- Department of Neurosurgery, University of Baghdad, College of medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Louisville, Louisville, Kentucky, United States,
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, Alfaisal University, College of Medicine, Riyadh, Saudi Arabia,
- Department of Neurosurgery, University of Al-Mustansiriya, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Mansoura, College of Medicine, Mansoura, Egypt,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Hagar A. Algburi, Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq.
DOI:10.25259/SNI_1039_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hagar A. Algburi1, Mayur Sharma2, Mustafa Ismail3, Sadeem A. Albulaihed4, Mustafa R. Al-Gertani5, Sajjad N. Majeed5, Hussein M. Hasan1, Osama S. Idris6, Norberto Andaluz7, Samer S. Hoz7. The coexistence of anterior communicating artery aneurysm and meningioma: A literature review and illustrative case. 02-Dec-2022;13:569
How to cite this URL: Hagar A. Algburi1, Mayur Sharma2, Mustafa Ismail3, Sadeem A. Albulaihed4, Mustafa R. Al-Gertani5, Sajjad N. Majeed5, Hussein M. Hasan1, Osama S. Idris6, Norberto Andaluz7, Samer S. Hoz7. The coexistence of anterior communicating artery aneurysm and meningioma: A literature review and illustrative case. 02-Dec-2022;13:569. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12032
Abstract
Background: Anterior communicating artery (Acom) aneurysm has an association with many types of intracranial lesions. However, its association with meningioma can be challenging, which is not well addressed in the literature. Herein, we described a literature review focused on the association between Acom aneurysm and meningioma, explicitly highlighting the spatial presence between these two pathologies. We analyzed the literature according to that association with particular emphasis on location-based challenges. Furthermore, we present an illustrative case of surgically treating both lesions in one surgery utilizing the same approach.
Methods: A Medline database search was conducted by the following combined formula: (Meningioma [Title/ Abstract]) AND (Aneurysm [Title/Abstract]) AND (((Anterior communicating artery [Title/Abstract]) OR (Acom [Title/Abstract])) OR Acomm [Title/Abstract]))). Additional resources were added after screening the references of the included papers.
Results: Nine patients with coexistence of Acom aneurysm and meningioma were found in the literature. The coexistence of both pathologies was found in seven females and two males. The presence of an aneurysm was found to be solitary in 66.67% (n = 6/9). Furthermore, meningioma was found to be an isolated lesion in all included cases, and in 22.2% (n = 2/9), they were located ipsilaterally. The location of the meningioma to the aneurysm seems to be in proximity.
Conclusion: Acom aneurysm can coexist with intracranial meningioma; this association can be spatially related intracranially. Such coexistence entails a variety of nuances and challenges that neurosurgeons encounter during the management of these complex lesions.
Keywords: Anterior communicating artery aneurysm, Intracranial meningioma, Meningioma
INTRODUCTION
Intracranial aneurysm (ICAn) is a common cerebrovascular disease characterized by abnormal localized dilation of blood vessels that mostly found through the branching points of major cerebral arteries that course through the subarachnoid space. A subarachnoid hemorrhage (SAH) resulting from aneurysmal rupture is a potentially devastating event found in 3–5% of the general population and associated with high morbidity and mortality rates, reaching 50% of cases.[
MARTIALS AND METHODS
We conducted a different Medline database search by the following combined formula: (Meningioma [Title/Abstract]) AND (Aneurysm [Title/Abstract]) AND (((Anterior communicating artery [Title/Abstract]) OR (Acom [Title/ Abstract])) OR Acomm [Title/Abstract]))). A total of 30 results were found. Seventeen articles were included; they included twenty-four cases. Specifically, from these 17 articles, nine articles were found to address Acom aneurysm and meningioma relationship, with a total of nine cases. Furthermore, references cited by the retrieved articles were thoroughly reviewed to search for additional articles. The included cases were analyzed according to these parameters:
Preoperative data: (A) Patient demographics (age, gender). (B) Clinical presentation. (D) Aneurysmal characteristics: multiplicity other than Acom aneurysm, shape, size, the direction of the dome, neck diameter, and dome to neck ratio. (E) Meningioma characteristics: multiplicity, location, types, source, nature, hemorrhagic or not, grade according to the World Health Organization (WHO) grading scale, adhesion to Acom aneurysm present or not. (F) Sides of lesions. Intra-operative data: (G) Treatment of aneurysm: clipping, coiling, observation. (H) Treatment of meningioma: surgical resection, gamma knife or radiotherapy, observation. (I) which one was treated first? Or treated together? Postoperative data: it includes outcome and follow-up.
