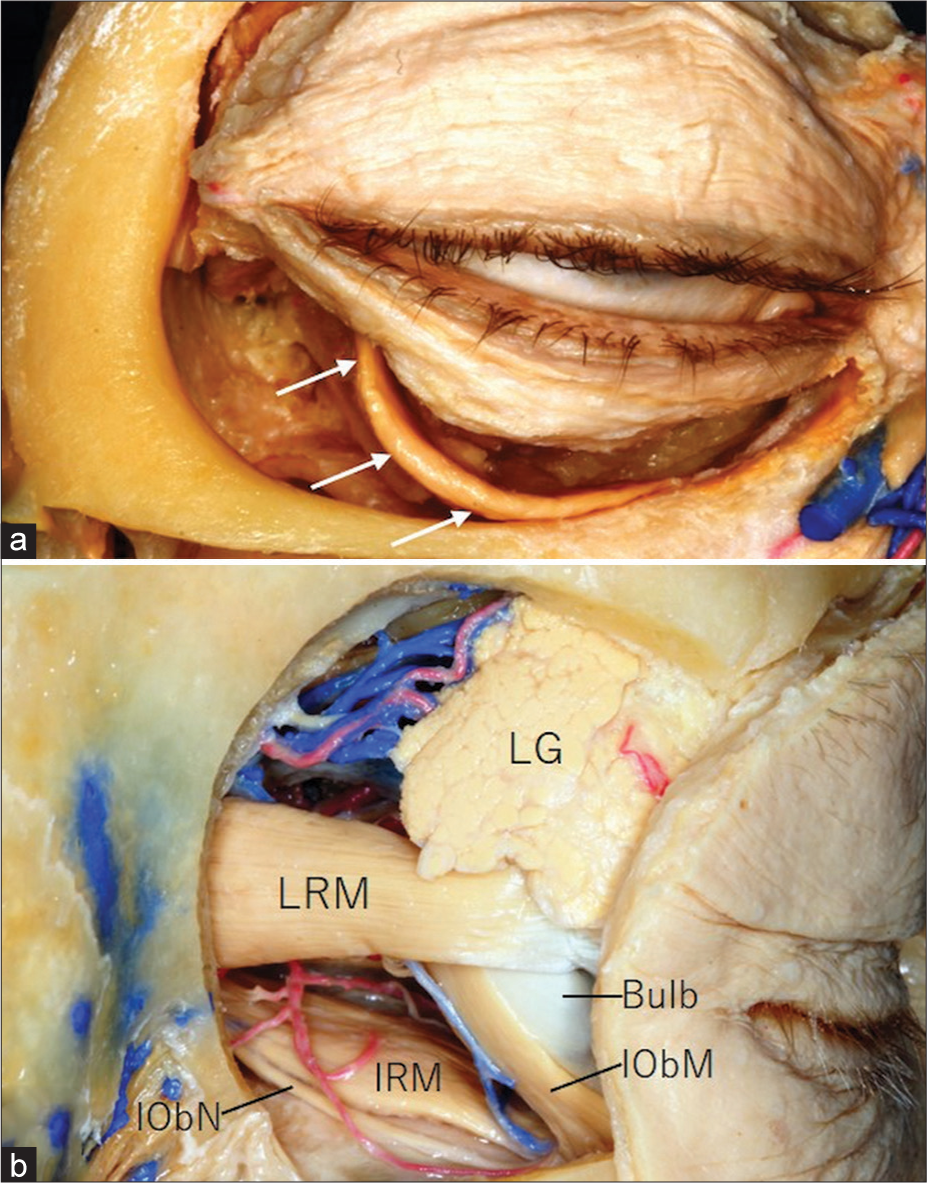
The IObM, located in the anterior part of the orbit, can be accessed from both anterior and lateral aspects. In the anterior aspect, the anterior belly of the IObM can be percutaneously exposed, without creating a bony window. The lateral part of the belly, which is thicker than the medial part and courses separately from the orbital floor, may be a suitable site for safe biopsy [
Figure 5:
Cadaver dissections showing specimens of the right orbits viewed from the anterior aspect (a) and through a lateral orbitotomy (b) showing the inferior oblique muscle and relevant structures. IObM: Inferior oblique muscle; IObN: Inferior oblique nerve; IRM: Inferior rectus muscle; LG: Lacrimal gland; LRM: Lateral rectus muscle; Arrows: belly of the inferior oblique muscle. a and b: personal pictures.
