- Department of Surgery, Hull University Teaching Hospitals NHS Trust, Anlaby Road, Hull,
- Department of Health Sciences, University of York, York,
- Peninsula Medical School, Faculty of Health, University of Plymouth, Plymouth Science Park, Plymouth,
- Southwest Neurosurgery Centre, University Hospitals Plymouth NHS Trust, Plymouth, United Kingdom.
Correspondence Address:
Temidayo Osunronbi, Department of Surgery, Hull University Teaching Hospitals NHS Trust, Hull, United Kingdom.
DOI:10.25259/SNI_160_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Temidayo Osunronbi1,2, Balint Borbas3, Hiba Lusta3, Agbolahan Sofela4, Himanshu Sharma4. Preoperative lymphocyte percentage and neutrophil-lymphocyte ratio are useful predictors of 30-day postoperative complications after lumbar fusion. 15-Apr-2022;13:145
How to cite this URL: Temidayo Osunronbi1,2, Balint Borbas3, Hiba Lusta3, Agbolahan Sofela4, Himanshu Sharma4. Preoperative lymphocyte percentage and neutrophil-lymphocyte ratio are useful predictors of 30-day postoperative complications after lumbar fusion. 15-Apr-2022;13:145. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11538
Abstract
Background: Lymphocyte percentage/count, platelet-lymphocyte ratio (PLR), and neutrophil-lymphocyte ratio (NLR) have shown prognostic significance in patients with cancer, stroke, and following cardiac surgery. However, the utility of these blood parameters for assessing the 30-day postoperative risk for lumbar fusion complications has not been established.
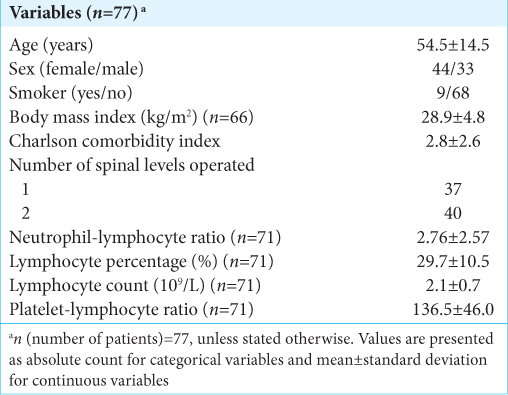
Methods: In this single-center-single-surgeon retrospective series, 77 consecutive patients underwent one- or two-level lumbar fusion. Lymphocyte percentage/count, PLR, and NLR were investigated as predictors of 30-day postoperative complications.
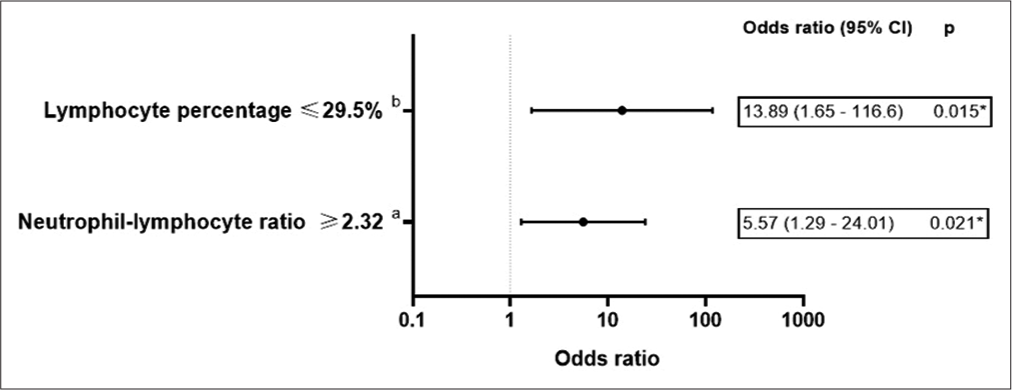
Results: Ten of 77 patients had postoperative complications. A unit increase in NLR and lymphocyte percentage was significantly associated with a 23% increase and 7% decrease, respectively, in the odds of a complication occurring. Preoperative NLR ≥ 2.32 and lymphocyte percentage ≤ 29.5% significantly discriminated between the “complication” and “no-complication” groups.
