- Department of Neurosurgery, NTT Medical Center Tokyo, Shinagawa City, Tokyo, Japan.
Correspondence Address:
Masafumi Segawa, Department of Neurosurgery, NTT Medical Center Tokyo, Shinagawa City, Tokyo, Japan.
DOI:10.25259/SNI_1024_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masafumi Segawa, Tomohiro Inoue, Sho Tsunoda, Ryuichi Noda, Atsuya Akabane. Anterior transpetrosal approach for microvascular decompression associated with the dolichoectatic vertebrobasilar artery in two patients with refractory trigeminal neuralgia: Technical note. 09-Dec-2022;13:576
How to cite this URL: Masafumi Segawa, Tomohiro Inoue, Sho Tsunoda, Ryuichi Noda, Atsuya Akabane. Anterior transpetrosal approach for microvascular decompression associated with the dolichoectatic vertebrobasilar artery in two patients with refractory trigeminal neuralgia: Technical note. 09-Dec-2022;13:576. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12055
Abstract
Background: Trigeminal neuralgia (TN) due to compression from the dolichoectatic vertebrobasilar artery (DVBA) is extremely rare and difficult to treat due to its morphological characteristics. We report two cases of good transposition of DVBA and postoperative course obtained using the anterior petrosal approach and a new vasoculopexy method.
Methods: We describe two cases of microvascular decompression (MVD) for refractory TN associated with DVBA. In both cases, MVD was performed through the anterior petrosal approach. The DVBA was decompressed using a GORE-TEX sling and WECK clip in an inferomedial direction.
