- Department of Neurosurgery, Cairo University Hospital, Cairo, Egypt,
- Department of Neurosurgery, Punjab Institute of Neurosciences, Lahore General Hospital, Lahore, Pakistan.
Correspondence Address:
Mohammed A. Azab, Department of Neurosurgery, Cairo University Hospital, Cairo, Egypt.
DOI:10.25259/SNI_22_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed A. Azab1, Sajid Iqbal2. Spontaneous acute subdural hematoma as a complication of preeclampsia. A case report and literature review. 03-Mar-2023;14:81
How to cite this URL: Mohammed A. Azab1, Sajid Iqbal2. Spontaneous acute subdural hematoma as a complication of preeclampsia. A case report and literature review. 03-Mar-2023;14:81. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12177
Abstract
Background: Acute subdural hematoma (ASDH) is a common form of intracranial bleeding that may be fatal. Trauma is a major cause, while a subset of cases may occur spontaneously. The authors of this article present a case of spontaneous ASDH in the context of preeclampsia and review similar cases in the literature to identify the prognosis.
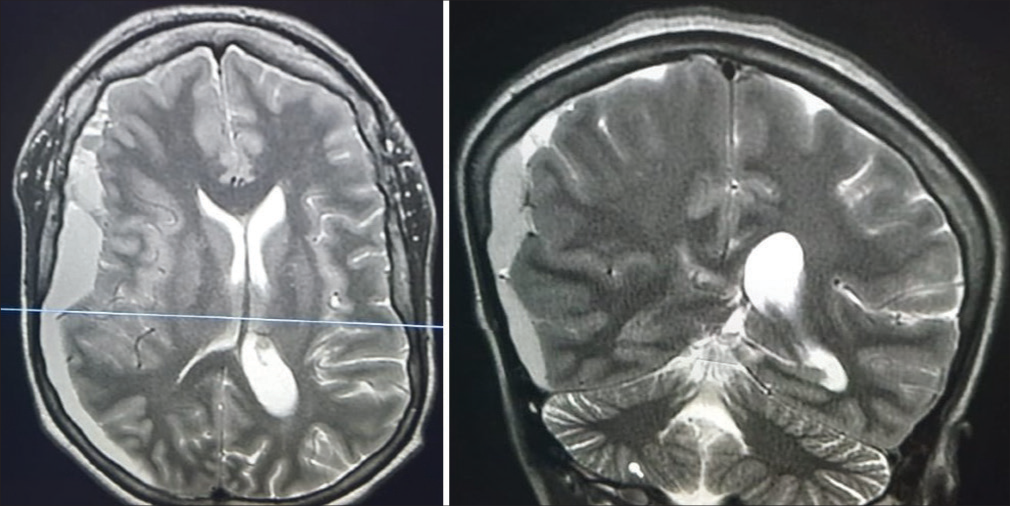
Case Description: A healthy 27-year-old woman presented in her first pregnancy which was complicated with pregnancy-induced hypertension and was sent to a provincial local maternity hospital at 37 weeks of gestation. On day 4 postpartum, the patient complained of severe headache, vomiting and blurred vision. Fundus examination showed papilledema and magnetic resonance imaging showed right acute frontoparietal subdural hematoma. The hematoma was surgically evacuated with decompressive craniotomy. Postoperatively, the patient’s symptoms improved.
Conclusion: Spontaneous ASDH is a rare event in the context of preeclampsia; however, it should be considered as one of its possible complications. Research should be directed to emphasize on the possibility of spontaneous ASDH as a cause of neurological deterioration in those cases. A proper diagnosis and early intervention for these cases are crucial for both the mother and the fetus.
Keywords: Subdural hematoma, Preeclampsia, Pregnancy, Prognosis, Spontaneous
INTRODUCTION
Intracranial hemorrhage as a complication of pregnancy is a rare event that has significant morbidity and mortality. Pregnancy-induced hypertension accounts for about 16% of maternal deaths, although the rate is lower in high-income countries.[
Most cases of intracerebral hemorrhage caused by pregnancy-induced hypertension is caused by a ruptured aneurysm or arteriovenous malformation.[
CASE DESCRIPTION
A healthy 27-year-old woman in her first pregnancy which was complicated with pregnancy-induced hypertension on oral nifedipine was admitted to a provincial local maternity hospital at 37 weeks of gestation. On admission, the patient was fully conscious with the Glascow Coma Scale (GCS) at 15, eye examination revealed bilateral equal reactive pupils, blood pressure was 180/100 mmHg with 4+ proteinuria, no history of convulsions, the patient denied any headache, visual disturbances, or epigastric pain. The cesarean section was performed uneventfully.
