- Department of Neurosurgery, Tokyo General Hospital, Tokyo, Japan
- Department of Neurosurgery, National Defense Medical College, Tokorozawa, Japan,
- Department Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Awfa Aktham, Department of Neurosurgery, Tokyo General Hospital, Nakano, Japan.
DOI:10.25259/SNI_801_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Awfa Aktham1, Shuhei Morita1, Satoru Takeuchi2, Mustafa Ismail3, Samer S. Hoz4, Shinichi Numazawa1, Sadayoshi Watanabe1, Kentaro Mori1. Traumatic rupture of intracranial dermoid cyst with continuous fat droplet migration. 03-Feb-2023;14:39
How to cite this URL: Awfa Aktham1, Shuhei Morita1, Satoru Takeuchi2, Mustafa Ismail3, Samer S. Hoz4, Shinichi Numazawa1, Sadayoshi Watanabe1, Kentaro Mori1. Traumatic rupture of intracranial dermoid cyst with continuous fat droplet migration. 03-Feb-2023;14:39. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12141
Abstract
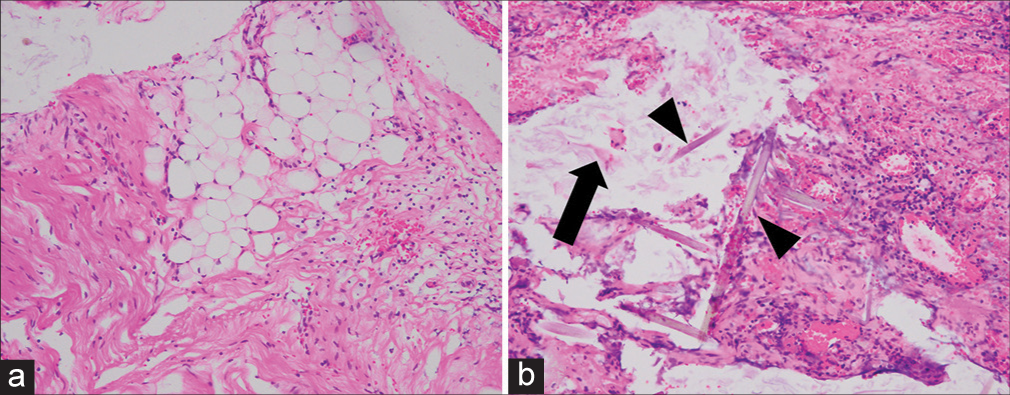
Background: The intracranial dermoid cyst (ICD) can be complicated by rupture and spilling of its contents with potentially dreadful consequences. Head trauma as a predisposing element for this phenomenon is extremely rare. Few reports address the diagnosis and management of trauma-related rupture of ICD. However, there is a pronounced knowledge gap related to the long-term follow-up and the fate of the leaking contents. Here, we present a unique case of traumatic rupture of ICD complicated by continuous fat particle migration within the subarachnoid space with its surgical implications and outcome.
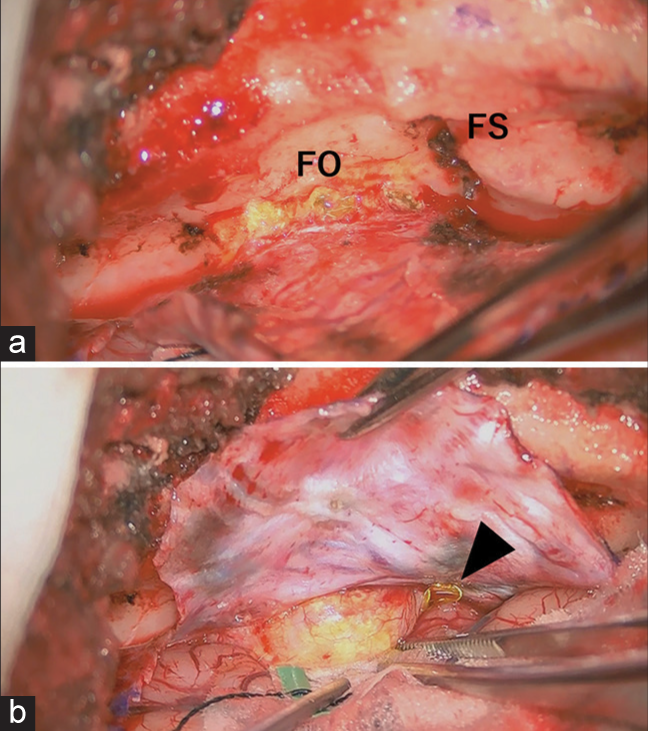
Case Description: A 14-year-old girl had an ICD rupture following a vehicle collision. The cyst was located near the foramen ovale with intra and extradural extensions. Initially, we opted to follow the patient clinically and radiologically as she had no symptoms, and the imaging showed no red flags. Over the next 24 months, the patient remained asymptomatic. However, the sequential brain magnetic resonance imaging revealed significant continuous migration of the fat within the subarachnoid space, with the droplets noticed to increase in the third ventricle. That is considered an alarming sign of potentially serious complications impacting the patient’s outcome. Based on the above, the ICD was completely resected through an uncomplicated microsurgical procedure. On follow-up, the patient is well, with no new radiological findings.
