- Department of Spine, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India
- Department of Orthopaedics, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India.
Correspondence Address:
Siddharth Manik Katkade, Department of Spine, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India.
DOI:10.25259/SNI_467_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shailesh Ramakant Hadgaonkar1, Siddharth Manik Katkade1, Pramod Dashrath Bhilare1, Parag Kantilal Sancheti2. Less invasive O-arm navigation-guided excision of thoracic extraosseous intraforaminal osteoblastoma: A case report. 23-Jun-2022;13:263
How to cite this URL: Shailesh Ramakant Hadgaonkar1, Siddharth Manik Katkade1, Pramod Dashrath Bhilare1, Parag Kantilal Sancheti2. Less invasive O-arm navigation-guided excision of thoracic extraosseous intraforaminal osteoblastoma: A case report. 23-Jun-2022;13:263. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11670
Abstract
Background: Gross-total excision of spinal osteoblastomas remains challenging as they are typically found in close proximity to major neural and/or vascular structures. Here, we found that O-arm navigation allowed for safe/effective excision of a spinal osteoblastoma in a 29-year-old male.
Case Description: A 29-year-old male presented neurologically intact with mid back pain of 8 months’ duration and 2 months of the left-sided chest wall discomfort. X-rays showed a sclerotic left D12 pedicle, while the MRI revealed an extradural lesion in extending into the left D11-12 neural foramen (i.e., hypointense on both T1- and T2-weighted images). The CT scan suggested a “floating” foraminal radiolucent lesion with surrounding vertebral body/posterior elements sclerosis and dense peripheral rim enhancement. These findings were diagnostic for an osteoblastoma. Utilizing O-arm navigation, the nidus and full extent of the lesion were excised (i.e., utilizing intralesional curettage). Two year’s postoperatively, there was no MR evidence of tumor recurrence.
Conclusion: O-arm navigation provided accurate intraoperative localization to safely and fully excise a left D11– D12 spinal osteoblastoma.
Keywords: Accuracy, O-arm navigation, Safety, Spinal osteoblastoma, Various operative modalities
INTRODUCTION
About 40% of all osteoblastomas are found in the spine. They mostly involve the posterior spinal elements and occur in, in descending order, the cervical, lumbar, and thoracic regions.[
CASE DESCRIPTION
A 29-year-old male presented with 8 months of mid back pain and 2 months of the left-sided chest wall discomfort with VAS 8/10. His examination revealed diffuse mid back tenderness but no neurological deficit. X-rays showed a mixed sclerotic/lytic lesion involving the left D12 pedicle and superior articular process [
Figure 1:
X-ray and MRI images; (a) AP view showing sclerosis of the left D12 pedicle, (b) lateral view showing radiolucent shadow in D12 superior articular process along, (c) sagittal T1WI showing hypointense lesion surrounded by isointense shadow, (d) sagittal T2WI showing hypointense shadow obliterating foramen, and (e) axial T1WI and (f): axial T2WI showing involvement of pedicle and part of endplate (white arrows).