During the early postpartum period, she was apparently well and blood pressure was 130/90 mmHg without any other abnormal clinical signs. Platelet count was 250.000, prothrombin time was 12.5 s, and activated partial thromboplastin time was 30 s. Liver enzymes were not elevated and serum creatinine was also normal. On day 4 postpartum, the patient complained of severe headache (intensity 10/10) referred to the whole cranium not responding to analgesia with repeated vomiting and blurred vision. Blood pressure was 160/95 and laboratories were normal. The examination of the eye showed bilateral papilledema. Urgent magnetic resonance imaging brain was done, which showed a right fronto-parietal ASDH as shown in
DISCUSSION
ASDH is the accumulation of acute blood between the dura and the underlying brain. It is considered a common life threatening form of traumatic brain injury. Spontaneous ASDH in pregnancy is uncommon, while it is more commonly caused by trauma or epidural anesthesia in the postpartum period.[
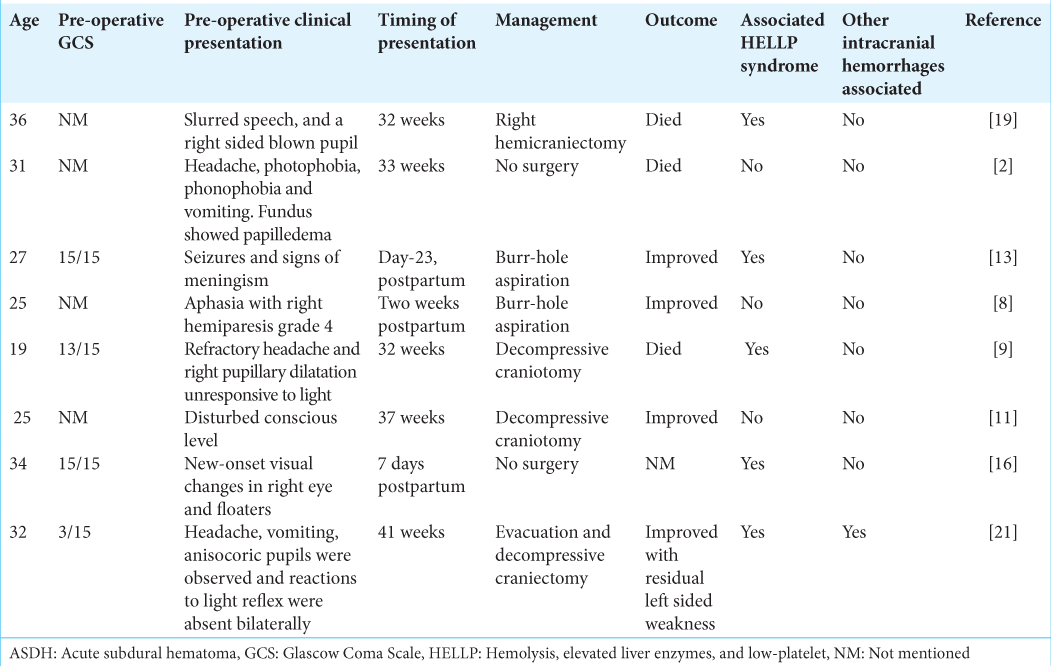
An association between preeclampsia and spontaneous ASDH has not been well established in literature. We highlighted the case reports of spontaneous subdural hematoma in literature
In the acute setting, ASDH management includes either urgent surgical evacuation or conservative management. ASDH more than 10 mm thickness or midline shift more than 5 mm on computed tomography imaging, neurological deterioration, and/or increased intracranial pressure are indications for surgical intervention.[
CONCLUSION
Spontaneous subdural hematoma is a rare event in the context of preeclampsia; however, it should be considered as one of its possible complications. Research should be directed to emphasize on the possibility of spontaneous ASDH as a cause of neurological deterioration in those cases. Proper diagnosis and early intervention for these cases is crucial for both the mother and the fetus.