Results: Complete pain relief without new neurological deterioration was achieved immediately in both patients.
Conclusion: We experienced a rare condition of TN due to exclusion by the DVBA. The anterior transpetrosal approach was extremely effective in this case. This approach secured the surgical field, allowed transposition of the DVBA, and caused no perioperative complications.
Keywords: Anterior petrosal approach, Dolichoectatic vertebrobasilar artery, Microvascular decompression, Retrosigmoid approach, Trigeminal neuralgia
INTRODUCTION
Jannetta first reported trigeminal neuralgia (TN) due to vascular compression in 1967.[
Video 1
CASE REPORT
Case 1
History and examination
A 65-year-old man presented with refractory TN (BNI pain intensity scale IV) in the left V2–3 area.
Imaging studies
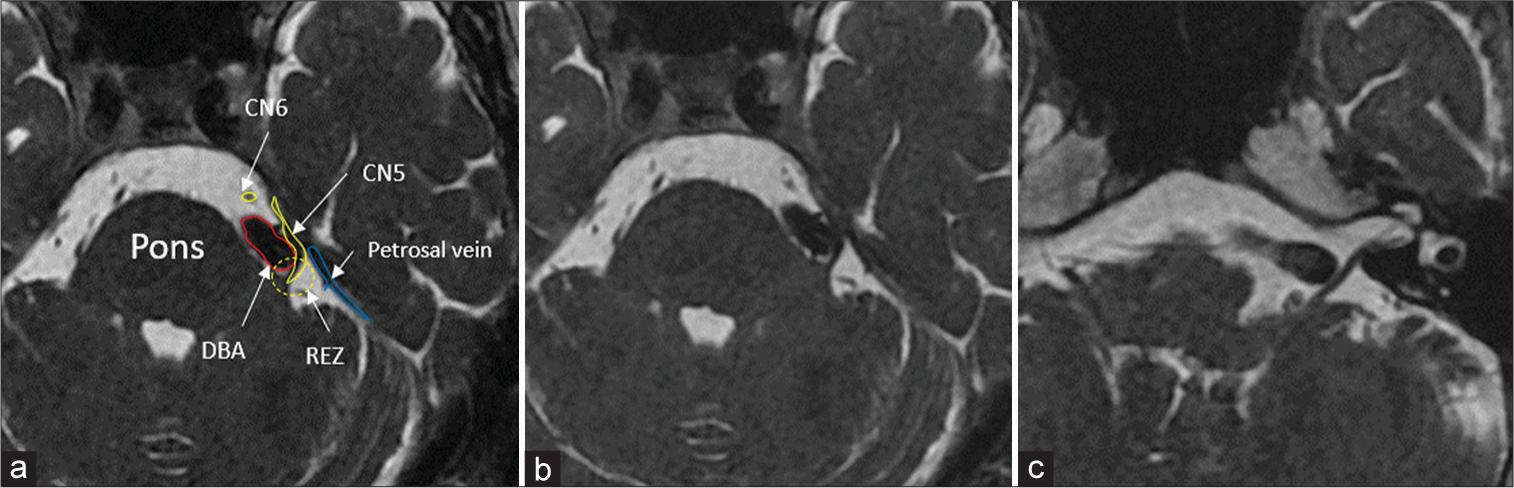
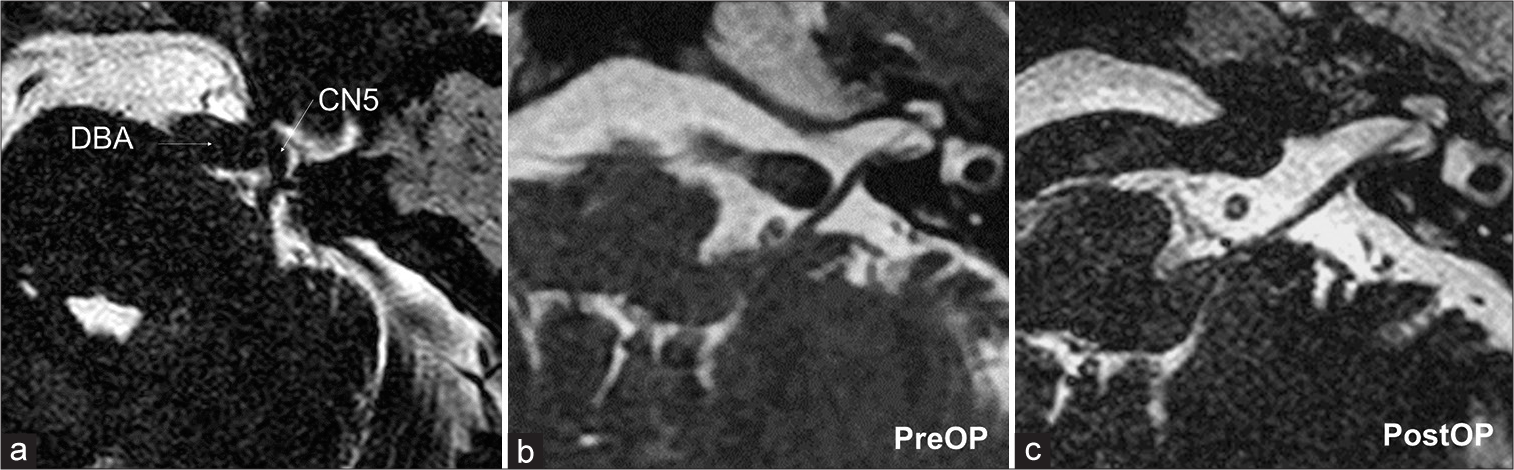
Magnetic resonance imaging (MRI) showed the DVBA with compression of the left trigeminal nerve (CN5) [
Figure 1:
(a and b) DBA compressing the left CN5 on preoperative magnetic resonance imaging (MRI) FIESTA (fast imaging employing steady-state acquisition). (c) DBA also compress the left facial and cochlea nerves. CN5, trigeminal nerve; CN6, abducens nerve (yellow line); DBA, dolichoectatic basilar artery; petrosal vein (blue line); REZ, root exit zone (yellow dotted line).
Surgical report
The retrosigmoid approach is typical for MVD. However, considering the difficulty of securing the surgical field and the transport direction, we chose the anterior petrosal approach.