Conclusion: Patients with a preoperative lymphocyte percentage of ≤29.5% and/or NLR ≥2.32 should be closely monitored as high-risk groups susceptible to 30-day postoperative complications after lumbar fusion.
Keywords: Complications, Lymphocyte, Neutrophil, Prognosis, Spinal fusion
INTRODUCTION
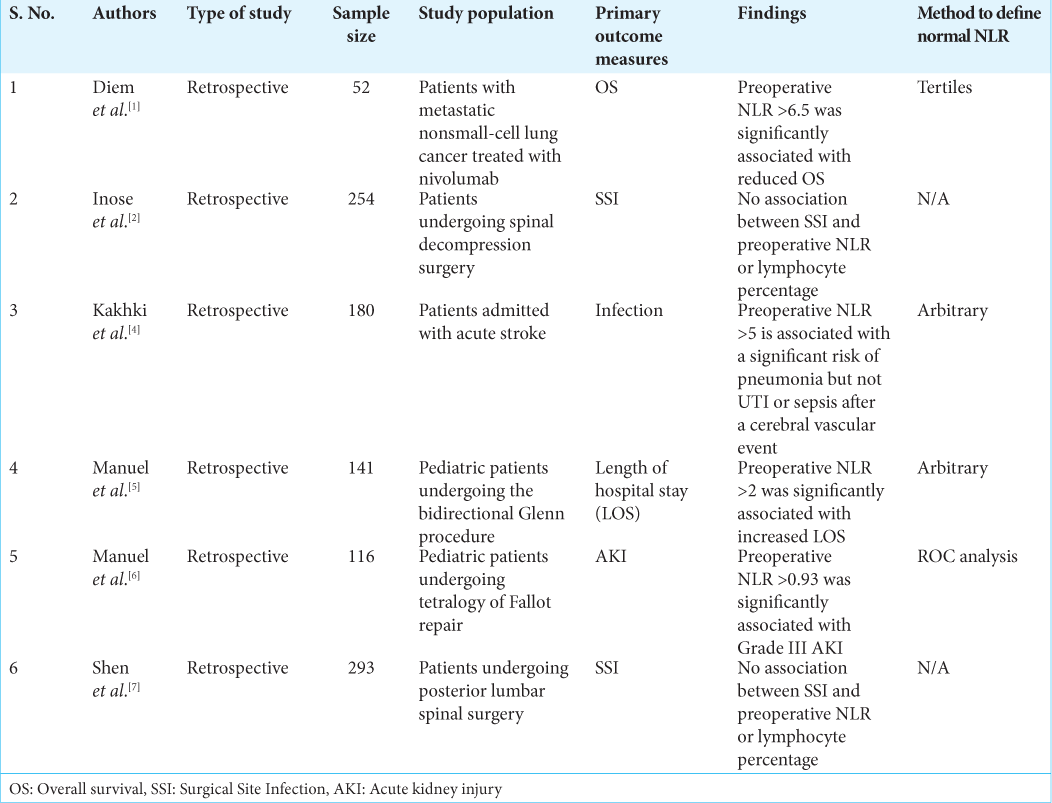
The importance of preadmission/preoperative lymphocyte percentage/count, platelet-lymphocyte ratio (PLR), and neutrophil-lymphocyte ratio (NLR) as prognostic markers following cardiac surgery, stroke, and cancers has been extensively reported.[
MATERIALS AND METHODS
Study design
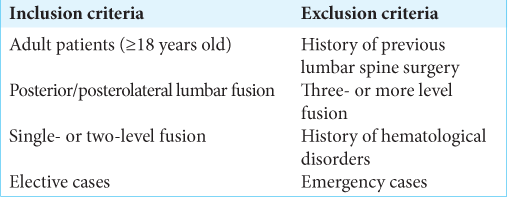
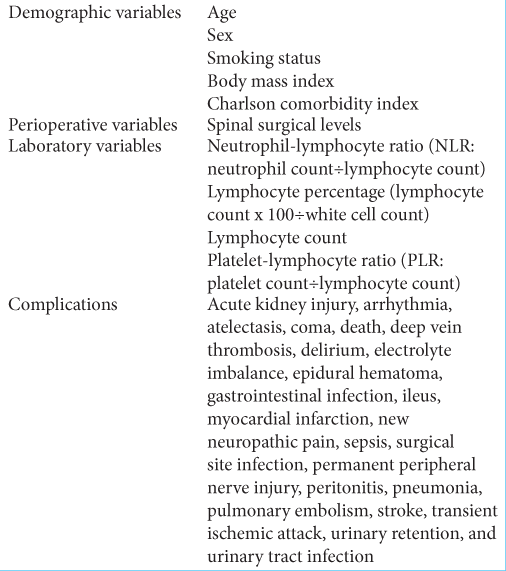
In this case–control study, 77 adults underwent elective single- (37 patients) or two-level (40 patients) posterior/posterolateral lumbar fusion performed by one surgeon (2012–2019) [
Statistical analysis
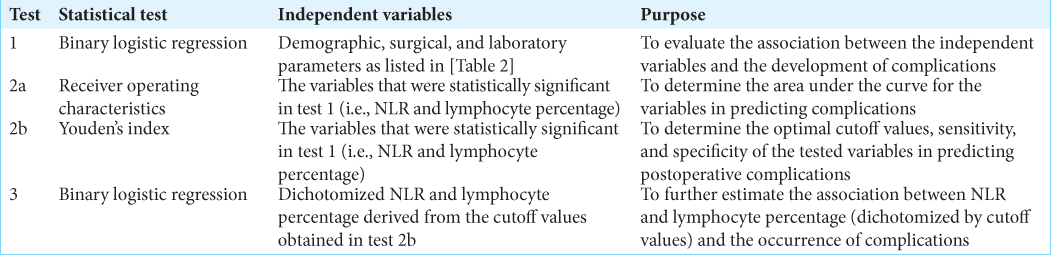
Statistical analysis was performed on IBM SPSS Statistics 27 (Windows). Binary logistic regression, receiver operating characteristics, and Youden’s index were utilized [