Surgery
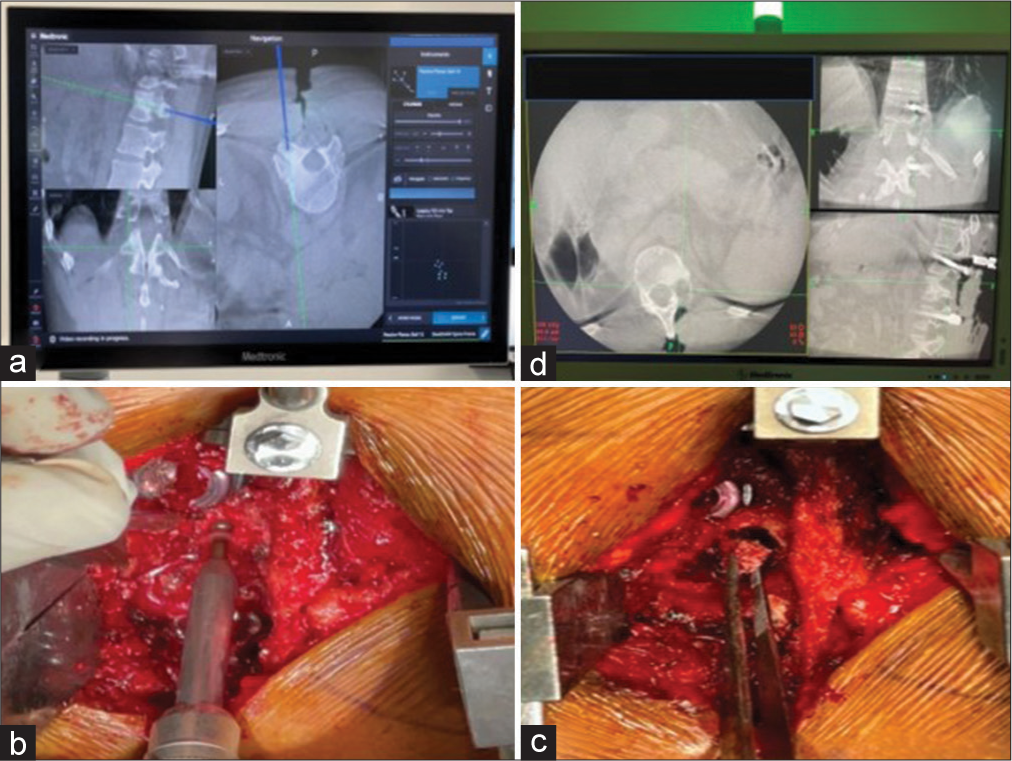
Using O-arm navigation, the tumor was entirely excised (i.e., including the tumor nidus and intralesional curettage) and followed by a standard posterior midline pedicle/ screw/rod instrumented fusion from D11 to L1 level [
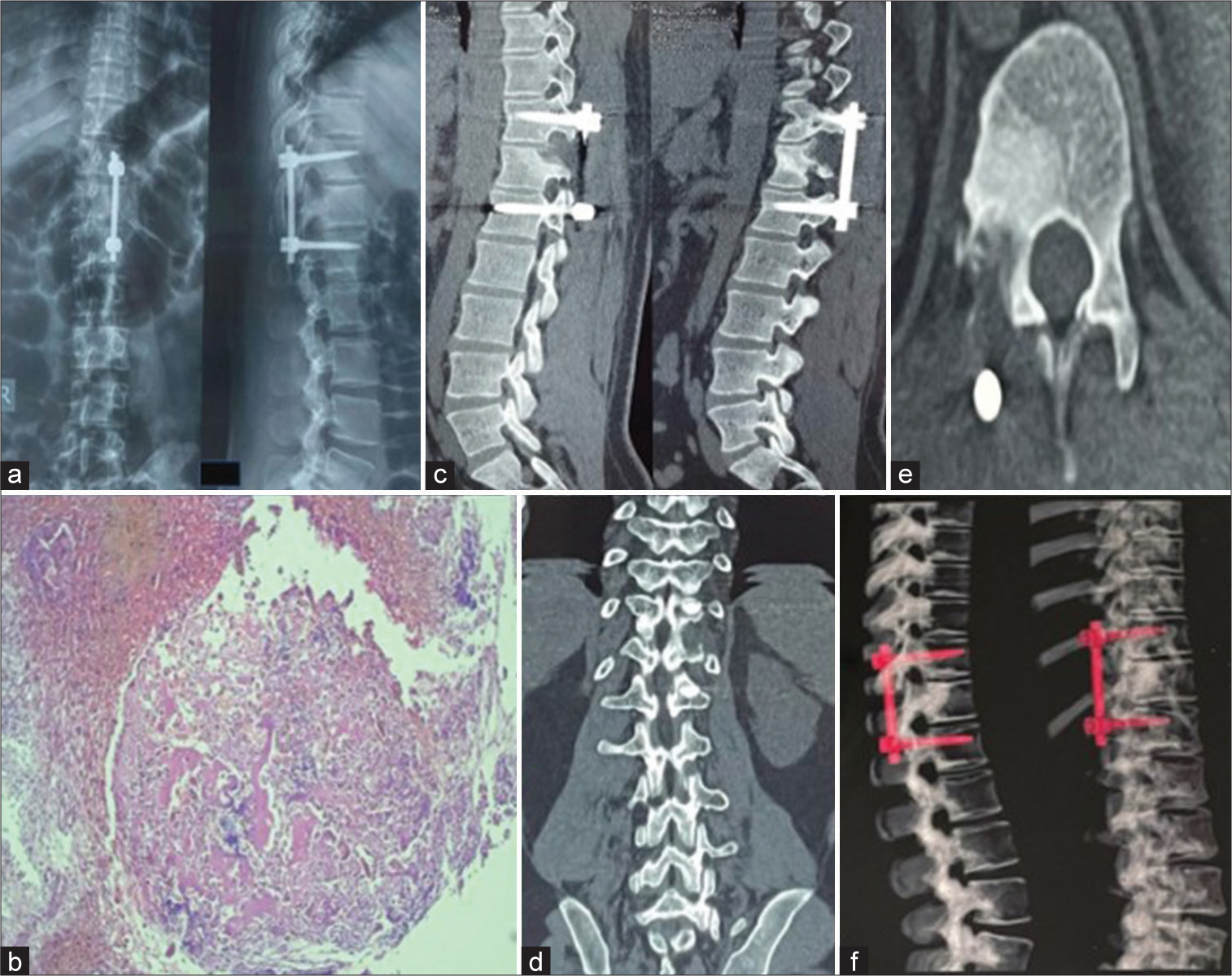
Figure 4:
(a) Postoperative X-ray showing absent nidus and proper implantation, (b) histopathological slide showing a neoplasm composed of interanastomosing trabeculae of woven bone lined by a single layer of osteoblast set within loose edematous fibrovascular stroma with no evidence of increase mitosis or necrosis consistent with osteoblastoma, and (c-f) 2 years postoperative CT images showing no signs of recurrence.
DISCUSSION
Frequency and location of osteoblastomas
Osteoblastomas constitute 1% of all bone tumors, with 40% localized to the spine. They are typically located in posterior elements, in descending order, of the cervical, lumbar, thoracic spine, and only rarely the sacrococcygeal levels. About 80% of osteoblastomas occur in patients under 30 years of age and are predominantly found in males (i.e., male-to-female ratio of 2.5:1). The pain associated with osteoblastomas is somewhat less robust with NSAIDS/aspirin versus osteoid osteomas (i.e., defined as < 1.0 cm).[