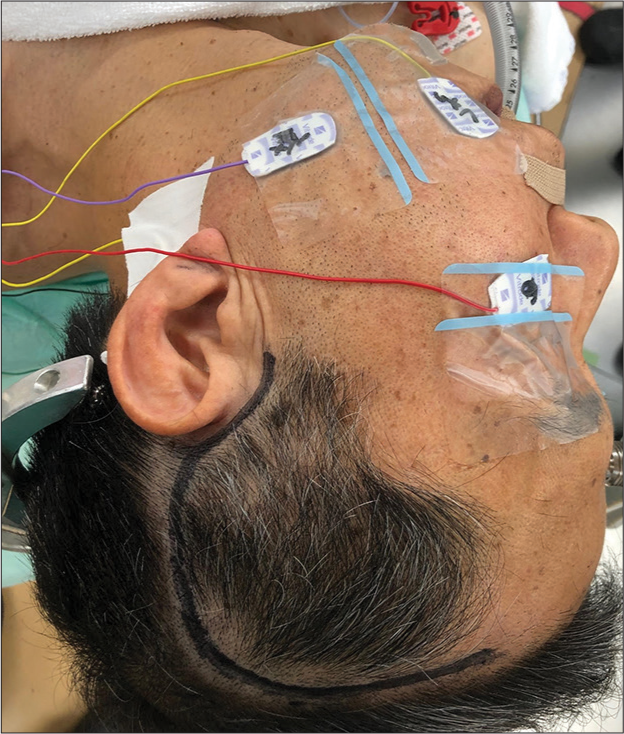
Auditory brainstem responses (ABR) and facial nerve monitoring were placed while the patient was under general anesthesia [
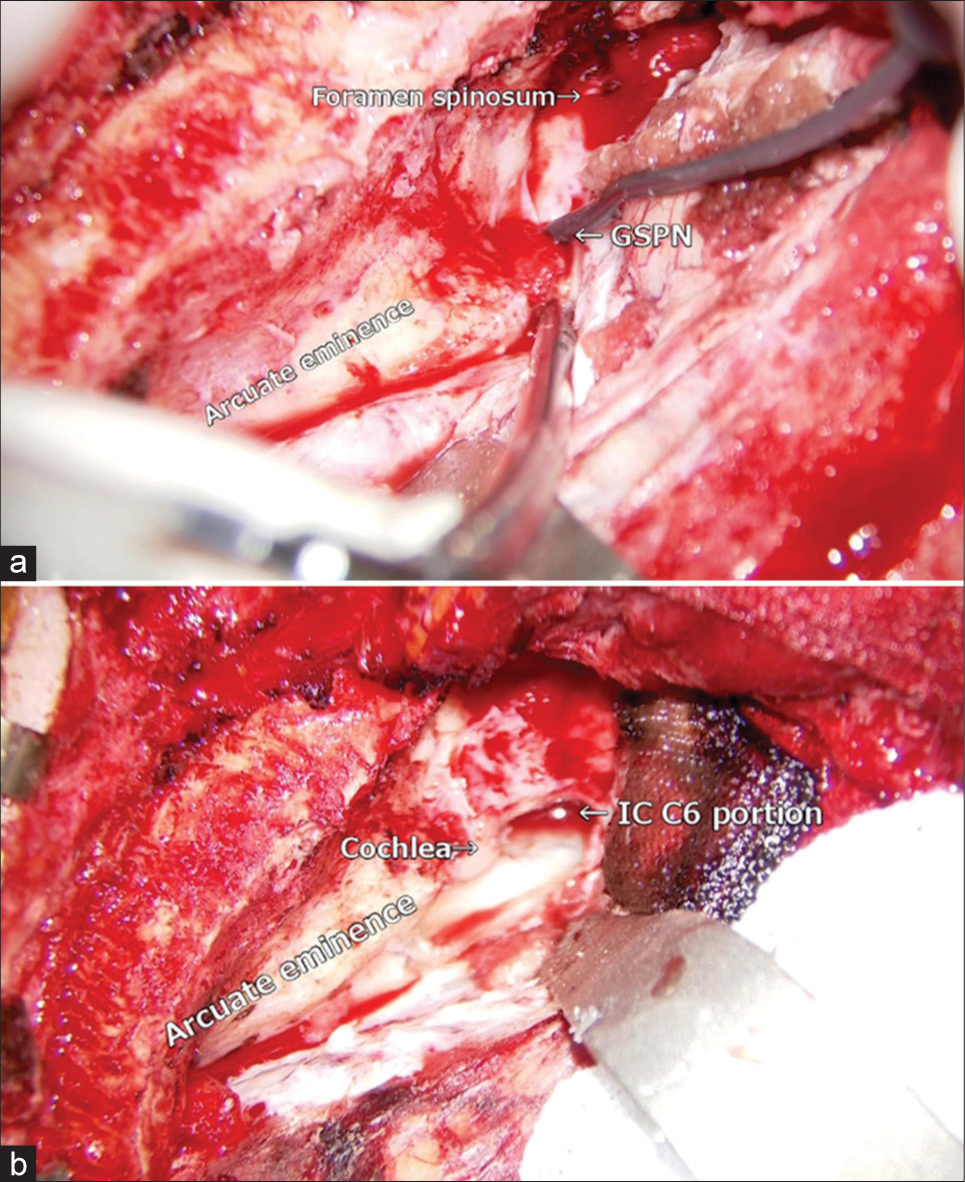
Figure 3:
(a) The dura mater was elevated interdurally, leaving the GSPN on the middle base, up to the point where the GSPN submerges inside the foramen ovale. (b) The drilling proceeded inferiorly up to the depth of the internal carotid artery on the deep anterior border. GSPN: Greater superficial petrosal nerve.