The location of meningioma was classified as (parasagittal area, followed by the falx, sinus cavernous, tuberculum sellae, lamina cribrosa, foramen magnum, and torcular zones). In contrast, the type of meningioma was classified as (convexity, falcine and parasagittal, intraventricular, cavernous sinus, clival, foramen magnum, olfactory groove, posterior fossa, sphenoid wing, spinal, and suprasellar, tentorial). Furthermore, Meningioma was classified according to the WHO into Grade I (benign slowly growing), Grade II (atypical or mid-grade tumors), and Grade III (malignant rapidly growing).[
RESULTS
Patients’ characteristics
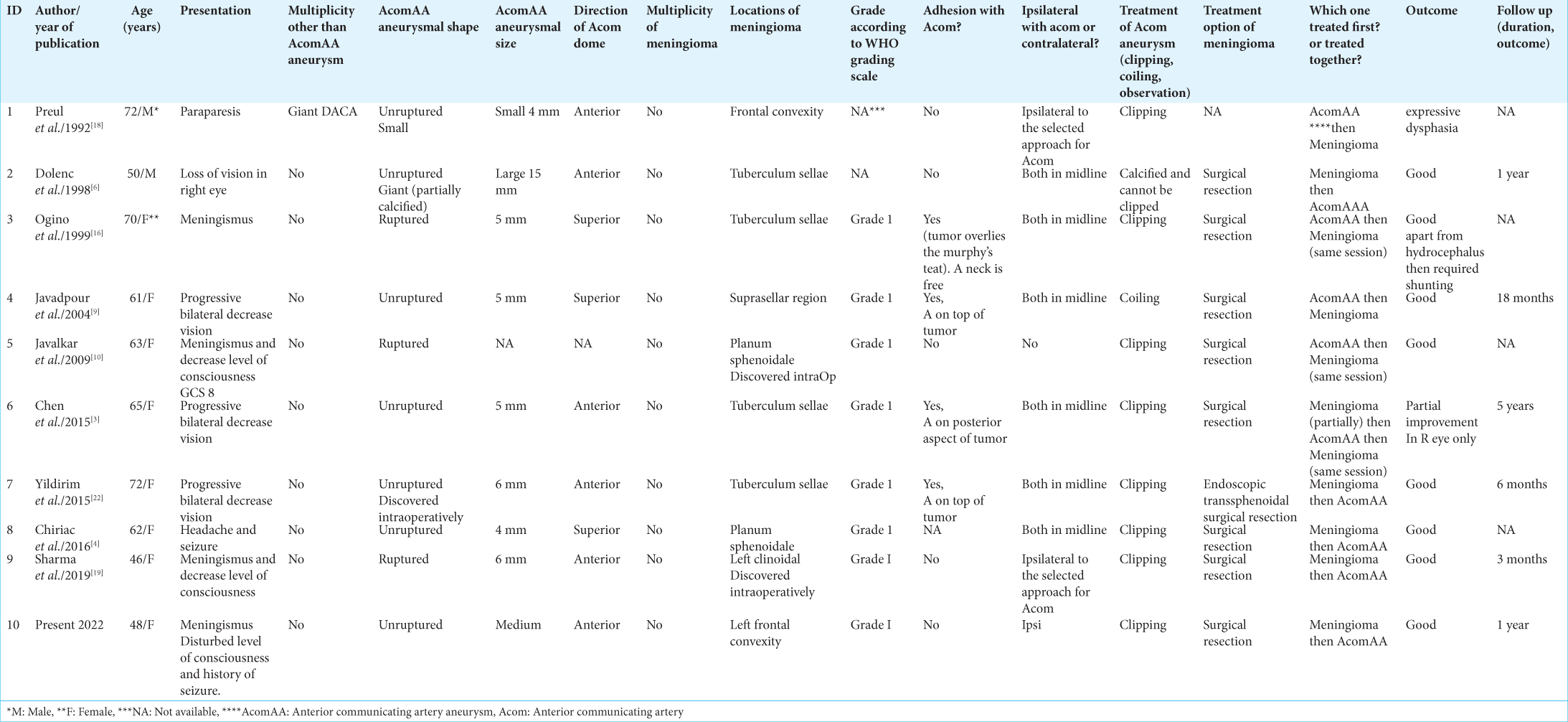
An analysis of published data from 1992 to 2019 showed coexistence of Acom aneurysms and meningiomas in nine cases. Analyzing the available data, we found the coexistence of aneurysm and meningioma in seven females and two males (ratio 7:2). Range of patients’ age was (46–72 years) with a mean of 62.2 years. Data for the all available cases are presented in
Aneurysm and tumors characteristics
The Acom aneurysm was found to be isolated in (n = 6/9) (67%) cases, and one case included a multiple Acom aneurysm. Moreover, the aneurysmal size ranged between 4 and 15 mm in (n = 8/9) (89%) cases. The status of the aneurysm was unruptured in (n = 6/9) (67%) cases, while in the remaining three cases, it was found to be ruptured. Another aneurysmal characteristic, like the direction of the dome, was mentioned in (n = 5/9) (56%) cases, which was anteriorly directed, and the neck-to-dome ratio was mentioned in one case, which was 2.5 mm. Further, meningioma was found to be isolated in 9 cases. Regarding the location, meningioma was located in tuberculum sellae in (n = 4/9) (44%), planum sphenoidale (n = 2/9) (22%), frontal convexity (n = 1/9) (11%), left clinoid process (n = 19) (11%), and suprasellar region (n = 19) (11%).
