- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, United States
- Department of Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin, United States.
Correspondence Address:
Mokshal H. Porwal, Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, United States.
DOI:10.25259/SNI_454_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mokshal H. Porwal1, Christina N. Feller1, Devesh Kumar1, Julie Kolinski2, Grant P. Sinson1. MedCDI: A technology-based documentation and quality improvement initiative in neurosurgery. 23-Jun-2022;13:271
How to cite this URL: Mokshal H. Porwal1, Christina N. Feller1, Devesh Kumar1, Julie Kolinski2, Grant P. Sinson1. MedCDI: A technology-based documentation and quality improvement initiative in neurosurgery. 23-Jun-2022;13:271. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11678
Abstract
Background: Clinical documentation of patient care alters coding accuracy of Medicare Severity Diagnosis-Related Groups (MS-DRGs), expected mortality, and expected length of stay (LOS) which impact quality metrics. We aimed to determine if neurosurgical quality metrics could be improved by facilitating accurate documentation and subsequently developed a mobile application and educational video to target areas of opportunity.
Methods: Vizient software was used to analyze MS-DRGs and expected LOS for sample of patients requiring surgery for spinal pathology, brain tumors, and subarachnoid hemorrhage (SAH) between January 2019 and August 2021. Chart reviews were conducted to discover variables missed by documenting provider and/or coder.
Results: Review of 114 spinal surgeries, 20 brain tumors, and 53 SAH patients revealed at least one additional variable impacting LOS in 43% of spine, 75% of brain tumor, and 92% of SAH patients, with an average of 1 (1.25), 2 (1.75), and 3 (2.89) new variables, respectively. Recalculated expected LOS increased by an average of 0.86 days for spine, 3.08 for brain tumor, and 6.46 for SAH cases.
Conclusion: Efforts to accurately document patient care can improve quality metrics such as expected LOS, mortality, and cost estimates. We determined several missing variables which impact quality metrics, showing opportunity exists in neurosurgical documentation improvement. Subsequently, we developed an educational video and mobile-supported application to specifically target these variables. To the best of our knowledge, this represents the first initiative to utilize the proven powers of mobile phones in health care toward the novel application of specifically improving neurosurgical quality metrics.
Keywords: Brain tumor, Documentation improvement, Mobile application, Quality metrics, Spine, Subarachnoid hemorrhage
INTRODUCTION
Quality metrics are closely tracked within hospital systems due to their effect on revenue, hospital expansion, relative hospital performance, and trust in the health-care team. Clinical documentation of patient care alters the coding accuracy of Medicare Severity Diagnosis-Related Groups (MS-DRGs), expected length of stay (LOS), expected mortality, and expected costs. These factors are used to code quality metrics which can impact physician and medical center profiling, quality reporting, and revenue. Consequently, surgeons face increasing pressure to improve these metrics in their patient population. However, it can be difficult to accurately document all major factors due to poor data accessibility and ease of interpretation by providers and coders, along with requiring effortful behavioral changes by multiple stakeholders.[
Improving hospital-wide quality metrics such as mortality index (the observed to expected mortality ratio) can be greatly impacted by high-acuity departments such as neurosurgery.[
In this initiative, we aimed to determine if neurosurgical quality metrics could be improved by facilitating clinical documentation using toolkits that have multiple modalities of support. Initially, we aimed to retrospectively determine commonly missed variables within documentation. Subsequently, we aimed to develop a toolkit consisting of an educational video along with a mobile application. This technology-based approach provides the benefit of increased engagement, customized interventions, user convenience, and dynamic real-time updates.
MATERALS AND METHODS
Vizient is the largest health-care performance company that tracks data from over 97% of the US academic medical centers and 600 community hospitals. To create a technology-based quality improvement toolkit, we first developed a 2 min video animation to provide an overview of the role of clinical documentation improvement, coding, Vizient, and a demonstration of the proposed mobile application. We provided this animation to providers for input to assess educational value and effectiveness. We then initiated department specific interventions based on provider preferences and needs. First, specific diagnoses were identified that were being treated but not documented in a way that could be captured by coding. For example, cases of “coma” documentation cannot only include the total Glasgow Coma Scale score, rather it requires each subsection score to show accurate severity of illness. The Vizient Clinical Data Base was utilized with permission of Vizient, Inc. (All rights reserved.) to target areas of opportunity, by MS-DRG, for expected LOS. Retrospective chart reviews based on these targets were conducted to identify high-yield variables for providers to focus on, some of which were documented but not delineated as present on admission. MS-DRGs and expected LOS were analyzed from the clinical database for a sample of 114 spine, 20 brain tumors, and 53 subarachnoid hemorrhage (SAH) patients over the span of January 2019 to August 2021. Chart reviews for all procedures were conducted to search for variables missed by the documenting provider or coder that impact LOS. Expected LOS was recalculated for every procedure, accounting for the missed variables discovered during chart review. Of note, variables are groupings of International Classification of Diseases Tenth Revision (ICD-10) codes that based on risk stratification impact quality metrics including expected LOS, mortality, and cost. If any one ICD-10 code within each grouping is identified, the associated variable is assigned to the patient encounter.