Two presentations: Conventional versus aggressive
There are two types of osteoblastomas; conventional and aggressive.[
Surgical recommendations for osteoblastomas
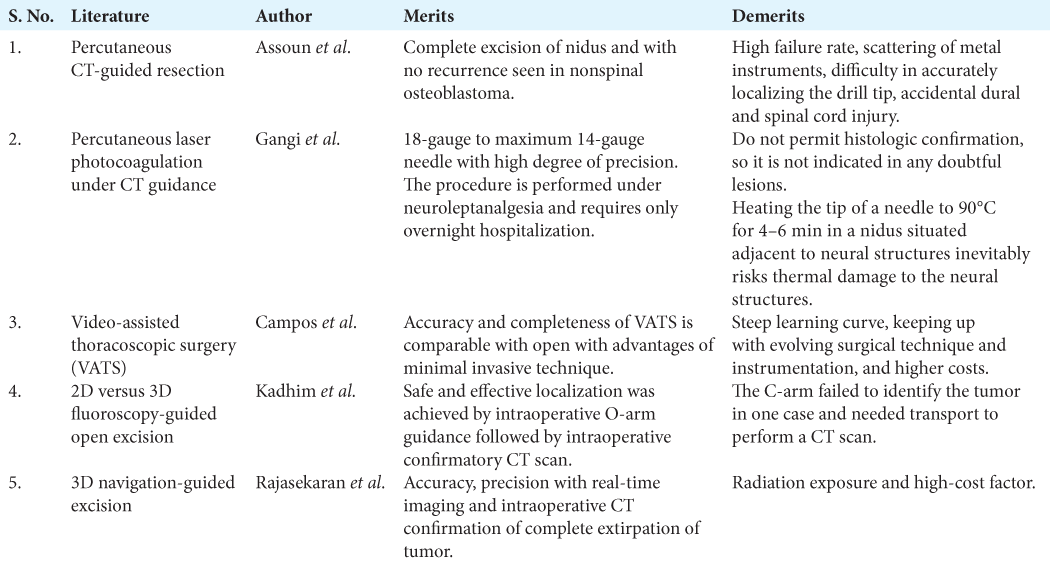
The total excision of osteoblastomas is recommended as they have a 50% recurrent rate with partial/subtotal excision.[
Rajasekaran et al. used of fluoroscopy-based computer navigation in four cases of osteoid osteoma.[
Campos et al. used O-arm navigation in video-assisted thoracoscopic surgery for resection of osteoid osteoma in dorsal vertebra.[
CONCLUSION
O-arm navigation aids accurate location of spinal osteoblastoma and helps to target the nidus resulting in it’s safe and complete excision with intraoperative confirmatory CT scan avoiding neural damage, minimizing dissection, bone removal, and blood loss resulting in faster recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Assoun J, Railhac JJ, Bonnevialle P, Poey C, de Gauzy JS, Baunin C. Osteoid osteoma: Percutaneous resection with CT guidance. Radiology. 1993. 188: 541-7
2. Campos WK, Gasbarrini A, Boriani S. Case report: Curetting osteoid osteoma of the spine using combined video-assisted thoracoscopic surgery and navigation. Clin Orthop Relat Res. 2013. 471: 680-5
