- Department of Orthopedics, Seth G. S. Medical College and KEM Hospital, Mumbai, Maharashtra, India.
Correspondence Address:
Shivaprasad Sharangouda Kolur, Department of Orthopedics, Seth G. S. Medical College and KEM Hospital, Mumbai, Maharashtra, India.
DOI:10.25259/SNI_167_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tushar Narayan Rathod, Shivaprasad Sharangouda Kolur, Vinod Kumar Yadav, Rudra Mangesh Prabhu. Functional outcomes in the management of cervicothoracic junction tuberculosis. 13-May-2022;13:198
How to cite this URL: Tushar Narayan Rathod, Shivaprasad Sharangouda Kolur, Vinod Kumar Yadav, Rudra Mangesh Prabhu. Functional outcomes in the management of cervicothoracic junction tuberculosis. 13-May-2022;13:198. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11592
Abstract
Background: We analyzed the clinical and radiological parameters influencing functional outcomes and neurological recovery in patients with cervicothoracic junctional tuberculosis (TB).
Methods: This was a retrospective analysis of 16 cases of cervicothoracic junction (CTJ) spinal TB; 11 patients were managed operatively, while five were managed conservatively. Patients’ outcomes were assessed at 1 month, 1 year, and yearly thereafter and included an analysis of multiple outcome scores, various radiographic parameters, and sensitivity or resistance to anti-tubercular therapy.
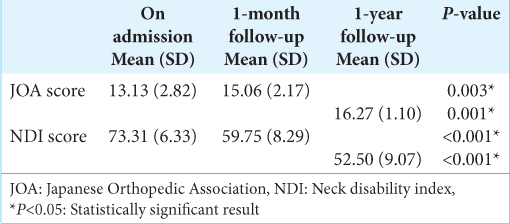
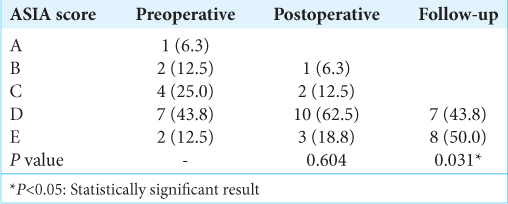
Results: Patients averaged 25.94 years of age, and typically had three-level vertebral involvement. They were followed for a mean duration of 24 months, and the duration of anti-tubercular therapy averaged 17 months. Patients demonstrated clinical improvement on Japanese Orthopedic Association score and Neck disability index (P P > 0.05) at the end of 1 year.
Conclusion: Tuberculous affection of the dynamic CTJ is a challenging scenario in clinical practice and its management involves consideration of disease extent, neurological status, and effort toward restoration of normal alignment of spine in sagittal and coronal plane to get favorable clinical outcomes.
Keywords: ASIA, Cervical sagittal alignment, Cervicothoracic junction, Neck disability index, Thoracic inlet measurement, Tuberculosis
INTRODUCTION
Most cases of spinal tuberculosis (TB) involve the thoracolumbar, followed by the lumbar region, and finally, the cervical region (i.e., <5% of cases).[
MATERIALS AND METHODS
We prospectively evaluated 16 patients with CTJ (i.e., including C7/T1 or both) TB (2015–2020). They averaged 25.94 years of age and had between 1 and 6 vertebral bodies involvement. Of the 16 patients, 11 had surgery, while five were treated conservatively. A diagnosis of TB of the spine was based on microbiologically proven TB (BACTEC MGIT and GeneXpert) with a histopathological confirmation in the operated patients. In the conservatively managed group, the diagnosis was based on radiographic imaging (X-rays and MRI), hematological parameters, and constitutional symptoms. All the patients underwent serial evaluations at admission, 1 month, 1 year, and yearly thereafter. MR studies and supine radiographs were utilized to determine the extent of CTJ involvement and measure the cervicothoracic sagittal parameters.