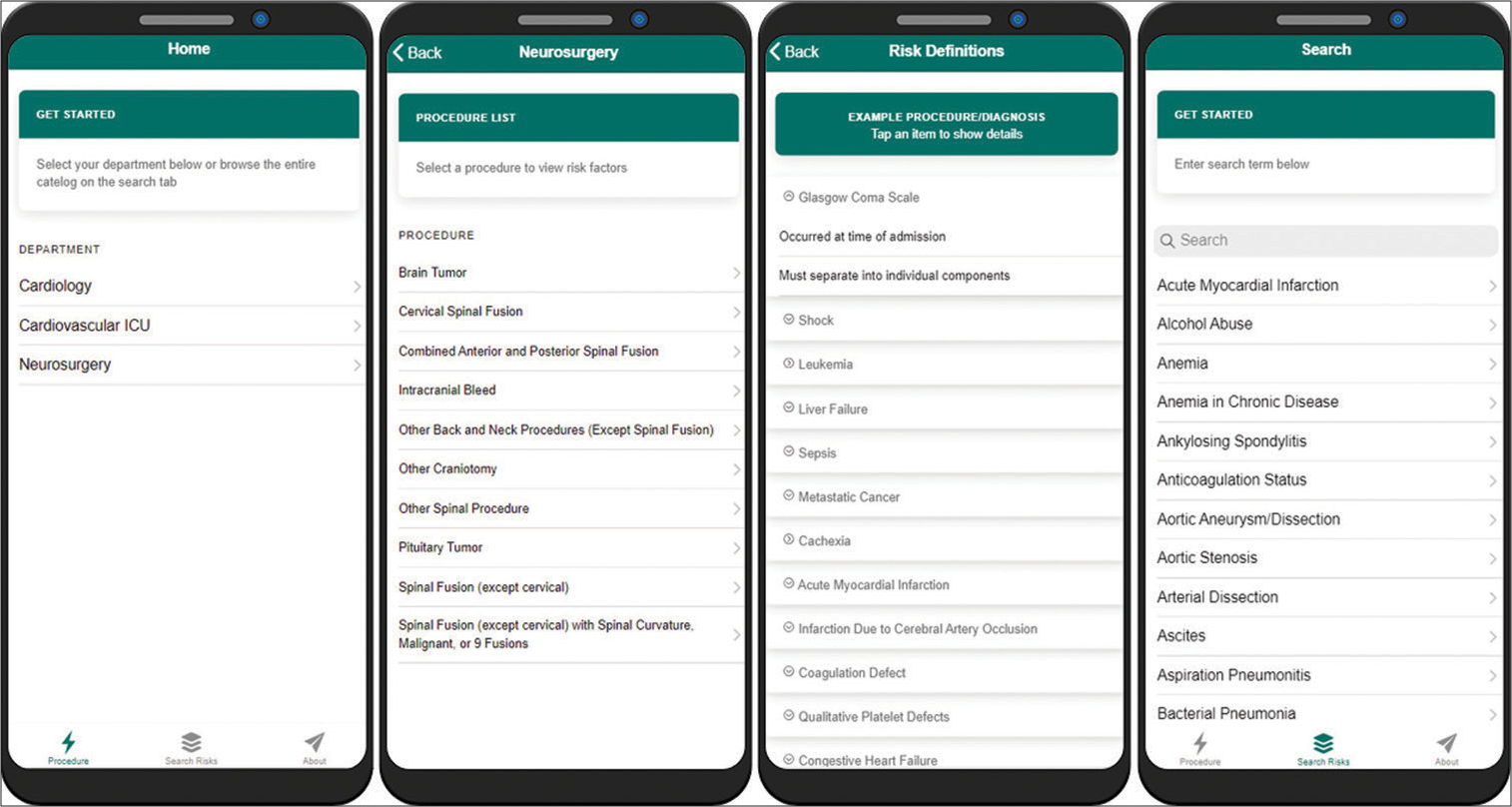
By utilizing department feedback and retrospective clinical data, a Progressive Web Application (PWA) was created with variables divided by procedure and included variable definitions when necessary. A PWA allows seamless access through any device with an internet connection including computers, mobile phones, and tablets. Within this PWA, expandable descriptions for each variable allow the provider to understand what to document for each patient.