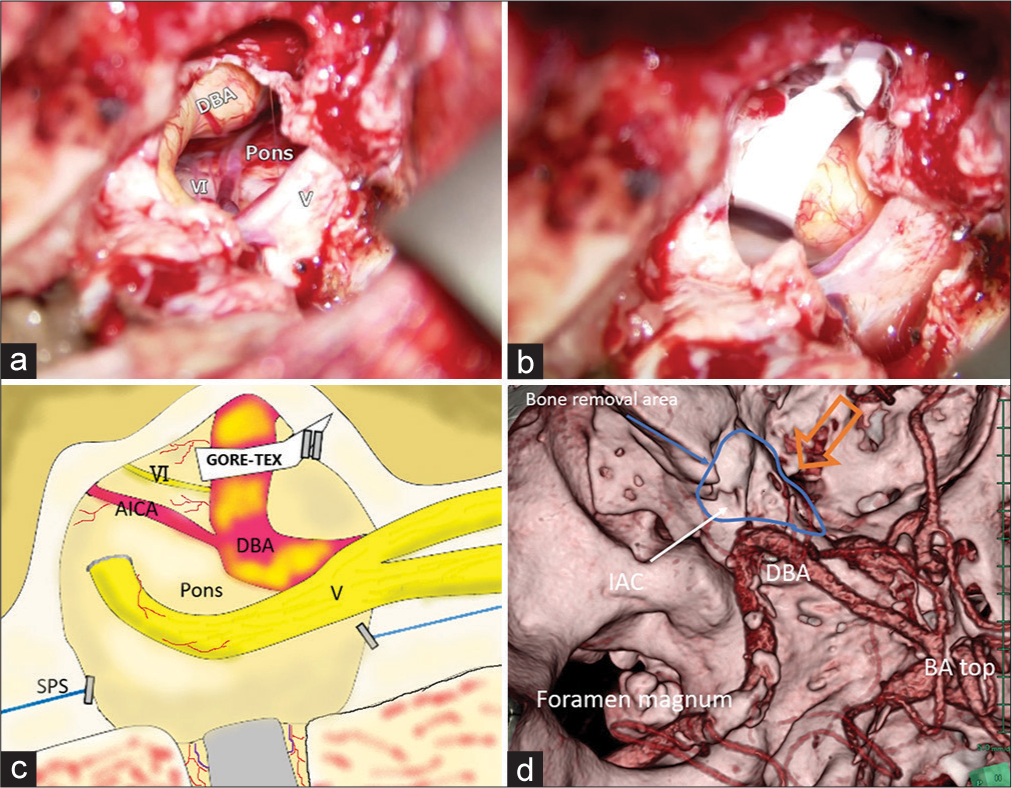
The anterior superior wall of the internal auditory canal was opened and the tip of the petrous bone was removed up to the height of the inferior petrosal sinus. The dura mater of the middle fossa and posterior fossa was incised perpendicular to the superior petrosal sinus (SPS). The SPS was cauterized and divided anterior to the petrous vein, and the cerebellar tentorium was cut toward the free edge of the tentorium. The stretched trigeminal nerve, pons, yellowish DVBA, and anterior inferior cerebellar artery (AICA) were confirmed [
Figure 4:
(a) The stretched trigeminal nerve, pons, yellowish DVBA, AICA were confirmed. (b) The GORE-TEX slip was immobilized on the dura mater of the clivus with a WECK clip. (c) Intraoperative anatomical schema. SPS (d) Postoperative computed tomography angiography 3D construction. Bone removal area (blue area) and DVBA. BA top: Top of the basilar artery, IAC: Internal auditory canal; Operative projection (orange arrow), SPS: Superior petrosal sinus, DVBA: Dolichoectatic basilar artery, AICA: Anterior inferior cerebellar artery.