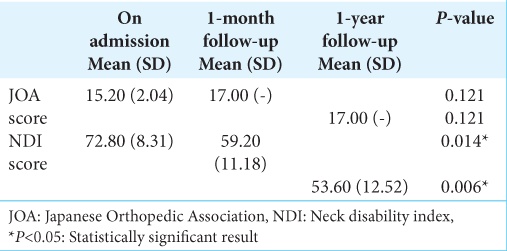
Assessment of outcome scores
Three outcome measures were used to assess these 16 patients and were documented on admission, at 1 month, 1 year and in the subsequent years. The neck disability index (NDI) was used for the subjective evaluation of the distability experienced.[
Indications for surgery in 11 patients with CTJTB
Indications for surgery in 11 patients included progressive neurological worsening, significant static neurological deficits, kyphotic deformity, biomechanical instability, bowel bladder involvement, and an inadequate response to chemotherapy. Anterior approach (8) consisting of anterior debridement and fusion with tricortical graft or mesh cage, and anterior cervical plate was used.[
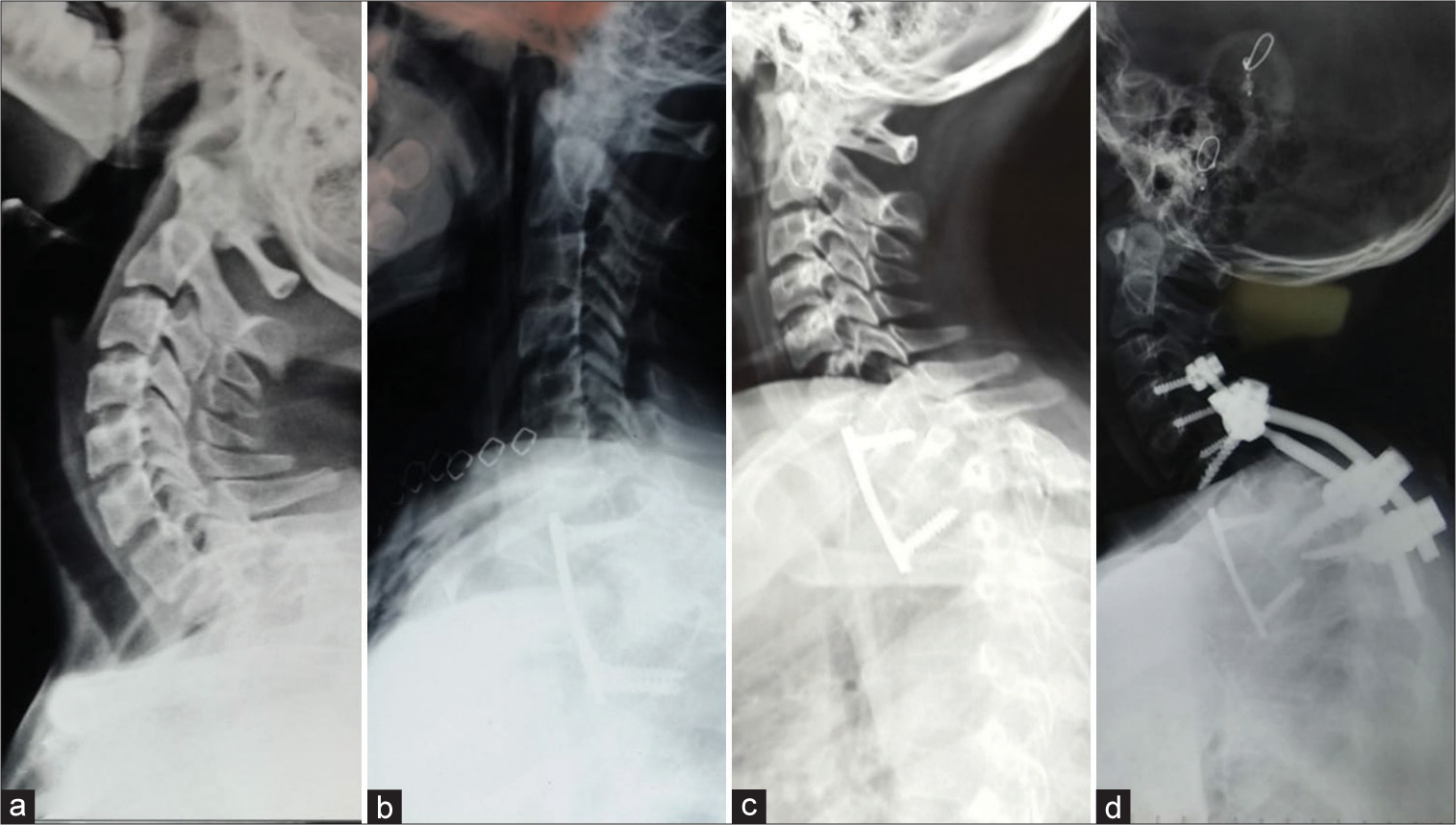
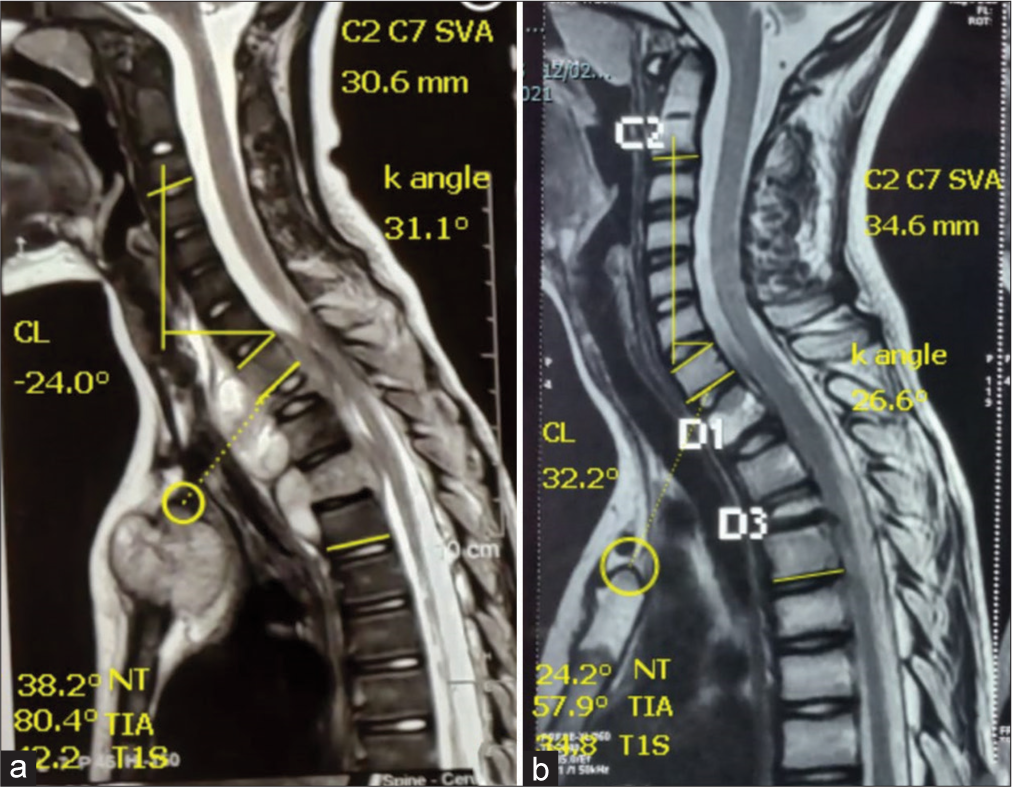
Figure 1:
(a) Radiograph showing CTJ kyphosis with hyperlordosis of the cervical spine, (b) anterior cervical plate in situ with caudally directed inferior screws, (c) anterior cervical plate in situ with cephalad directed inferior screws depicting increased kyphosis due to unabated posterior column growth, and (d) correction of kyphosis with additional posterior instrumentation.
Postoperative management
Postoperatively, patients received rehabilitation and bracing (i.e., with cervical extension) until bony fusion was documented on serial radiographs. Patients were assessed with serial supine radiographs at monthly intervals for the 1st year and yearly thereafter.