Regarding the grade of meningioma (according to the WHO grading scale), Grade 1 was documented in (n = 7/9) (78%) cases. Out of nine cases, aneurysm and meningioma were found to be located in the midline in 67% (n = 6/9) of patients and ipsilaterally in 22% (n = 2/9) of patients.
Clinical data
The cases presented in
Treatment
The majority of aneurysms were treated by clipping (n = 7/9) (78%), whereas coiling was found in one case; observation of the patients with aneurysms was noted in one case. Meningioma was treated by surgical resection in (n = 8/9) (89%) patients, which represents the most common type of treatment, and it was not mentioned in 1 case. In (n = 3/9) (33%) cases, the meningioma was treated first, followed by the aneurysm. However, the aneurysm and meningioma were treated together in (n = 3/9) (33%) cases. In one case, the aneurysm was managed first; a week later, the meningioma was resected. Furthermore, in one case, the aneurysm was treated first, and in another one, the meningioma was treated first.
Outcome and follow-up
The postoperative outcome was reported as good (no neurological deficit) in six out of nine cases, while the other three patients had postoperative complications. One patient had hydrocephalus requiring CSF diversion procedure. In terms of tumor outcomes, follow-up of 4 cases was reported as good; 5 years follow-up showed tumor recurrence in one case, while the remaining cases were not reported.