RESULTS
Correlation between 30-day postoperative complications and lymphocyte percentage and NLR
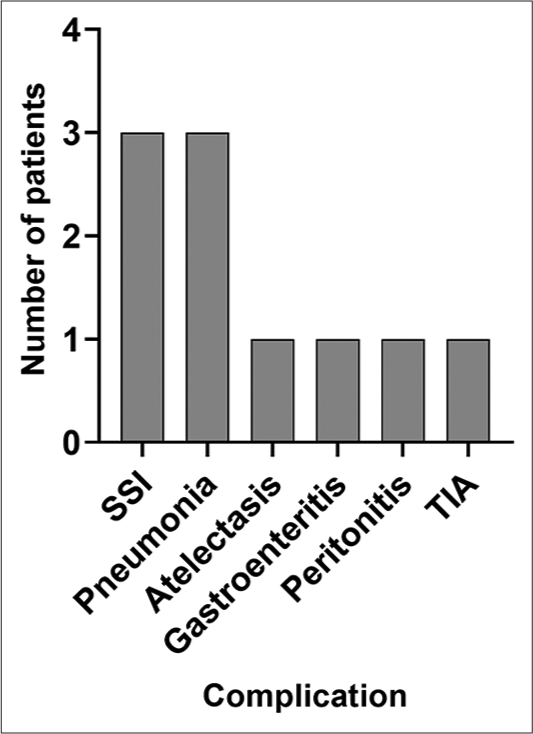
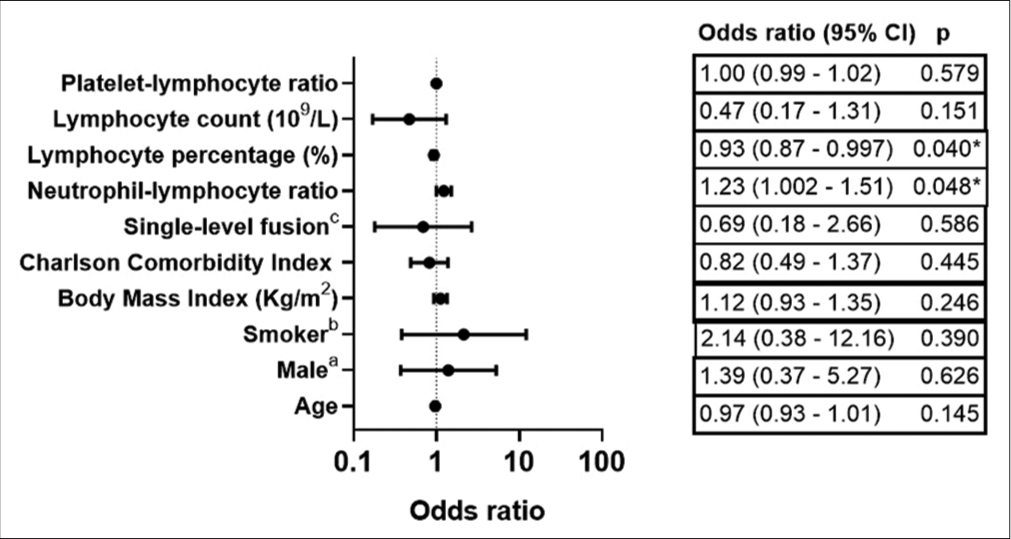
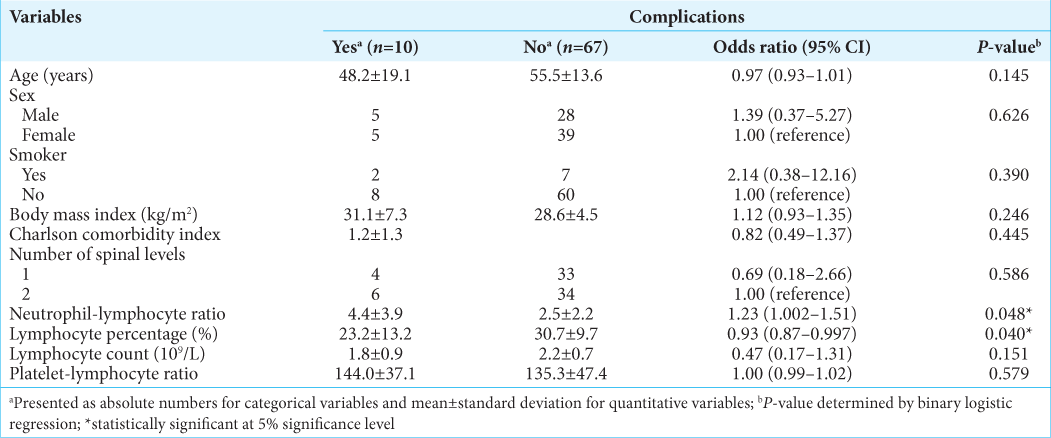
[
Predictive value of preoperative lymphocyte percentage and NLR for determining 30-day postoperative complications
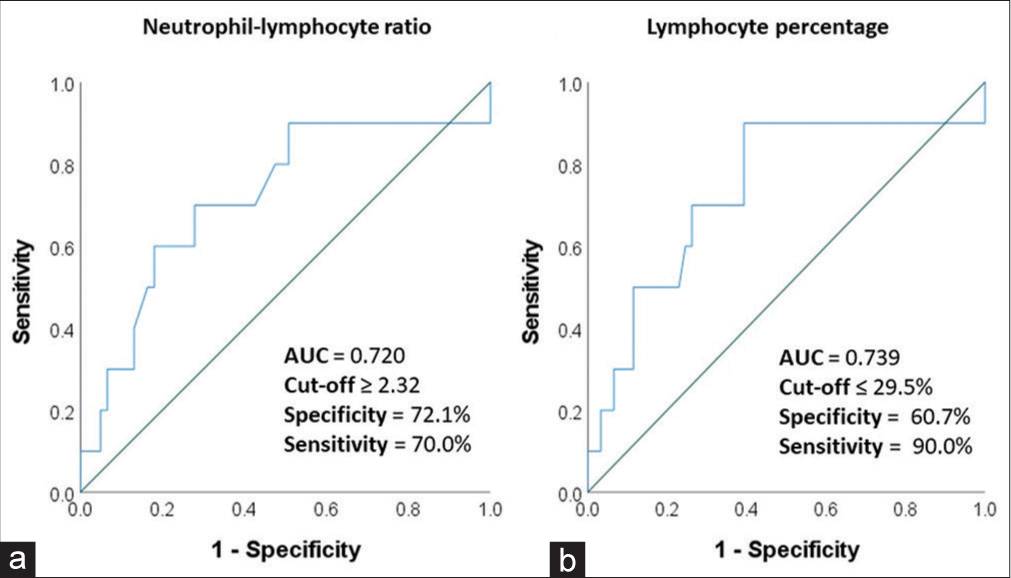
The area under the curve values for the preoperative NLR and lymphocyte percentage were in the “acceptable” range (0.7–0.8) of prognostic accuracy for postoperative 30-day complications. The optimal cutoff value for preoperative NLR and lymphocyte percentage were ≥2.32 and ≤29.5%, respectively [
DISCUSSION
We investigated the preoperative predictors of postoperative complications after lumbar fusion. Patients with preoperative lymphocyte percentage ≤29.5% and/or NLR ≥ 2.32 had a higher risk of developing postoperative complications. Other studies have reported similar findings (i.e., high baseline/ preoperative NLR and lymphocytopenia were predictors of worse outcomes).[