RESULTS
Outcomes for 11 surgical patients
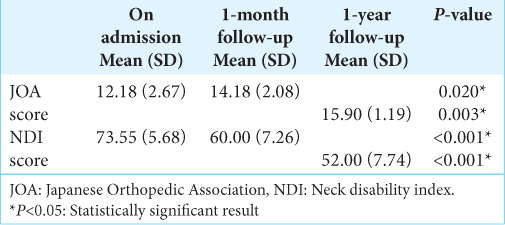
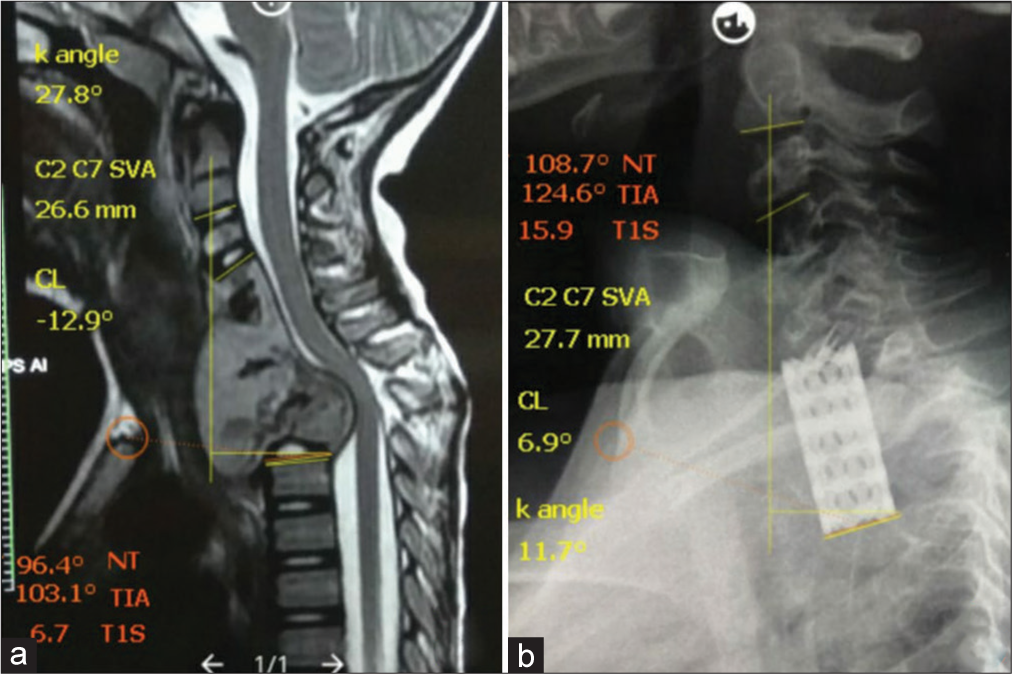
At the end of 1 year, the mean JOA and NDI improved from 12.18 to 14.18 and 73.55 to 60.00 at the end of 1 month follow-up, and to 15.90 and 52.00 at the end of 1 year, respectively [
Sensitivity to antitubercular therapy
Fourteen (87.5%) patients were sensitive to the first line of anti-tubercular therapy, while one patient showed multidrug-resistant Koch’s and one extensively drug-resistant TB (MTB strain resistant to even second line of anti-tubercular drugs). The mean duration of anti-tubercular therapy was 17 ± 4.75 months.
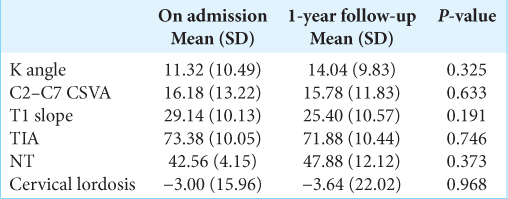
Postoperative radiological improvement in 11 surgically treated cases of CTJTB
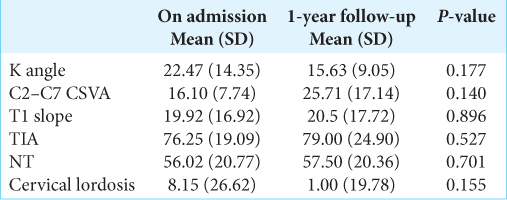
Patients undergoing cervicothoracic corrective surgery for TB exhibited the following changes in their mean cervical sagittal parameters, postoperatively. Segmental kyphotic angle (K), and cervical lordosis improved; C2–C7 sagittal vertical axis decreased; T1 slope, thoracic inlet angle, and neck tilt showed an increase [
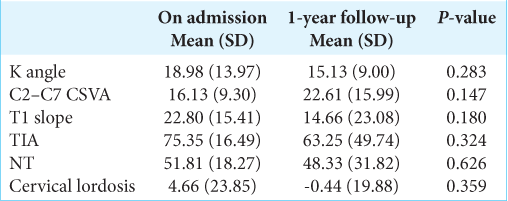
Nonoperative results in five patients
The five patients treated without surgery showed improvement in the NDI score at 1-month and 1-year follow-up, as well as in the JOA score [
Results from the entire cohort
Analysis of all the 16 patients showed that the cervicothoracic sagittal parameters varied from admission to 1-year follow up as follows, segmental kyphotic angle(K) changed from 18.98° to 15.13°; C2-C7SVA from 16.13mm to 22.61mm; CL from 4.66° to -0.44°. T1S from 22.80° to 14.66°; TIA from 75.35° to 63.25°; NT from 51.81° to 48.33° (P>0.05) [
DISCUSSION
Surgery for CTJTB
The literature on CTJTB is scant and surgery for CTJTB poses a unique challenge. Anti-tubercular therapy is the mainstay of treatment with or without surgical debridement and stabilization. Li et al. reported favorable outcomes in 34 patients undergoing decompression and posterior instrumentation for CTJ metastases.[
Conservative management of CTJTB
For those treated non surgically, on follow-up, they showed an increase in the kyphotic angle, reduction in T1 slope, and increase in neck tilt probably due to settling of the diseased segment. We attribute the improvement in NDI, ASIA, and JOA scores to neurological decompression and eradication of the tubercular focus by timely institution of anti-tubercular therapy along with bracing.