Case description
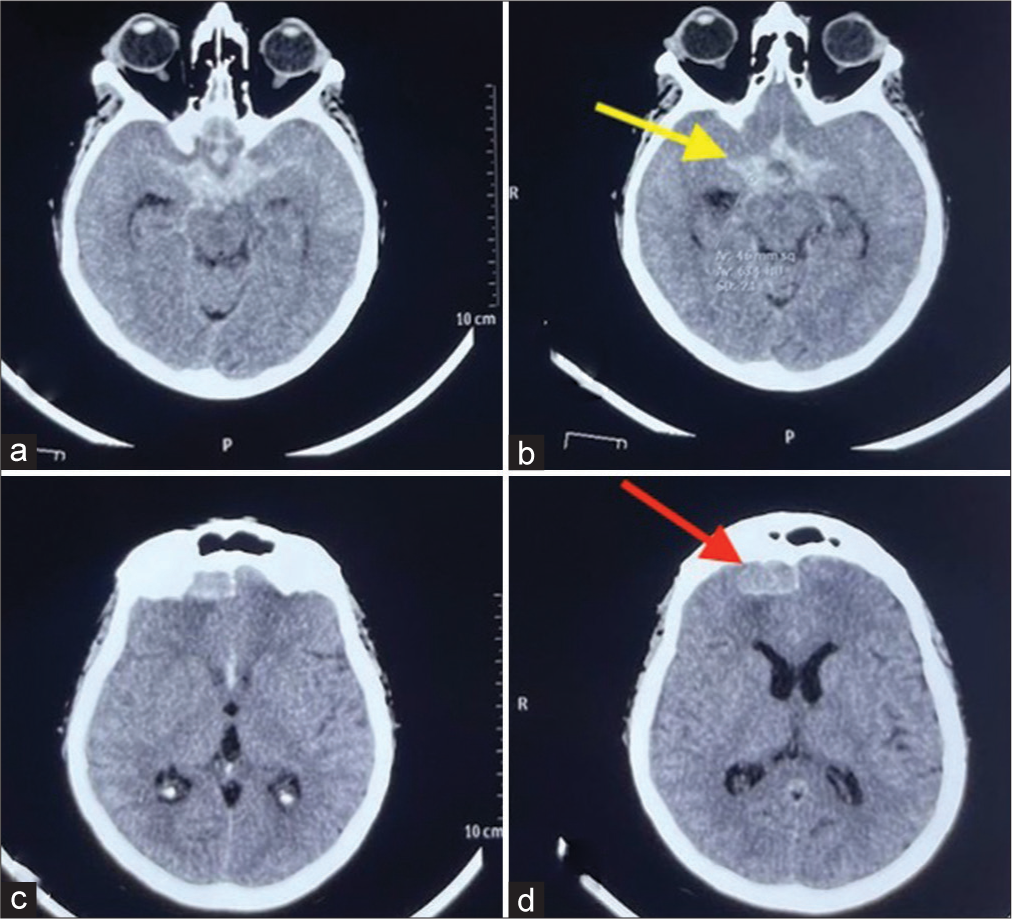
Forty-eight-year-old female was admitted to the Neurosurgery Teaching Hospital, Baghdad, Iraq, with a sudden onset of loss of consciousness. She had a history of recurrent seizures. Her initial Glasgow Coma Scale was13/15 (E3, V5, M5); there was no weakness. A head CT scan revealed diffuse SAH suspected to be related Acom aneurysm rupture [
DISCUSSION
The association between ICAn and brain tumors is rare but not a new phenomenon.[
In comparison, symptoms from the aneurysm, especially if it is ruptured, are estimated in 17–45% of all cases, and symptoms of both lesions were recorded in 6% of cases.[
Several articles in the literature attempted to explain this correlation using various hypotheses such as local hemodynamic, hormonal, and genetic factors and direct invasion of tumor cells to the vessel wall (considered a primary reason for this clinical coexistence).[
Based on the results of the reviewed literature and our case, seven out of all nine cases were female, which is interesting and points toward the hormonal theory. The presence of Acom aneurysms and meningiomas in most patients was found to be ipsilateral within the same hemisphere. The occurrence of both pathologies in different hemispheres seems purely accidental. The presence of meningioma associated with aneurysms was found to be isolated in most cases. Furthermore, the presence of an aneurysm was found to be solitary in most patients. In terms of management, most patients noted surgical clipping of the aneurysm and resection of the tumor during the same setting. Similar to the first case by Preul et al. in 1992, we encountered a calcified meningioma in our patient, which was not planned to be resected. However, while considering the supraorbital approach, we decided to resect the tumor in the same setting.[
Moreover, when an intracranial tumor is closely related to the major intracranial vessel, preoperative magnetic resonance imaging angiography can be considered for the early diagnosis of a possible coexisting aneurysm and for reducing the risk of intraoperative aneurysm rupture.