Conclusion: Trauma-related ruptured ICD may have critical consequences. Persistent migration of dermoid fat can be managed with surgical evacuation as a viable option to prevent those potential complications such as obstructive hydrocephalus, seizures, and meningitis.
Keywords: Asymptomatic, Intraventricular fat droplets, Ruptured dermoid, Surgical intervention, Traumatic rupture
INTRODUCTION
Intracranial dermoid cysts (ICD) are infrequent tumor-like ectodermal inclusion cysts.[
CASE SCENARIO
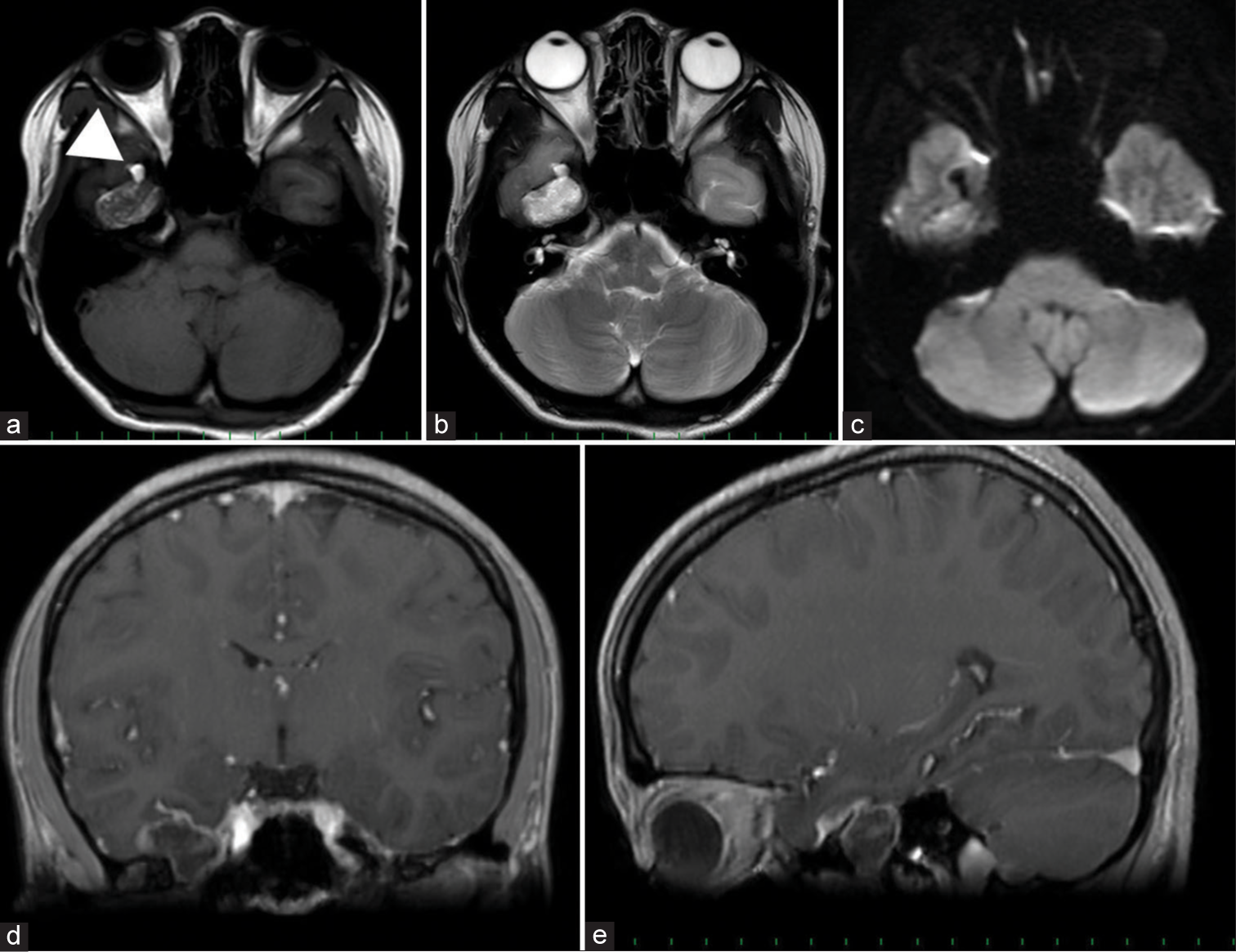
A neurologically intact 14-year-old girl presented to the office; she had post head trauma due to a motor vehicle accident. Her imaging included a brain magnetic resonance imaging (MRI) and head computed tomography scan that showed a right middle cranial fossa mass located near the foramen ovale and extended both intra and extradurally. It appeared restricted on diffusion-weighted imaging with a hypointense signal in T1 and hyperintense in T2, coupled with fat droplet presence in the nearby basal subarachnoid region [
Figure 1:
Initial magnetic resonance imaging MR images show hypointense in T1 (a), hyperintense in T2 (b), with restricted diffusion on DWI (c). Fat droplets in the subarachnoid space nearby the tumor was also noted (arrowhead). (d and e): The coronal and sagittal images with gadolinium shows the slight enhancement of the tumor capsule and also the mass locating both intradurally and extradurally at foramen ovale.