Ethics statement
IRB and ethics committee approval were not required for this study since it is classified as nonhuman research for quality improvement. Similarly, patient consent was not required since data collected pertain only to quality metrics assessment without any identifiable patient data or interventions affecting patient care.
RESULTS
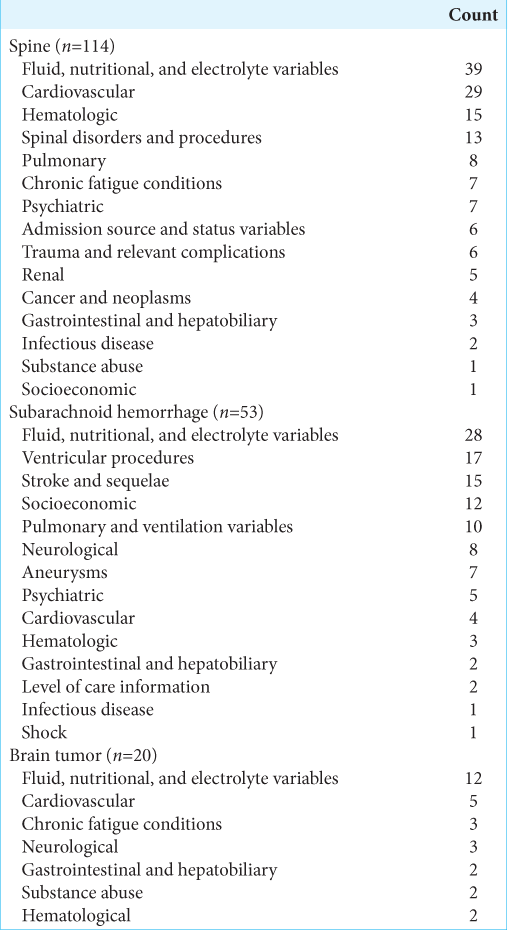
Chart reviews of 114 spinal surgeries, 20 brain tumors, and 53 SAH patients revealed at least one additional variable contributing to expect LOS in 43% of spine, 75% of brain tumor, and 92% of SAH patients. An average of 1 (1.25), 2 (1.75), and 3 (2.89) new variables was found which impact expected LOS in spine, brain tumor, and SAH patients, respectively. Expected LOS, recalculated with previously undocumented variables, increased by an average of 0.86 days for spine cases, 3.08 days for brain tumor cases, and 6.46 days for SAH cases. The greatest increase in expected LOS was 7 days for spine, 32 days for brain tumor, and 72 days for SAH patients when accounting for undocumented risk factors. The most common variable categories missed for each group are shown in
A 2 min educational video animation was created based on department feedback ([
Video 1
Figure 1:
Mobile application to facilitate clinical documentation. Data in this figure are an example and do not represent an exact Vizient risk model. (a) Home page where department can be selected, (b) department page where relevant procedure can be selected, and (c) procedure page showing applicable variables to document. Certain variables can be expanded for further explanation, (d) search page allows user to search for any variable in the application. Clicking the variable opens a descriptive page providing variable explanations.
DISCUSSION
The previous research shows that quality metrics in neurosurgery, such as mortality index, are often not capturing reality and such a problem needs to be addressed.[
Documentation issues
Correct documentation of comorbid conditions (CCs) and major CCs (MCCs) is essential for accurate coding, reimbursement, epidemiological data, and provider/ hospital quality metrics.[
Coding issues
Multiple barriers exist between providers and coders including the value placed on documentation as well as the language used between parties.[
Educational issues
The previous studies report on attempts to improve provider education surrounding coding and clinical documentation through use of an educational handout and group discussion,[
Limitations
This study is limited to the data within the neurosurgical department in one academic center. This application was developed based on retrospective data that show opportunity for improvement exists. However, the next steps require real-world implementation and prospective data on the true impact of such interventions. Generalizability may by limited due to several differences such as hospital structure, types of procedures commonly performed, and individual provider familiarity with the coding process. This further reinforces the need for department-specific interventions; however, the use of technology has a proven positive record in health care. While we provide a preliminary proof-of-concept and inspiration, the future steps are limitless. The possibility for direct integration into the electronic medical record could increase efficiency and adoption. We are working toward implementing this mobile application seamlessly into the daily workflow for the neurosurgery department. Although, this system should not be unique to neurosurgery and can be expanded easily into other departments throughout hospitals once a framework is created.