CONCLUSION
A muscle biopsy should be considered when the presentation of orbital myositis is atypical. Lateral orbitotomy may provide a useful surgical window when approaching the posterior belly of the IObM.
Declaration of patient consent
The authors certify that they have obtained appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. AlKhalifah M, Aloulah MO, Al-Faky YH. Superior oblique myositis mimics a subperiosteal abscess in a patient with sinusitis. Arq Bras Oftalmol. 2021. 84: 503-5
2. Artsi EB, McKelvie PA, McNab AA. Histopathologic findings in idiopathic orbital myositis. Ophthalmology. 2021. 128: 609-16
3. Badilla J, Dolman PJ. Orbital myositis involving the oblique muscles associated with herpes zoster ophthalmicus. Ophthalmic Plast Reconstr Surg. 2007. 23: 411-3
4. Basilious A, Jivraj I, DeAngelis D. Acute unilateral ptosis and myositis following the H1N1 influenza vaccine. Ophthalmic Plast Reconstr Surg. 2020. 36: e16-7
5. Fleischmann R, Assmann A, Bohner G, Ruprecht K. Isolated myositis of the superior oblique muscle. J Neurol Neurosurg Psychiatry. 2013. 84: 402-3
6. Lahoud S, Brownstein S, Barsoum-Homsy M. Inferior oblique myositis presenting as superior oblique muscle palsy. Can J Ophthalmol. 1988. 23: 124-7
7. Moon JS, Shin SY. Superior oblique myositis causing acquired Brown’s syndrome as the first manifestation of primary Sjögren’s syndrome. Clin Exp Rheumatol. 2018. 112: 237-8
8. Mowlavi A, Neumeister MW, Wilhelmi BJ. Lower blepharoplasty using bony anatomical landmarks to identify and avoid injury to the inferior oblique muscle. Plast Reconstr Surg. 2002. 110: 1318-24
9. Paula JS, Paula SA, Cruz AA, Chahud F. Superior oblique muscle amyloidosis mimicking myositis. Ophthalmic Plast Reconstr Surg. 2008. 24: 77-9
10. Salam A, Meligonis G, Malhotra R. Superior oblique myositis as an early feature of orbital Wegener’s granulomatosis. Orbit. 2008. 27: 203-6
11. Shin HJ, Shin KJ, Lee SH, Koh KS, Song WC, Gil YC. Location of the inferior oblique muscle origin with reference to the lacrimal caruncle and its significance in oculofacial surgery. Br J Ophthalmol. 2016. 100: 179-83
12. Spindle J, Narang S, Purewal B, Shinder R. Atypical idiopathic orbital inflammation in a young girl. Ophthalmic Plast Reconstr Surg. 2013. 29: e86-8
13. Stidham DB, Sondhi N, Plager D, Helveston E. Presumed isolated inflammation of the superior oblique muscle in idiopathic orbital myositis. Ophthalmology. 1998. 105: 2216-9
14. Tseng AM, Peng ET, Bindiganavile SH, Raviskanthan S, Bhat N, Mortensen PW. Superior oblique myositis following targeted therapy for papillary thyroid carcinoma. Can J Ophthalmol. 2021. 56: e125-7
15. Tsutsumi S, Nakamura M, Tabuchi T, Yasumoto Y, Ito M. An anatomic study of the inferior oblique nerve with high-resolution magnetic resonance imaging. Surg Radiol Anat. 2013. 35: 377-83
16. Tychsen L, Tse DT, Ossoinig K, Anderson RL. Trochleitis with superior oblique myositis. Ophthalmology. 1984. 91: 1075-9
17. Wan WL, Cano MR, Green RL. Orbital myositis involving the oblique muscles. An echographic study. Ophthalmology. 1988. 95: 1522-8
18. Yalçin B, Ozan H. Insertional pattern of the inferior oblique muscle. Am J Ophthalmol. 2005. 139: 504-8
19. Yan J, Wu P. Idiopathic orbital myositis. J Craniofac Surg. 2014. 25: 884-7