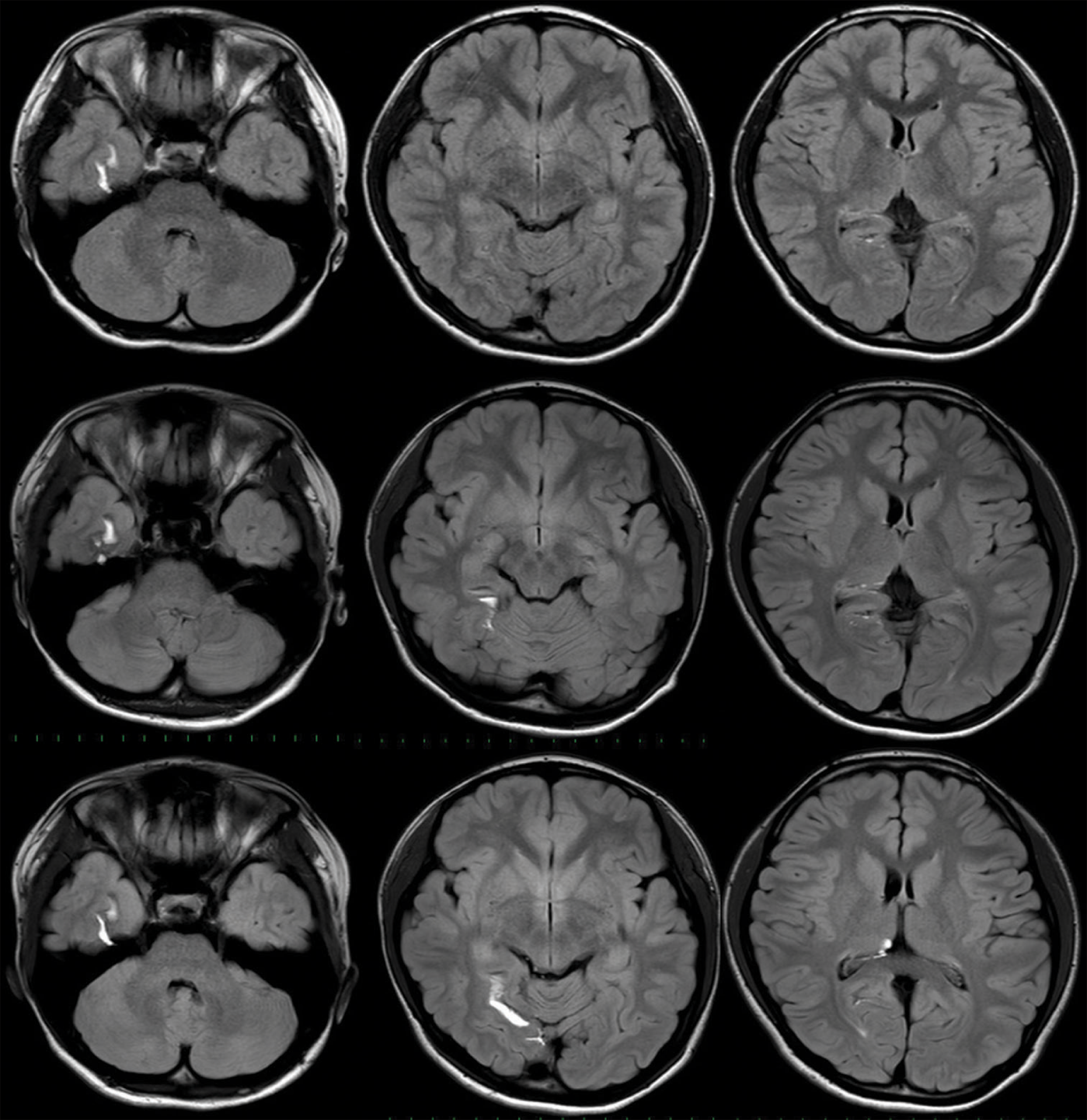
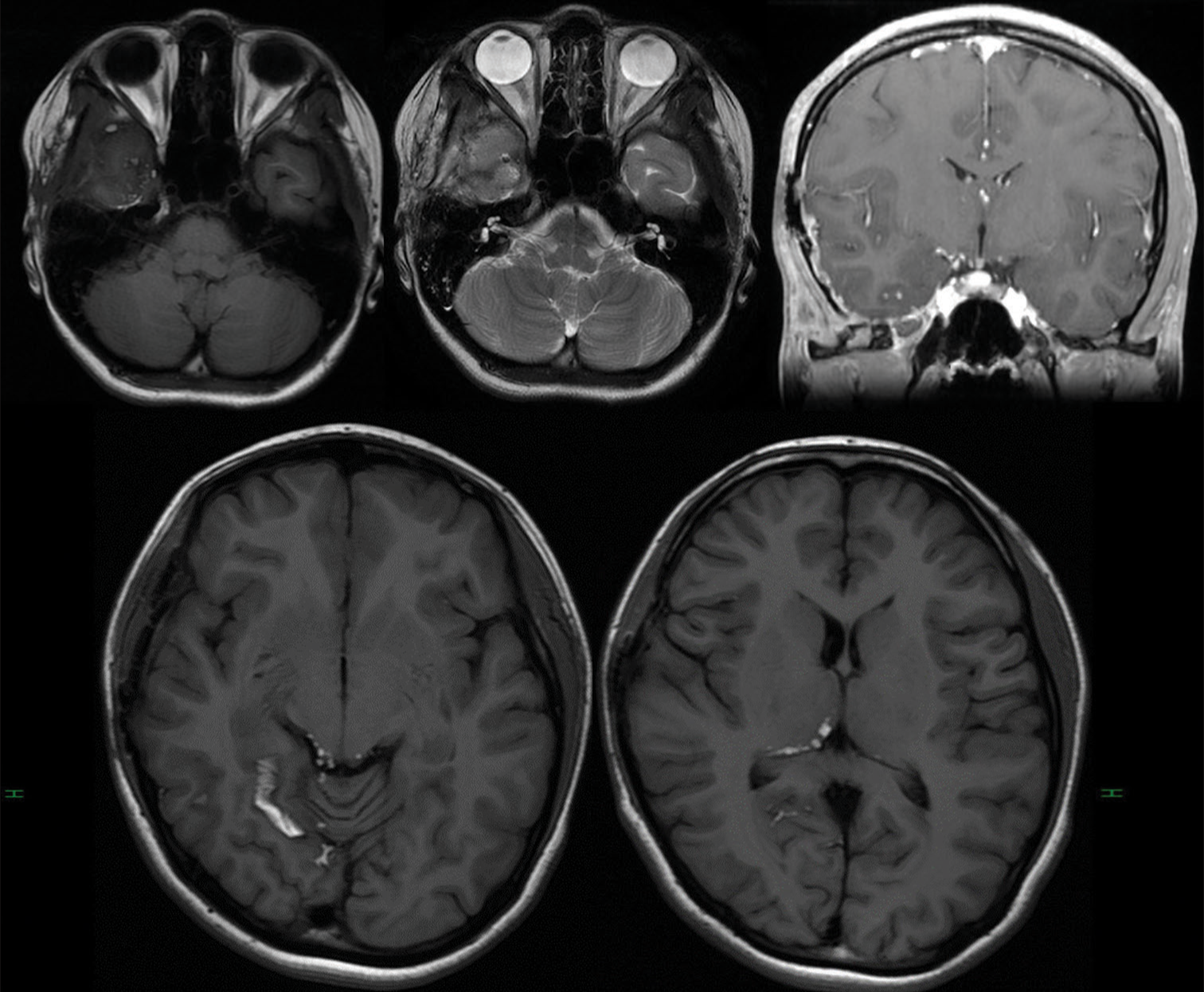
A serial brain MRI [
Figure 2:
Chronological magnetic resonance imaging (MRI) changes in a patient after traumatic rupture of dermoid cyst Upper: The initial MRI showing fat droplets in the adjacent collateral sulcus. Middle: 11 months later, MRI shows migration into the posterior part of the collateral sulcus and quadrigeminal cistern (not shown in this view). Lower: Final MRI showing the fat droplet further migrates into the third ventricle.