CONCLUSION
Acom aneurysm can coexist with intracranial meningioma; this association can be spatially related intracranially. Such coexistence entails a variety of nuances and challenges that neurosurgeons encounter during the management of these complex lesions.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Arieti S. Multiple meningioma and meningiomas associated with other brain tumors. J Neuropathol Exp Neurol. 1944. 3: 255-70
2. Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006. 355: 928-39
3. Chen JL, Lee JS, Su ED, Chuang MT, Chen HH. Coexistence of anterior communicating artery aneurysm and tuberculum sellae meningioma. Form J Surg. 2015. 48: 226-9
4. Chiriac A, Ion G, Faiyad Z, Poeata I. Associated intracranial lesions: Meningioma and anterior communicating aneurysm. Roman Neurosurg. 2016. 30: 356-9
5. Delfini R, Domenicucci M, Ferrari M. Association of intracranial meningiomas and aneurysms. Report of three cases and review of the literature. J Neurosurg Sci. 1990. 34: 51-6
6. Dolenc VV, Pregelj R, Slokan S, Skrbec M. Anterior communicating artery aneurysm associated with tuberculum sellae meningioma-case report. Neurol Med Chir (Tokyo). 1998. 38: 485-8
7. Elnahry AG, Elnahry GA. Oculomotor nerve palsy associated with duplication of middle cerebral artery, anterior communicating artery aneurysm, and parietal meningioma. NeuroOphthalmology. 2019. 43: 53-5
8. Hop JW, Rinkel GJ, Algra A, Van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage: A systematic review. Stroke. 1997. 28: 660-4
9. Javadpour M, Khan AD, Jenkinson MD, Foy PM, Nahser HC. Cerebral aneurysm associated with an intracranial tumour: Staged endovascular and surgical treatment in two cases. Br J Neurosurg. 2004. 18: 280-4
10. Javalkar V, Guthikonda B, Vannemreddy P, Nanda A. Association of meningioma and intracranial aneurysm: Report of five cases and review of literature. Neurol India. 2009. 57: 772-6
11. Kim YH, Lee YJ, Han JH, Ahn S, Lee J, Kim JH. Association of intracranial aneurysms and meningiomas: A case-control study. J Neurosurg. 2015. 123: 357-61
12. Kodama T, Matsukado Y, Takamoto K. Acoustic schwannoma presenting as subarachnoid hemorrhage due to ruptured contact aneurysm. Surg Neurol. 1987. 27: 77-80
13. Korhonen K, Salminen T, Raitanen J, Auvinen A, Isola J, Haapasalo H. Female predominance in meningiomas can not be explained by differences in progesterone, estrogen, or androgen receptor expression. J Neurooncol. 2006. 80: 1-7
14. Mira JM, Costa FA, Horta BL, Fabião OM. Risk of rupture in unruptured anterior communicating artery aneurysms: Meta-analysis of natural history studies. Surg Neurol. 2006. 66: S12-9
15. Nugraha N, Wiyasa IW, Wardhana DW, Vierlia WV, Mustofa E. Case report: Hyperprolactinemia in suprasellar meningioma. Asian J Health Res. 2022. 1: 52-6
16. Ogino M, Nakatsukasa M, Nakagawa T, Murase I. Ruptured anterior communicating artery aneurysm encased in a tuberculum sellae meningioma: Case report. J Neurosurg. 1999. 91: 871-4
17. Pia HW, Obrador S, Martin JG. Association of brain tumours and arterial intracranial aneurysms. Acta Neurochir (Wien). 1972. 27: 189-204
18. Preul M, Tampieri D, Leblanc R. Giant aneurysm of the distal anterior cerebral artery: Associated with an anterior communicating artery aneurysm and a dural arteriovenous fistula. Surg Neurol. 1992. 38: 347-52
19. Sharma RK, Jha R, Bista P. Clinoidal meningioma associated with an anterior communicating artery aneurysm: Case report. Nepal J Neurosci. 2019. 16: 50-3
20. Spitler K, Drazin D, Hanna G, Patel A, Chu R. Association of intracranial aneurysms with meningiomas, pituitary adenomas, and gliomas: Review of possible interrelationships. ISRN Neurol. 2013. 2013: 383425
21. Suslu HT, Bozbuga M. Primary brain tumors associated with cerebral aneurysm: Report of three cases. Turk Neurosurg. 2011. 21: 216-21
22. Yildirim AE, Divanlioglu D, Karaoglu D, Cetinalp NE, Belen AD. Pure endoscopic endonasal clipping of an incidental anterior communicating artery aneurysm. J Craniofac Surg. 2015. 26: 1378-81
23. Zhong Z, Sun Y, Lin D, Sun Q, Bian L. Surgical treatment of brain tumor coexisted with intracranial aneurysm-case series and review of the literature. Neurosurg Rev. 2013. 36: 645-56