Follow-up
Postoperative computed tomography angiography confirmed the appropriate range of bone removal and the positional relationship with the DVBA [
Figure 5:
(a) Exclusion of the DVBA to CN5 was released on the postoperative magnetic resonance imaging FIESTA. Changes between (b) preoperative (PreOp) and (c) postoperative (PostOp) in DVBA running at the level of the internal auditory meatus. DVBA: Dolichoectatic basilar artery, CN5: Trigeminal nerve, FIESTA: Fast imaging employing steady-state acquisition.
Case 2
History and examination
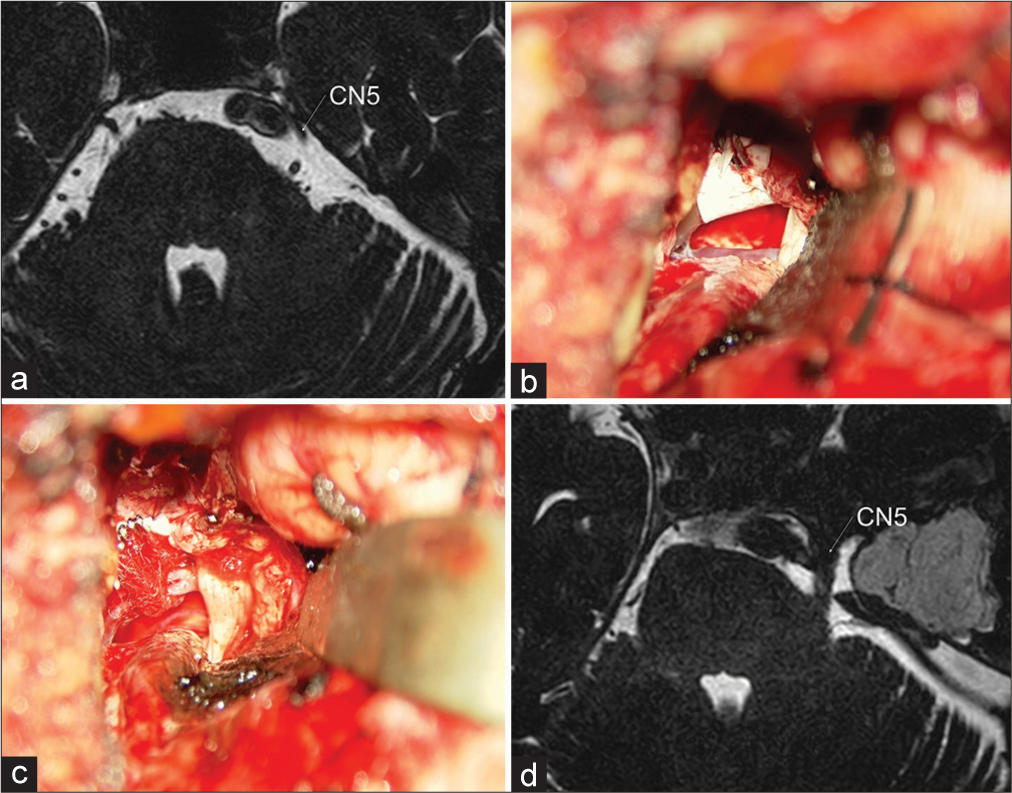
A 52-year-old man presented with refractory TN (BNI pain intensity scale: IV) in the left V2–3 area. Oral treatment was ineffective and the patient visited our hospital with an interest of undergoing surgery. The MRI scan revealed the DVBA and left AICA, with compression of the left CN5 in the posterolateral direction [
Figure 6:
(a) Preoperative MRI FIESTA shows DVBA compressing the left CN5. (b) The DVBA was immobilized with GORE-TEX sling. (c) Left AICA was transpositioned with Teflon sling, and the Meckel’s cave was opened to redirect the CN5. (d) The postoperative MRI scan confirmed the release of the nerve’s compression and the straightening of the CN5. DVBA: Dolichoectatic basilar artery, FIESTA: Fast imaging employing steady-state acquisition, AICA: Anterior inferior cerebellar artery, CN5: Trigeminal nerve.
DISCUSSION
TN due to vascular neuropathy is a painful disorder with an annual incidence of five in 100,000 people.[
The retrosigmoid or far-lateral approach has been adopted in most MVD cases associated with the DVBA. This manipulation must be performed in a narrow corridor while paying attention to the facial and cochlea nerves (CN8). Yoon et al. used the Kawase approach for TN associated with DVBA and obtained a good clinical result, except postoperative facial numbness and sixth nerve palsy.[
In the anterior petrosal approach, air cells in the petrosal apex and temporal bone are opened, which may cause postoperative cerebrospinal fluid (CSF) leaks and hearing impairment.[
The ectatic and atherosclerotic basilar artery has muscle memory and recoil and resists displacement. Teflon slings or pledgets are not sufficient to cushion the trigeminal nerve from DVBA compression from a severely ectatic basilar artery.[
This technique and approach should only be considered in cases where compression is caused by severely vertebrobasilar ectasia, to reduce the risk of neurovascular injury and brainstem infarction. Surgeons dedicated and specifically trained in skull base microsurgery are critical for success and avoiding complications.