Most of our patients at the time of presentation had not received any disease-specific treatment because of resource constraints and lack of access to quality health-care services and usually presented to us late with severe kyphosis and neurological deficit with various grades of functional dependence. Anterior approaches offer limited control in realigning the spine in contrast to posterior or combined approaches. Hence, we did not get significant alteration in the radiological parameters as the primary surgical goal was to do neurological decompression with the best possible realignment of spine because patients in our cohort presented quite late in the natural course of disease progression. The author strongly believes that compensatory mechanisms existing at the occipitocervical junction, thoracolumbar junction, and lumbopelvic junction play an important role in reducing the impact of these altered parameters on the overall global sagittal alignment to maintain the cone of economy.
CONCLUSION
CTJTB is a challenging scenario in clinical practice and has favorable outcomes if managed appropriately. Alterations in cervical sagittal parameters and thoracic inlet measurements did not have a significant bearing on the functional outcome in short term.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Jain A, Sreenivasan R, Mukunth R, Dhammi I. Tubercular spondylitis in children. Indian J Orthop. 2014. 48: 136-44
2. Kato S, Oshima Y, Oka H, Chikuda H, Takeshita Y, Miyoshi K. Comparison of the Japanese orthopaedic association (JOA) score and modified JOA (mJOA) score for the assessment of cervical myelopathy: A multicenter observational study. PLoS One. 2015. 10: e0123022
3. Li Z, Long H, Guo R, Xu J, Wang X, Cheng X. Surgical treatment indications and outcomes in patients with spinal metastases in the cervicothoracic junction (CTJ). J Orthop Surg Res. 2018. 13: 1-9
4. Macdelilld JC, Walton DM, Avery S, Blanchard A, Etruw E, Mcalpine C. Measurement properties of the neck disability index: A systematic review. J Orthop Sports Phys Ther. 2009. 39: 400-16
5. Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: Current concepts. Glob Spine J. 2018. 8: 96S
6. Ramani PS, Sharma A, Jituri S, Muzumdar DP. Anterior instrumentation for cervical spine tuberculosis: An analysis of surgical experience with 61 cases. Neurol India. 2005. 53: 83
7. Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. Clin Orthop Relat Res. 1999. 475: 1499-504
8. Shetty AP, Viswanathan VK, Rajasekaran S. Cervical spine TB current concepts in management. J Orthop Surg (Hong Kong). 2021. 29: 230949902110069
9. Tamai K, Buser Z, Paholpak P, Sessumpun K, Nakamura H, Wang JC. Can C7 slope substitute the T1 slope? An analysis using cervical radiographs and kinematic MRIs. Spine (Phila Pa 1976). 2018. 43: 520-5
10. Vernon H, Mior S. The neck disability index: A study of reliability and validity. J Manipulative Physiol Ther. 1991. 14: 409-15
11. Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am. 2007. 18: 365-71
12. Ye IB, Tang R, Cheung ZB, White SJ, Cho SK. Can C7 slope be used as a substitute for T1 slope? A radiographic analysis. Glob Spine J. 2020. 10: 148-52
13. Zhang HQ, Hu X, Yin X, Chen Y. One-stage combined anterior-posterior approach treatment of multiple cervicothoracic spinal tuberculosis with kyphosis. Int Orthop. 2015. 39: 1605-10
14. Zhu Z, Hao D, Wang B, Gao W, Yang R, Guo H. Selection of surgical treatment approaches for cervicothoracic spinal tuberculosis: A 10-year case review. PLoS One. 2018. 13: e0192581