CONCLUSION
This study identifies several opportunities for documentation accuracy improvement within a single academic neurosurgery department. To the best of our knowledge, this study represents the first initiative to specifically improve neurosurgical quality metrics by utilizing a mobile phone supported application, a modality proven to have profound impacts in health care. Accurate documentation, or lack thereof, influences quality metrics, accurate identification of areas requiring improvement for patient care, and reimbursement. Therefore, it is of vital importance to utilize technological advancements and provide individualized tools and education for the improvement of clinical documentation, especially within acute departments such as neurosurgery. While we retrospectively present that opportunity for improvement in several patient populations exists, the future studies are essential to prospectively determine the real-world impact, mobile phone supported tools can have on documentation improvement. It is our hope that this preliminary proof-of-concept study will inspire other initiatives in neurosurgery to improve quality metrics and patient care by utilizing similar strategies.
Videos available on:
Disclosure
None of the authors have any financial or personal affiliations with Vizient. The database is used to track internal quality metrics and the manuscript was approved for publication by Vizient. There are no conflicts of interest to disclose.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdulla S, Simon N, Woodhams K, Hayman C, Oumar M, Howroyd LR. Improving the quality of clinical coding and payments through student doctor-coder collaboration in a tertiary haematology department. BMJ Open Qual. 2020. 9: e000723
2. Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012. 10: CD004398
3. Grudniewicz A, Kealy R, Rodseth RN, Hamid J, Rudoler D, Straus SE. What is the effectiveness of printed educational materials on primary care physician knowledge, behaviour, and patient outcomes: A systematic review and meta-analyses. Implement Sci. 2015. 10: 164
4. Hakes NA, Kethman WC, Spain D, Nassar AK. Mobile application-based guidelines to enhance patient care and provider education in trauma and acute care surgery. Trauma Surg Acute Care Open. 2020. 5: 479
5. Hammers R, Anzalone S, Sinacore J, Origitano TC. Neurosurgical mortality rates: What variables affect mortality within a single institution and within a national database?. J Neurosurg. 2010. 112: 257-64
6. Hay P, Wilton K, Barker J, Mortley J, Cumerlato M. The importance of clinical documentation improvement for Australian hospitals. Health Inf Manag. 2020. 49: 69-73
7. Horwood CR, Latimer T, Powers CJ, Moffatt-Bruce SD, Rushing GD, Eiferman DS. Improving the mortality index by capturing patient acuity through interprofessional real-time documentation improvement in a single hospital system. Surgery. 2018. 164: 687-93
8. Kessler BA, Catalino MP, Jordan JD. Reducing the reported mortality index within a neurocritical care unit through documentation and coding accuracy. World Neurosurg. 2020. 133: e819-27
9. Kittinger BJ, Matejicka A, Mahabir RC. Surgical precision in clinical documentation connects patient safety, quality of care, and reimbursement. Perspect Health Inf Manag. 2016. 13: 1f
10. Liu W, Walsh T. The impact of implementation of a clinically integrated problem-based neonatal electronic health record on documentation metrics, provider satisfaction, and hospital reimbursement: A quality improvement project. JMIR Med Inform. 2018. 6: e40
11. Rosenbaum BP, Lorenz RR, Luther RB, Knowles-Ward L, Kelly DL, Weil RJ. Improving and measuring inpatient documentation of medical care within the MS-DRG system: Education, monitoring, and normalized case mix index. Perspect Health Inf Manag. 2014. 11: 1c
12. Shepheard J. What do we really want from clinical documentation improvement programs?. Health Inf Manag. 2018. 47: 3-5
13. Swaminath D, Hefner JL, Jenkins LA, Suarez JA, Meyerrose G, Huerta TR. Improving clinical documentation in an academic setting: A multidisciplinary team approach focused on the physician’s perspective. J Healthc Manag. 2018. 63: E88-98
14. Tarantino I, Widmann B, Warschkow R, Weitzendorfer M, Bock S, Roeske S. Impact of precoding on reimbursement in diagnosis-related group systems: Randomized controlled trial. Int J Surg. 2021. 96: 106173
15. Tobert CM, Mott SL, Nepple KG. Malnutrition diagnosis during adult inpatient hospitalizations: Analysis of a multi-institutional collaborative database of academic medical centers. J Acad Nutr Diet. 2018. 118: 125-31
16. Zalatimo O, Ranasinghe M, Harbaugh RE, Iantosca M. Impact of improved documentation on an academic neurosurgical practice. J Neurosurg. 2014. 120: 756-63