CONCLUSION
We experienced TN associated with DVBA exclusion. The anterior transpetrosal approach was extremely effective in securing the surgical field, accommodating the transposition, and avoiding perioperative complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Apra C, Lefaucheur JP, Le Guérinel C. Microvascular decompression is an effective therapy for trigeminal neuralgia due to dolichoectatic basilar artery compression: Case reports and literature review. Neurosurg Rev. 2017. 40: 577-82
2. Chai S, Xu H, Wang Q, Li J, Wang J, Wang Y. Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar dolichoectasia: Interposition technique versus transposition technique. Acta Neurochir (Wien). 2020. 162: 2811-21
3. Choudhri O, Connolly ID, Lawton MT. Macrovascular decompression of the brainstem and cranial nerves: Evolution of an anteromedial vertebrobasilar artery transposition technique. Neurosurgery. 2017. 81: 367-76
4. El-Ghandour NM. Microvascular decompression in the treatment of trigeminal neuralgia caused by vertebrobasilar ectasia. Neurosurgery. 2010. 67: 330-7
5. Inoue T, Shitara S, Goto Y, Prasetya M, Fukushima T. Microvascular decompression for trigeminal neuralgia attributable to the vertebrobasilar artery: Decompression technique and significance of separation from the nerve root. Acta Neurochir (Wien). 2021. 163: 1037-43
6. Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. 1967. 26: 159-62
7. Linskey ME, Jho HD, Jannetta PJ. Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar compression. J Neurosurg. 1994. 81: 1-9
8. Niizuma H, Ikeda S, Ohyama H. Trigeminal neuralgia and hemifacial spasm caused by the compression of tortuous vertebro-basilar system-a case report (author’s transl). No Shinkei Geka. 1981. 9: 1167-70
9. Ogawa A, Suzuki M, Shirane R, Yoshimoto T. Repositioning of the tortuous vertebrobasilar artery for trigeminal neuralgia: A technical note. Surg Neurol. 1992. 38: 232-5
10. Petty PG, Southby R. Vascular compression of lower cranial nerves: Observations using microsurgery, with particular reference to trigeminal neuralgia. Aust N Z J Surg. 1977. 47: 314-20
11. Singh H, da Silva HB, Zeinalizadeh M, Elarjani T, Straus D, Sekhar LN. Basilar artery ectasia causing trigeminal neuralgia: An evolved technique of transpositional suture-Pexy, Oper Neurosurg (Hagerstown). 2018. 14: 194-9
12. Tamura R, Tomio R, Mohammad F, Toda M, Yoshida K. Analysis of various tracts of mastoid air cells related to CSF leak after the anterior transpetrosal approach. J Neurosurg. 2019. 130: 360-7
13. Vanaclocha V, Herrera JM, Martínez-Gómez D, RiveraPaz M, Calabuig-Bayo C, Vanaclocha L. Is there a safe and effective way to treat trigeminal neuralgia associated with vertebrobasilar Dolichoectasia? Presentation of 8 cases and literature review. World Neurosurg. 2016. 96: 516-29
14. Yoon S, Mascitelli JR, Mooney MA, Gandhi S, Chen T, Cole TS. Kawase approach for Dolichoectactic basilar artery macrovascular decompression in a patient with trigeminal neuralgia: Case report. Oper Neurosurg (Hagerstown). 2019. 16: E178-83
15. Zaidi HA, Awad AW, Chowdhry SA, Fusco D, Nakaji P, Spetzler RF. Microvascular decompression for hemifacial spasm secondary to vertebrobasilar dolichoectasia: Surgical strategies, technical nuances and clinical outcomes. J Clin Neurosci. 2015. 22: 62-8






Safwat Al-Dineh
Posted December 19, 2022, 11:46 pm
Good article…..
you have opened new perspectives regarding dianosis and treatment of trigeminal neuralgia for me.
Thanks alot…..!