3. Gangi A, Dietemann JL, Guth S, Vinclair L, Sibilia J, Mortazavi R. Percutaneous laser photocoagulation of spinal osteoid osteomas under CT guidance. AJNR Am J Neuroradiol. 1998. 19: 1955-8
4. Kadhim M, Binitie O, O’Toole P, Grigoriou E, De Mattos CB, Dormans JP. Surgical resection of osteoid osteoma and osteoblastoma of the spine. J Pediatr Orthop B. 2017. 26: 362-9
5. Limaiem F, Byerly DW, Singh R.editors. Osteoblastoma. Treasure Island, FL: Stat Pearls Publishing; 2022. p.
6. Mori K, Neo M, Takemoto M, Nishizawa K, Imai S. Navigated pin-point approach to osteoid osteoma adjacent to the facet joint of spine. Asian Spine J. 2016. 10: 158-63
7. Rajasekaran S, Kamath V, Shetty AP. Intraoperative Iso-C three-dimensional navigation in excision of spinal osteoid osteomas. Spine (Phila Pa 1976). 2008. 33: E25-9
8. Su AW, Luo TD, McIntosh AL, Schueler BA, Winkler JA, Stans AA. Switching to a pediatric dose O-arm protocol in spine surgery significantly reduced patient radiation exposure. J Pediatr Orthop. 2016. 36: 621-6
9. Wioland M, Sergent-Alaoui A. Didactic review of 175 radionuclide-guided excisions of osteoid osteomas. Eur J Nucl Med. 1996. 23: 1003-11
10. Yin H, Zhou W, Yu H, Li B, Zhang D, Wu Z. Clinical characteristics and treatment options for two types of osteoblastoma in the mobile spine: A retrospective study of 32 cases and outcomes. Eur Spine J. 2014. 23: 411-6