DISCUSSION
ICDs, which form between 0.04% and 0.6% of all intracranial neoplasms and are primarily benign congenital inclusion cysts, develop during embryogenesis from ectopically misplaced surface ectoderm.[
Rupture can happen as a result of trauma or less commonly as a result of cyst growth. When the ICD bursts, its contents of cholesterol particles will float in the subarachnoid space and spread widely.[
CONCLUSION
The trauma-related ruptured ICD contents within the intracranial spaces may have critical consequences. Persistent migration of dermoid fat can be managed with surgical evacuation as a viable option to prevent those potential complications such as obstructive hydrocephalus, seizures, and meningitis.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Das U, Pandit N. Traumatic rupture of an intracranial dermoid cyst: A case report. East J Med Sci. 2022. 6: 69-72
2. El-Bahy K, Kotb A, Galal A, El-Hakim A. Ruptured intracranial dermoid cysts. Acta Neurochir (Wien). 2006. 148: 457-62
3. Esquenazi Y, Kerr K, Bhattacharjee MB, Tandon N. Traumatic rupture of an intracranial dermoid cyst: Case report and literature review. Surg Neurol Int. 2013. 4: 80
4. Kim IY, Jung S, Jung TY, Kang SS, Kim TS. Traumatic rupture of an intracranial dermoid cyst. J Clin Neurosci. 2008. 15: 469-71
5. Kosuge Y, Onodera H, Sase T, Uchida M, Takasuna H, Ito H. Ruptured dermoid cyst of the lateral cavernous sinus wall with temporary symptoms: A case report. J Med Case Rep. 2016. 10: 224
6. Liu JK, Gottfried ON, Salzman KL, Schmidt RH, Couldwell WT. Ruptured intracranial dermoid cysts: Clinical, radiographic, and surgical features. Neurosurgery. 2008. 62: 377-84 discussion 384
7. Lunardi P, Missori P, Artico M, Fortuna A. Posttraumatic intradiploic leptomeningeal cyst in an adult: Case report. Surg Neurol. 1991. 35: 475-7
8. Muçaj S, Ugurel MS, Dedushi K, Ramadani N, Jerliu N. Role of MRI in the diagnosis of ruptured intracranial dermoid cyst. Acta Inform Med. 2017. 25: 141-4
9. Osborn AG, Preece MT. Intracranial cysts: Radiologicpathologic correlation and imaging approach. Radiology. 2006. 239: 650-64
10. Park SK, Cho KG. Recurrent intracranial dermoid cyst after subtotal removal of traumatic rupture. Clin Neurol Neurosurg. 2012. 114: 421-4
11. Perdomo-Pantoja A, Zakaria HM, Judy BF, Khalifeh JM, Porras JL, Azad TD. Traumatic sacral dermoid cyst rupture with intracranial subarachnoid seeding of lipid particles: Illustrative case. J Neurosurg Case Lessons. 2021. 2: CASE21355
12. Ramlakhan R, Candy S. Traumatic rupture of an intracranial dermoid cyst. Radiol Case Rep. 2015. 10: 1053
13. Ray MJ, Barnett DW, Snipes GJ, Layton KF, Opatowsky MJ. Ruptured intracranial dermoid cyst. Proc (Bayl Univ Med Cent). 2012. 25: 23-5
14. Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics. 1995. 15: 1437-55
15. Sood S, Gupta R. Susceptibility artifacts in ruptured intracranial dermoid cysts: A poorly understood but important phenomenon. Neuroradiol J. 2014. 27: 677-84
16. Stendel R, Pietila TA, Lehmann K, Kurth R, Suess O, Brock M. Ruptured intracranial dermoid cysts. Surg Neurol. 2002. 57: 391-8
17. Taha A, Abdelrazek MA, Manalo N, Elsadek R, Morrin SJ, Brodski A. Traumatic rupture of a skull base dermoid cyst mimicking chronic meningitis. Cureus. 2022. 14: e25066
18. Wang YM, Chang TP, Lo CP, Tu MC. Spontaneous rupture of intracranial dermoid cyst with chemical meningitis. J Emerg Med. 2013. 44: e275-6
19. Zhang MH, Feng Q, Zhu HL, Lu H, Ding ZX, Feng B. Asymptomatic traumatic rupture of an intracranial dermoid cyst: A case report. World J Clin Cases. 2021. 9: 4046