Ethical approval
Consent was obtained by the patient in this study. King Khalid General Hospital Research Board approved the IRB of this work.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
Dr. Azab has contributed to drafting and manuscript writing. Dr. Sajid has contributed to manuscript editing and final review.
References
1. Amias AG. Cerebral vascular disease in pregnancy. 2-Occlusion. J Obstet Gynaecol Br Commonw. 1970. 77: 312-5
2. Barbosa OA, Correia JW, Lemos PL, De Almeida EJ, Filho AA, de Lima IP. Atraumatic subdural hematoma in preeclampsia with lethal outcome. J Clin Gynecol Obstet North Am. 2015. 4: 191-2
3. Bateman BT, Schumacher HC, Bushnell CD, Pile-Spellman J, Simpson LL, Sacco RL. Intracerebral hemorrhage in pregnancy: Frequency, risk factors, and outcome. Neurology. 2006. 67: 424-9
4. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018. 13: 291-310
5. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW. Surgical management of acute subdural hematomas. Neurosurgery. 2006. 58: S16-24 discussion Si-iv
6. Duley L, Meher S, Abalos E. Management of pre-eclampsia. BMJ. 2006. 332: 463-8
7. El-Sayed AA. Preeclampsia: A review of the pathogenesis and possible management strategies based on its pathophysiological derangements. Taiwan J Obstet Gynecol. 2017. 56: 593-8
8. Gautam S, Meena SC, Gautam B. Spontaneous postpartum subacute subdural hematoma: A case report of probable compilation of eclampsia. Nep J Neurosci. 2016. 13: 109-11
9. Giannina G, Smith D, Belfort MA, Moise KJ. Atraumatic subdural hematoma associated with pre-eclampsia. J Matern Fetal Med. 1997. 6: 93-5
10. Hammoud GM, Ibdah JA. Preeclampsia-induced liver dysfunction, HELLP syndrome, and acute fatty liver of pregnancy. Clin Liver Dis (Hoboken). 2014. 4: 69-73
11. Irie Bi GS, Derou KL, Koffi N, Pete Y, Menin M, Nda-Koffi C. A Rare complication of severe pre-eclampsia: Acute spontaneous subdural haematoma. Analg Resusc Curr Res. 2017. 6: 2
12. Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: A systematic review. Lancet. 2006. 367: 1066-74
13. Patabendige M. Acute subdural haemorrhage in the postpartum period as a rare manifestation of possible HELLP (haemolysis, elevated liver enzymes, and low-platelet count) syndrome: A case report. BMC Res Notes. 2014. 7: 408
14. Ryan CG, Thompson RE, Temkin NR, Crane PK, Ellenbogen RG, Elmore JG. Acute traumatic subdural hematoma: Current mortality and functional outcomes in adult patients at a Level I trauma center. J Trauma Acute Care Surg. 2012. 73: 1348-54
15. Servadei F. Prognostic factors in severely head injured adult patients with acute subdural haematoma’s. Acta Neurochir (Wien). 1997. 139: 279-85
16. Shah FA, Guez G, Patel N, Patel BB. Complicated post-partum HELLP syndrome causing acute renal failure and a spontaneous acute subdural hematoma. Cureus. 2021. 13: e13233
17. Sircar M, Thadhani R, Karumanchi SA. Pathogenesis of preeclampsia. Curr Opin Nephrol Hypertens. 2015. 24: 131-8
18. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Preeclampsia. Lancet. 2010. 376: 631-44
19. Traficante DC, Marin A, Catapano A. Atraumatic subdural hematoma in a third-trimester gravid patient. Case Rep Emerg Med. 2016. 2016: 8252746
20. Vaughan DJ, Stirrup CA, Robinson PN. Cranial subdural haematoma associated with dural puncture in labour. Br J Anaesth. 2000. 84: 518-20
21. Yokota H, Miyamoto K, Yokoyama K, Noguchi H, Uyama K, Oku M. Spontaneous acute subdural haematoma and intracerebral haemorrhage in a patient with HELLP syndrome: Case report. Acta Neurochir (Wien). 2009. 151: 1689-92