CONCLUSION
A raised NLR (≥2.32) and/or decreased lymphocyte percentage (≤29.5%) at baseline predict the development of postoperative complications after lumbar fusion.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W. Neutrophil-to-lymphocyte ratio (NLR) and platelet-tolymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017. 111: 176-81
2. Inose H, Kobayashi Y, Yuasa M, Hirai T, Yoshii T, Okawa A. Postoperative lymphocyte percentage and neutrophillymphocyte ratio are useful markers for the early prediction of surgical site infection in spinal decompression surgery. J Orthop Surg. 2020. 28: 2309499020918402
3. Iwata E, Shigematsu H, Okuda A, Morimoto Y, Masuda K, Nakajima H. Lymphopenia at 4 days postoperatively is the most significant laboratory marker for early detection of surgical site infection following posterior lumbar instrumentation surgery. Asian Spine J. 2016. 10: 1042-6
4. Kakhki RD, Dehghanei M, ArefNezhad R, Motedayyen H. The predicting role of neutrophil lymphocyte ratio in patients with acute ischemic and hemorrhagic stroke. J Stroke Cerebrovasc Dis. 2020. 29: 105233
5. Manuel V, Miana LA, Guerreiro GP, Tenório DF, Turquetto A, Penha JG. Prognostic value of the preoperative neutrophil-lymphocyte ratio in patients undergoing the bidirectional Glenn procedure. J Card Surg. 2020. 35: 328-34
6. Manuel V, Miana LA, Turquetto A, Guerreiro GP, Fernandes N, Jatene MB. The role of the neutrophil-lymphocyte ratio for pre-operative risk stratification of acute kidney injury after tetralogy of Fallot repair. Cardiol Young. 2021. 31: 1009-14
7. Shen CJ, Miao T, Wang ZF, Li ZF, Huang LQ, Chen TT. Predictive value of post-operative neutrophil/lymphocyte count ratio for surgical site infection in patients following posterior lumbar spinal surgery. Int Immunopharmacol. 2019. 74: 105705
8. Wu X, Luo Q, Su Z, Li Y, Wang H, Yuan S. Prognostic value of preoperative absolute lymphocyte count in children with tetralogy of fallot. J Am Heart Assoc. 2021. 10: e019098